Back to Journals » Clinical Ophthalmology » Volume 17
Complementary and Alternative Medicine Use Among Patients with Dry Eye Syndrome in Saudi Arabia: A Survey Study
Authors Aljuhani GA , Afandi R , Alkayyal AA, Alharbi J, Alharbi AS , Alsaedi M, AlHujaili H
Received 14 August 2023
Accepted for publication 13 October 2023
Published 26 October 2023 Volume 2023:17 Pages 3207—3213
DOI https://doi.org/10.2147/OPTH.S435346
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Ghada Awad Aljuhani,1 Rahaf Afandi,2 Aaesha A Alkayyal,2 Jana Alharbi,2 Abeer Surihan Alharbi,3 Mohammed Alsaedi,3 Haneen AlHujaili3
1Ophthalmology department, Saudi Commission for Health Specialties, Madinah, Saudi Arabia; 2Medical Intern, Taibah University, Madinah, Saudi Arabia; 3Ophthalmology Department, Ohud Hospital, Madinah, Saudi Arabia
Correspondence: Ghada Awad Aljuhani, Email [email protected]
Introduction: Complementary and alternative medicine (CAM) includes all healthcare practices that are not part of conventional medicine. One of the most common eye disorders for visiting an ophthalmology clinic is dry eye disease (DED), and due to the increasing number of CAM used for eye conditions, 1 in 5 patients has been reported in previous studies to use CAM for eye treatment. This study aimed to estimate the prevalence of CAM use among patients with (DED).
Methods: A web-based survey was used to collect the data, the first part of the questionnaire was about demographic data, and the second part included a validated Arabic version of the ocular surface disease index (OSDI). The third part was about practices that alleviate DED other than conventional medicine.
Results: The total sample was 282, 61 were males, and 221 were females. Most participants (48.5%) were between 25 and 44 years old, 90% were Saudi, and only 10% were non-Saudi. Of the participant, 70% reported having attained a university or higher education level. The prevalence of the use of CAM among patients with dry eye was around 85%. The most frequently reported type of CAM used among the participants was faith healing (Ruqyah) (41%). This was followed by warm compressors (37%). There was no significant correlation between the severity of OSDI and using CAM, as the p-value was 0.909.
Conclusion: In conclusion, our study shows that CAM is a popular choice among patients with dry eye syndrome. Faith healing and warm compressors are the most used types of CAM. However, the lack of correlation between OSDI severity and CAM use indicates that patients may use CAM for reasons other than symptom severity. Further research is needed to explore the reasons behind CAM use and its effectiveness in managing dry eye syndrome.
Keywords: dry eye, complementary medicine, alternative medicine
Introduction
More than 30% of adults and 12% of children in the United States use healthcare strategies not typically part of conventional medical treatment, referred to as complementary and alternative medicine (CAM), the primary therapeutic types of complementary approaches can be classified as nutritional and psychological (physical) approaches, which include what were referred to as mind and body practices. Although there are indications that some of these products may be beneficial, more information is required regarding the effects of these products on the human body, their safety, and potential interactions with medicines and other natural products.1
Dry eye disease (DES) is a clinical ophthalmic condition affecting about 14% of people over 48. It is characterized by a disorder of the preocular tear film and is relatively common.2
Prevalence of DES in Saudi Arabia may vary between the studies as it ranges from 17 to 50%,3–5 the second most common cause of emergency room visit in Madinah, Saudi Arabia, was DED.6 One of the well-known medical treatments of DED among the population is the over-the-counter artificial tear. However, according to one study, only 64% of the patients with DED were satisfied by over-the-counter medications, and 34% were symptoms relieved.7 Ocular surface disease index (OSDI) questionnaire is a popular tool for evaluating DED symptoms. It has been found to be easy to use, has acceptable repeatability across tests, and has high levels of reliability and validity.8
The use of CAM for ophthalmological causes is on the rise. According to one study in Palestine, two thirds of the eye patients were using CAM,9 while the use of CAM among the population in Saudi Arabia was 21.9%.10
One study done in Australia found that vitamins and herbal medicine were the most prevalent among patients with inflammatory eye disease as non-conventional treatment.11
A large study done in the USA among glaucoma patients showed that only 5% of them used CAM and vitamins on the top list.12 Among the different types of CAM, supplication was found to be the most prevalent for patients with eye disorders in Palestine,9 and in comparison, castor oil was the most used in the Saudi population.10
Some form of CAM has shown to be beneficial acupuncture; for example, it is part of Chinese complementary medicine and was found to alleviate the DES symptomatically and clinically in 88% of the patients.13
Until now, no single study has estimated the prevalence of CAM among patients with dry eye syndrome in Saudi Arabia.
This study aims to know the prevalence and pattern of using CAM among patients with dry eye in Madinah, Saudi Arabia, to inform the public about some harm of these treatments and to establish population-based data for further studies.
Methodology
This study employs a cross-sectional design. Data was collected randomly through an electronic questionnaire that was distributed to participants via a web-based survey platform. The questionnaire included demographic data, an ocular surface disease index (validated Arabic version),14 a section to ask about types of CAM that have been used to alleviate dry eye syndrome that part was used from the questionnaire in previously published study,9 and the questionnaire was available for completion from February 2023 to March 2023.
The study population consisted of adults aged 18–65 who live in Madinah, Saudi Arabia, and get a 13 or more on the OSDI score, OSDI severity was calculated and graded as follows: 0–12 was normal (was removed from the total sample), 13–22 was mild, 23–32 was moderate and 33–100 was severe.8
Data were analyzed using Microsoft Excel version 16.66.1 and was exported to SPSS version 29 for data analysis. Descriptive analysis was used to write the characteristics of the study population and the responses to each question in the questionnaire. Inferential statistics, such as chi-square tests, were used to investigate the relationships between variables of interest, and the chi-square test allowed us to assess the association between two categorical variables by comparing the observed frequencies with the expected frequencies.
This study adhered to the ethical principles in The Declaration of Helsinki on Medical Research involving Human Subjects. Informed consent was taken from all participants before they began the questionnaire. The study protocol was reviewed and approved by the institutional review board and general directorate of health affairs in Madinah. Participants’ privacy and confidentiality were protected throughout the study, and personal identifying information was kept confidential and secure.
Result
As shown in Table 1, most participants (48%) were between the ages of 25 to 44 years old, and only 18% were from 45 to 65 years old.
 |
Table 1 Socio-Demographic Data |
There was a statistically significant relationship between age and using CAM as the P value was 0.21.
Most of our respondents were females (78%).
Nighty percent of them were Saudi.
In our study, 240 of the DED patients (85%) were reported to use at least one type of CAM for the DES.
Fifty percent reported having severe symptoms, according to OSDI, as it is shown in Figure 1. The prevalence of other grades is shown in the same figure as well.
 |
Figure 1 OSDI severity. |
No significant relationship was found between using CAM and the severity of DED, as the p-value was 0.993.
Faith healing (Ruqyah) was the most prevalent type of CAM used among DED patients (41%), followed by warm compressors (37%), and massage therapy was reported by 36%.
Among the vitamins, vitamin D (22%) was the most used to alleviate DED in our study, while among the herbs, tea was the most prevalent use (32%).
Other types are shown in detail in Table 2.
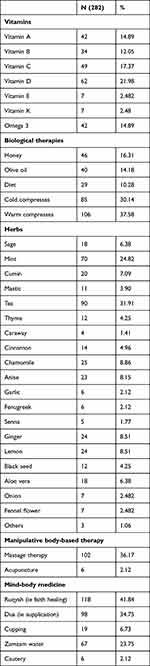 |
Table 2 Types of CAM Used for Dry Eye |
Discussion
As far as we know, this is the first study to assess the use of CAM among patients with dry eye using OSDI to diagnose and grade the severity of DED. Knowing the prevalence and pattern of CAM among DED is crucial for healthcare practitioners as some of the CAM may be beneficial alongside conventional treatment, but some of them may cause harm, interfere with other medications, or have no to little effect.
According to our results, most of the patients (85%) were using CAM to alleviate DED symptoms. There was a significant relationship between age (p = 0.021), marital status (p = 0.031), and monthly income (p = 0.012) among CAM users. Most of the correspondents have severe dry eye, and interestingly there was no significant correlation between the severity and CAM use. Faith healing was the most prevalent type of CAM used to treat DED in our community, followed by warm compressor, massage, and supplication. Older age groups were most likely to use CAM for their DED among our population, as the p-value was 0.021.
Compared to similar research, which was conducted in Palestine, they found a high number of eye patients were using CAM9 (67%), in contrast to a local study in Saudi Arabia, the prevalence was only 22%10, both two previous studies included all eye patients in the calculations. International CAM use was only 5% among glaucoma patients12 and 42% among inflammatory eye diseases.11 All these differences may be due to geographical influence and not to forget to mention the effect of ophthalmological disease on the prevalence of CAM. Locally, castor oil (49%)10 was the most prevalent CAM type among eye patients in Saudi Arabia, in contrast to our finding that faith healing was the most common one among DED patients. Nationally, mind and body therapy were most prevalent among eye patients, like our finding, but supplication (Dua) was the most common one.9 In the USA, megavitamins (62%) were most prevalently used among glaucoma patients,12 again a wide difference perhaps related to cultural effects and type of eye disease. Vitamin D was the most prevalent vitamin to be used for DED in our study compared to omega 3 supplements as most used among patients of eye disease in Palestine.9 Tae was most used in herbal medicine, which was like another national study.9
As mentioned earlier, most of our patients had severe dry eye disease as measured by OSDI, although there was no significant correlation between the degree of severity and whether to use CAM or not; this may lead to speculate other causes that led the patients to use CAM other than the severity, family pressure or norms may be one of the leading causes to use CAM.
Limitation
The low response rate was an obstacle faced during this study, and the high male-to-female ratio was an issue as well that may limit the generalization of the result.
Conclusion
As shown in our findings, CAM use was higher among the DED patients, the most common one was faith healing, and to highlight that there was no significant correlation between using CAM and the severity of DED and which may suggest the patients may have been using the CAM for reasons other than the discomfort and pain, further research is needed to investigate the reasons behind using CAM among dry eye patients and to assess the benefit and harm of these practices.
Funding
There is no funding to report.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Complementary, alternative, or integrative health: what’s in a name? NCCIH. Available from: https://www.nccih.nih.gov/health/complementary-alternative-or-integrative-health-whats-in-a-name.
2. Moss SE, Klein R, Klein BE, Prevalence of and risk factors for dry eye syndrome. Arch Ophthalmol. 2000;118(9):1264–1268. doi:10.1001/archopht.118.9.1264
3. Alshamrani AA, Almousa AS, Almulhim AA, et al. Prevalence and risk factors of dry eye symptoms in a Saudi Arabian Population. Middle East Afr J Ophthalmol. 2017;24(2):67. doi:10.4103/MEAJO.MEAJO_281_16
4. Dossari SK, Alkhars AZ, Albaqshi AA, et al. Prevalence of dry eye disease and its risk factors among the general population of Saudi Arabia: a Cross-Sectional Survey. Cureus. 2022;14(12). doi:10.7759/CUREUS.32552
5. Alkhaldi SA, Allam KH, Radwan MA, Sweeny LE, Alshammeri S. Estimates of dry eye disease in Saudi Arabia based on a short questionnaire of prevalence, symptoms, and risk factors: the Twaiq Mountain Eye Study I. Cont Lens Anterior Eye. 2023;46(2):101770. doi:10.1016/J.CLAE.2022.101770
6. Alabbasi OM, Al-Barry M, Albasri RF, et al. Patterns of ophthalmic emergencies presenting to a referral hospital in Medina City, Saudi Arabia. Saudi J Ophthalmol. 2017;31(4):243. doi:10.1016/J.SJOPT.2016.03.001
7. Nichols KK, Bacharach J, Holland E, et al. Impact of dry eye disease on work productivity, and patients’ satisfaction with over-the-counter dry eye treatments. Invest Ophthalmol Vis Sci. 2016;57(7):2975–2982. doi:10.1167/IOVS.16-19419
8. Schiffman RM, Christianson MD, Gordon Jacobsen F, Hirsch JD, Reis BL. Reliability and validity of the ocular surface disease index. Arch Ophthalmol. 2000;118(5):615. doi:10.1001/archopht.118.5.615
9. Jaber D, Ghannam RA, Rashed W, Shehadeh M, Zyoud SE. Use of complementary and alternative therapies by patients with eye diseases: a hospital-based cross-sectional study from Palestine. BMC Complement Med Ther. 2021;21(1). doi:10.1186/s12906-020-03188-9
10. AlSalman S, AlHussaini MA, Khandekar RB, Edward DP. King Khaled Eye Specialist Hospital, Riyadh, SAU 2. Ophthalmology, College of Medicine, King Saud Medical City, Riyadh, SAU 3. Ophthalmology, King Khalid Eye Specialist Hospital. Ophthalmology. 2021. doi:10.7759/cureus.13109
11. Smith JR, Spurrier NJ, Martin JT, Rosenbaum JT. Prevalent use of complementary and alternative medicine by patients with inflammatory eye disease. Ocul Immunol Inflamm. 2009;12(3):193–204. doi:10.1080/092739490500200
12. Rhee DJ, Spaeth GL, Myers JS, et al. Prevalence of the use of complementary and alternative medicine for glaucoma. Ophthalmology. 2002;109(3):438–443. doi:10.1016/S0161-6420(01)01030-2
13. Tong L, Htoon HM, Hou A, et al. Acupuncture and herbal formulation compared with artificial tears alone: evaluation of dry eye symptoms and associated tests in randomised clinical trial. BMJ Open Ophth. 2018;3(1):150. doi:10.1136/bmjophth-2018-000150
14. Bakkar MM, El-Sharif AK, Al Qadire M. Validation of the Arabic version of the Ocular Surface Disease Index Questionnaire. Int J Ophthalmol. 2021;14(10):1595–1601. doi:10.18240/ijo.2021.10.18
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
