Back to Journals » Clinical Ophthalmology » Volume 11
Comparison of visual acuity, refractive outcomes, and satisfaction between LASIK performed with a microkeratome and a femto laser
Authors Hashmani S, Hashmani N , Rajani H, Ramesh P, Soomro JA, Hussain Shah SR, Kumar J, Mahmood Shah SM
Received 21 March 2017
Accepted for publication 27 April 2017
Published 23 May 2017 Volume 2017:11 Pages 1009—1014
DOI https://doi.org/10.2147/OPTH.S137451
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Sharif Hashmani,1 Nauman Hashmani,1 Hina Rajani,2 Priyanka Ramesh,2 Junaid Ahmed Soomro,2 Syed Rashid Hussain Shah,2 Jaish Kumar,2 Sayed Mustafa Mahmood Shah2
1Department of Ophthalmology, Hashmanis Hospital, Karachi, Pakistan; 2Dow Medical College, Karachi, Pakistan
Purpose: To compare refractive outcomes, visual acuities, and satisfaction of patients between those treated with laser-assisted in situ keratomileusis (LASIK) using a Hansatome microkeratome (HM) and femto-assisted laser (FAL).
Methods: This was a retrospective analysis of 1,366 eyes in 687 patients who underwent LASIK with an HM (n=1,137) and an FAL (n=229) at the two centers of Hashmanis Hospital, Karachi, Pakistan. Refractive outcomes, including sphere, cylinder, and spherical equivalent in diopters (D), and visual acuities were assessed both preoperatively and at 1 month follow-up. Patient satisfaction was gauged by contacting the patient at the time of chart review.
Results: The postoperative median sphere, cylinder, and spherical equivalent values for those treated with FAL were 0.3±0.7 (-5.5–1.8), -0.5±0.6 (-5.0–1.0), and 0.0±0.7 (-6.0–1.6), respectively. For the HM arm, they were 0.0±1.28 (-10.8–6.8), -0.5±0.5 (-4.5–1.5), and -0.3±1.3 (-11.6–6.8), respectively. All preoperative values were statistically insignificant between the groups, while postoperative values were significant with P-values <0.001. Predictability and efficacy index was higher for the FAL (92.1%, 1.00) than the HM group (82.2%, 0.84). Similarly, patient satisfaction was slightly higher for those treated with FAL (93.3%) than HM (91.4%).
Conclusion: Our large retrospective analysis of eyes that have undergone LASIK using HM and FAL shows superior refractive outcomes in the latter, with special regard to procedural efficacy and predictability.
Keywords: laser-assisted in situ keratomileusis, femtosecond, microkeratome, cornea, refractive surgery
Introduction
Recently, the global prevalence of myopia has been shown to be on the increase, worldwide.1 According to current trends, the international myopic burden is set to boom, with 4,578 million people or approximately half of the world population expected to be victims of this disorder.2 In Pakistan, the prevalence of myopia among the adult population was found to be 36.5%.3
The dynamic and multifaceted development of myopia in the region, coupled with technological advances over time, has led to the growing utilization of contemporary avenues of treatment for this disorder. Refractive surgery, particularly laser-assisted in situ keratomileusis (LASIK), has shown promising results in this regard.4,5
With the advent of Femto-LASIK, superior refractive outcomes in patients have been reported,6 but not all researchers agree. Some show superior outcomes with the former,7–10 others favor the use of a microkeratome,11 and a few show no significant differences in either of the treatment modalities.12,13
This large-scale retrospective study compares the refractive outcomes following two distinct LASIK modalities in a large cohort of patients. To date, most studies comparing outcomes of LASIK with a Hansatome microkeratome (HM) and femto-assisted laser (FAL) have been conducted in western, developed countries7,14 and have often compared outcomes in small sample sizes with limited refractive ranges.12,13,15 To the best of our knowledge, this is the only study to assess the large-scale refractive outcomes of two distinct LASIK techniques in this region and one of the only in the world to include a wide range of refractive errors.
Methods
Patients
Thousand three-hundred sixty-six individual eyes of 687 patients were enrolled in this retrospective study, including 272 males and 415 females. Of this cohort, 1,137 eyes were treated with an HM and 229 with an FAL. The study period was from January 2013 to August 2016. All surgeries were conducted at the two centers of Hashmanis Hospital in Karachi, Pakistan. Three different surgeons took part in the HM group, while there was a single surgeon in the FAL cohort. Ethical approval for this retrospective study was granted by the Ethics Committee of the Hashmanis Hospital. Additionally, written informed consent for the surgery and inclusion in this study was obtained from all patients.
Inclusion/exclusion criteria
Prior to treatment, all individuals were assessed according to the study’s inclusion/exclusion criteria. Individuals older than 18 years with a stable refraction, a central corneal thickness (CCT) greater than 480 μm, a presumed residual stromal bed of >250 μm, and discontinued soft contact use for at least 1 week were deemed eligible. Informed consent was sought from all such individuals prior to surgery. Those with any ocular pathology, either active or residual, retinal pathologies including dystrophies or diabetic retinopathy, dry eyes with a Schirmer’s test II value of less than 2 mm, and those who were immunocompromised, nursing, or pregnant were excluded.
Prior to surgery, all patients underwent routine examinations including uncorrected visual acuity (UCVA), best-corrected visual acuity (BCVA), cycloplegic and subjective refractive error, slit-lamp examination, dilated retinal exam, ultrasonic pachymetry, keratometry, and corneal topography.
LASIK procedure and postoperative care
We performed surgeries in both eyes using the same procedure. Both surgeries were performed using the wavelight EX 500 machine (Alcon, Ft Worth, TX, USA), which was wavefront optimized. An HM (Bausch & Lomb, Rochester, NY, USA) was used to create flaps in one group, while a wavelight FS 200 Laser machine (Alcon) was employed in the other group undergoing LASIK with an FAL. We measured the CCT on the apex of the cornea, preoperatively. Then, once the flap was created, a second measurement was taken to calculate the thickness of the underlying stroma intraoperatively. In both instances, the Pocket II ultrasonic pachymeter (Quantel Medical, Inc., Bozeman, MT, USA) was used. A 140 μm and 120 μm flap was used in the HM and FAL groups, respectively. In those under FAL, a tissue separator was used to raise the flap, and in both arms, a balanced salt solution was used to irrigate the eye once the flap was placed back after the procedure.
Following surgery, these postoperative measures were employed: artificial tears 4 times a day for 3 weeks; moxifloxacin eye drops 4 times a day for 10 days; and combination drops with tobramycin and dexamethasone 4 times a day for 10 days.
Patients were followed up at 1 month postoperatively to review refractive outcomes including UCVA, spherical equivalent (SE), and sphere and cylinder values. The target refractive outcome was emmetropia in all patients that was either greater than −12.00 diopters (D) or less than 4.00 D. For those exceeding this value, the target was the refractive error subtracted from these values. The target outcome in both instances was dependent on the keratometry reading. Accordingly, procedural efficacy index was calculated as the proportion of the mean postoperative UCVA to the mean preoperative BCVA. Predictability was defined as percentage of eyes achieving mean SE within ±1.00 D.
Patient satisfaction
Patients were surveyed at the time of chart review and asked to rate their LASIK experience in the following classes: extremely satisfied, very satisfied, satisfied, and not satisfied.
Statistical analysis
AppSheet was used to enter data into Google Sheet from which the data were subsequently imported into SPSS 16.0 (SPSS Inc., Chicago, IL, USA). All subsequent analysis was done on this software. Descriptive statistics was used to calculate the median and standard deviation of all values; median values were used, as these data were not normally distributed. The Mann–Whitney U test was used to compare the sphere, cylinder, and SE between the two modalities. Graphs were constructed using SPSS and Microsoft Excel (Microsoft Corp., Redmond, WA, USA).
Results
Of the 1,366 eyes (687 patients) treated, 1,137 (570 patients) were in the HM group and 229 (117 patients) in the FAL. The mean age of patients in both groups was 25±5.8 and 27.0±7.3 years (Table 1), respectively.
  | Table 1 Preoperative data |
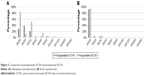
Preoperative parameters included: sphere values of −4.3±2.8 D and −4.3±2.3 D; cylinder values of −1.0±1.0 D and −1.0±1.3 D; and SE values of −4.5±2.8 D and −4.5±2.5 D, among the HM and FAL groups, respectively (Table 1). No statistically significant difference existed in any of these values. Figure 1 displays the preoperative and postoperative astigmatism of the two treatment modalities. Figure 2, on the other hand, shows the predicted versus the achieved SE.
  | Figure 1 Comparison of astigmatism. |
  | Figure 2 Comparison of attempted and achieved SE. |
Postoperatively, the refractive outcomes for HM and FAL included: sphere values of 0.0±1.28 and 0.3±0.7; cylinder values of −0.5±0.5 and −0.5±0.6; and SE values of −0.3±1.3 and 0.0±0.7, respectively (Table 2). All differences in postoperative values were found to be statistically significant with P-values <0.001 (Table 2).
  | Table 2 Postoperative data |
It was found that the FAL group yielded the most uniform outcomes in visual acuity, as almost all achieved a postoperative UCVA of 20/20 (Figure 3), with a corresponding efficacy index of 1.00. This is in contrast with those in HM, which yielded a somewhat lower efficacy index of 0.84.
The postsurgical refractive outcomes demonstrated good predictability (Figure 4), with 92.1% of eyes that had undergone FAL achieving a mean SE within 1.00 D of the intended value. The same was achieved in 82.2% of eyes treated with an HM.
  | Figure 4 Comparison of refractive outcomes. |
Slightly more patients (93.3%) reported an overall level satisfaction in the FAL cohort, compared to HM (91.4%) (Table 3). The combined patient satisfaction rate was 91.8% for both procedures. 61.4% of patients were available for judging patient satisfaction in the HM and 64.1% in the FAL.
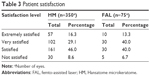  | Table 3 Patient satisfaction |
Discussion
Our study measured refractive outcomes across 1,366 eyes, of which a majority underwent LASIK with an HM (n=1,137) and the remainder with an FAL (n=229). The median age of patients in each treatment group was 25.0±5.8 and 27.0±7.3, which may be reflective of the increasing myopic burden among younger individuals.16–18 Moreover, the preoperative data was similar for both the groups as indicated by the insignificant P-values.
The FAL cohort had significantly superior outcomes in two refractive domains: cylinder and SE (P<0.01). Sphere, on the other hand, showed better values in the HM group. This corresponded to a greater efficacy index among eyes treated with the FAL (n=1.00), compared with the HM (n=0.84). These results are consistent with Montes Mico et al’s7 findings, where efficacy index for eyes treated with an FAL and a microkeratome were 1.07 and 1.00, respectively. Superior postoperative UCVA outcomes in eyes that have undergone FAL over microkeratome have been documented in other studies as well.9,10 Pajic et al,15 in a prospective, randomized, and paired-eye study, also reported a lower efficacy index among eyes treated with microkeratome. However, significant differences in visual acuity between the two groups were only seen till the end of the first postoperative week as the delay in visual recovery in eyes treated with a microkeratome was attributed to a minimal interface fluid accumulation.15 Our study, with a longer postoperative follow-up, shows a greater efficacy index in FAL at 1 month.
Interestingly, the aforementioned study correlated the lower efficacy index of eyes treated with microkeratome to the deviation in achieved versus intended flap thickness.15 Several studies have shown that flaps produced using Femto-LASIK are more predictable, thinner, and have a favorable planar shape.19–22 However, it is unclear whether the desirable flap properties translate into superior visual outcomes. Xia et al8 found no significant differences in UCVA or BCVA in eyes treated with FAL or a mechanical microkeratome at any time postoperatively, despite achieving superior flap dimensions in the former group. Likewise, no significant differences in visual outcomes between the two flap cutting modalities were reported by Hashimoto et al12 or Patel et al13 in two separate randomized, controlled, paired-eye studies. However, the latter study reported greater flap thickness in eyes treated with Femto-LASIK, instead of blade LASIK, although the difference was not significant. One study was found to report a greater procedural efficacy in eyes treated with microkeratome LASIK over Femto LASIK.11
Given the uncertainty surrounding the subject matter, meta-analyses have been conducted by Zhang et al14 and Chen et al23 to evaluate refractive outcomes of the two modalities. Neither of these reported any significant differences in efficacy, although a better predictability was documented by Chen et al.23 In addition, both had conflicting reports on the prevalence of higher-order aberrations (HOAs) with Zhang et al14 reporting significantly fewer HOAs in eyes that have undergone FAL, and Chen et al23 reporting no significant differences in either group.
In our setting, eyes treated with FAL showed a greater procedural predictability of 92.1%, as opposed to 82.2% predictability of eyes treated with LASIK using an HM. These findings are consistent with those of other studies,7,23–25 and may be reflective of faster visual recoveries associated with Femto-LASIK.24
Our study also assessed the reported satisfaction levels of patients postoperatively. It was found that both treatment modalities were received with high levels of satisfaction (Table 3): 91.4% reported satisfaction in the HM group and 93.3% in the FAL cohort. Similar high levels have also been reported in a previous study.26
Limitations
This was a retrospective, observational study, and so all limitations associated with such methods apply. Additionally, our study was confined to the assessment of refractive outcomes following surgery, and we could not evaluate other pertinent outcomes like HOAs or contrast sensitivity. Also, our study did not report the flap thicknesses achieved with either treatment modality. Finally, we only had a 1 month follow-up and therefore cannot comment on the long-term effects of the procedure.
We recommend performing prospective studies where one surgeon performs surgeries on both modalities to get a more direct comparison. Such a model will account for any changes based on the skill of the surgeon.
Conclusion
We reported superior refractive outcomes in LASIK performed with an FAL as compared to one with an HM. Femto-LASIK also showed greater procedural efficacy and predictability in this large cohort of Pakistani patients. Additionally, slightly higher levels of patient satisfaction were reported in the FAL group.
Acknowledgment
We would like to thank Dr Azfar Nafees and Dr Khaliq ur Rehman for providing their surgical data for use in this study.
Disclosure
The authors report no conflicts of interest in this work.
References
Pan CW, Ramamurthy D, Saw SM. Worldwide prevalence and risk factors for myopia. Ophthalmic Physiol Opt. 2012;32(1):3–16. | ||
Holden BA, Fricke TR, Wilson DA, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123(5):1036–1042. | ||
Shah SP, Jadoon MZ, Dineen B, et al. Refractive errors in the adult pakistani population: the national blindness and visual impairment survey. Ophthalmic Epidemiol. 2008;15(3):183–190. | ||
Pillar A, Krueger R. Advances in refractive surgery: June 2014 to July 2015. Asia Pac J Ophthalmol. 2016;5(3):212–222. | ||
Solomon KD, Fernandez de Castro LE, Sandoval HP, et al. LASIK world literature review: quality of life and patient satisfaction. Ophthalmology. 2009;116(4):691–701. | ||
Huhtala A, Pietila J, Makinen P, Uusitalo H. Femtosecond lasers for laser in situ keratomileusis: a systematic review and meta-analysis. Clin Ophthalmol. 2016;10:393–404. | ||
Montes-Mico R, Rodriguez-Galietero A, Alio JL. Femtosecond laser versus mechanical keratome LASIK for myopia. Ophthalmology. 2007;114(1):62–68. | ||
Xia LK, Yu J, Chai GR, Wang D, Li Y. Comparison of the femtosecond laser and mechanical microkeratome for flap cutting in LASIK. Int J Ophthalmol. 2015;8(4):784–790. | ||
Durrie DS, Kezirian GM. Femtosecond laser versus mechanical keratome flaps in wavefront-guided laser in situ keratomileusis: prospective contralateral eye study. J Cataract Refract Surg. 2005;31(1):120–126. | ||
Tanna M, Schallhorn SC, Hettinger KA. Femtosecond laser versus mechanical microkeratome: a retrospective comparison of visual outcomes at 3 months. J Refract Surg. 2009;25(Suppl 7):S668–S671. | ||
AlArfaj K, Hantera MM. Comparison of LASEK, mechanical microkeratome LASIK and Femtosecond LASIK in low and moderate myopia. Saudi J Ophthalmol. 2014;28(3):214–219. | ||
Hasimoto AR, Gomes MF, de Siqueira MA, Moreira H. [Femtosecond laser versus mechanical microkeratome for LASIK flap creation]. Arquivos Bras Oftalmol. 2013;76(6):335–338. | ||
Patel SV, Maguire LJ, McLaren JW, Hodge DO, Bourne WM. Femtosecond laser versus mechanical microkeratome for LASIK: a randomized controlled study. Ophthalmology. 2007;114(8):1482–1490. | ||
Zhang ZH, Jin HY, Suo Y, et al. Femtosecond laser versus mechanical microkeratome laser in situ keratomileusis for myopia: metaanalysis of randomized controlled trials. J Cataract Refract Surg. 2011;37(12):2151–2159. | ||
Pajic B, Vastardis I, Pajic-Eggspuehler B, Gatzioufas Z, Hafezi F. Femtosecond laser versus mechanical microkeratome-assisted flap creation for LASIK: a prospective, randomized, paired-eye study. Clin Ophthalmol. 2014;8:1883–1889. | ||
Bar Dayan Y, Levin A, Morad Y, et al. The changing prevalence of myopia in young adults: a 13-year series of population-based prevalence surveys. Invest Ophthalmol Vis Sci. 2005;46(8):2760–2765. | ||
Lee YY, Lo CT, Sheu SJ, Lin JL. What factors are associated with myopia in young adults? A survey study in Taiwan Military Conscripts. Invest Ophthalmol Vis Sci. 2013;54(2):1026–1033. | ||
Abdullah AS, Jadoon MZ, Akram M, et al. Prevalence of uncorrected refractive errors in adults aged 30 years and above in a rural population in Pakistan. J Ayub Med Coll Abbottabad. 2015;27(1):8–12. | ||
Ahn H, Kim JK, Kim CK, et al. Comparison of laser in situ keratomileusis flaps created by 3 femtosecond lasers and a microkeratome. J Cataract Refract Surg. 2011;37(2):349–357. | ||
Prakash G, Agarwal A, Yadav A, et al. A prospective randomized comparison of four femtosecond LASIK flap thicknesses. J Refract Surg. 2010;26(6):392–402. | ||
Sutton G, Hodge C. Accuracy and precision of LASIK flap thickness using the IntraLase femtosecond laser in 1,000 consecutive cases. J Refract Surg. 2008;24(8):802–806. | ||
Zhou Y, Zhang J, Tian L, Zhai C. Comparison of the Ziemer FEMTO LDV femtosecond laser and Moria M2 mechanical microkeratome. J Refract Surg. 2012;28(3):189–194. | ||
Chen S, Feng Y, Stojanovic A, Jankov MR 2nd, Wang Q. IntraLase femtosecond laser vs mechanical microkeratomes in LASIK for myopia: a systematic review and meta-analysis. J Refract Surg. 2012;28(1):15–24. | ||
Stonecipher K, Ignacio TS, Stonecipher M. Advances in refractive surgery: microkeratome and femtosecond laser flap creation in relation to safety, efficacy, predictability, and biomechanical stability. Curr Opin Ophthalmol. 2006;17(4):368–372. | ||
Kezirian GM, Stonecipher KG. Comparison of the IntraLase femtosecond laser and mechanical keratomes for laser in situ keratomileusis. J Cataract Refract Surg. 2004;30(4):804–811. | ||
Eydelman M, Hilmantel G, Tarver M, et al. Symptoms and Satisfaction of Patients in the patient-reported outcomes with laser in situ keratomileusis (PROWL) studies. JAMA Ophthalmol. 2017;135(1):13–22. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.