Back to Journals » Clinical Ophthalmology » Volume 16
Comparison of Time-to-Surgery and Outcomes in Transferred Vs Non-Transferred Open Globe Injuries
Authors Fernandez EO , Miller HM, Pham VQ, Fleischman D
Received 16 June 2022
Accepted for publication 1 August 2022
Published 22 August 2022 Volume 2022:16 Pages 2733—2742
DOI https://doi.org/10.2147/OPTH.S378049
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Elise O Fernandez,1 Hannah M Miller,2 Vincent Q Pham,3 David Fleischman2
1School of Medicine, University of North Carolina, Chapel Hill, NC, USA; 2Department of Ophthalmology, University of North Carolina, Chapel Hill, NC, USA; 3College of Medicine, Northeast Ohio Medical University, Rootstown, OH, USA
Correspondence: David Fleischman, Department of Ophthalmology, University of North Carolina, 5126 Bioinformatics Bldg #7040, Chapel Hill, NC, 27599-7040, USA, Tel +1 919 966-5296, Fax +1 919 966-1908, Email [email protected]
Purpose: It is widely accepted in the field of ophthalmology that closure of open globes within 24 hours of the injury results in the best visual outcomes. This study investigates the time-to-surgery and visual outcomes of open globe injury patients in North Carolina that were transferred to our institution before receiving surgical intervention as compared to those that were not transferred.
Patients and methods: This is a retrospective cohort study using data from UNC Hospitals trauma registry. Demographics, time of injury, final clinical outcomes, time to surgical intervention, and transfer history were extracted and analyzed. The study population includes open globe injury patients of all ages that were seen and treated at our institution from 2005 to 2020. Patients were divided based on transfer history. The transfer group consisted of patients who were transferred from an outside hospital to our tertiary care facility for surgical treatment. The non-transfer group consisted of patients who arrived at our tertiary care facility directly after injury.
Results: In total, 238 open globe injuries were evaluated. Of those, 197 were transferred and 41 were not transferred. Compared to non-transfer patients, transfer patients had longer delays between injury and surgery, between presentation at the initial ED and surgery, and between injury and arrival at the tertiary care center. On average, the delay between injury and surgical intervention was 3 hours and 51 minutes longer for transfer patients compared to non-transfer patients. Eight patients in the transfer group were delayed > 24 hours due to inter-hospital transfer. Additionally, transfer patients on average suffered from poorer final visual acuities, with an average final visual acuity of 1.84 logMAR in the transfer group and 1.35 logMAR in the non-transfer group.
Conclusion: Our study found that inter-hospital transfer leads to significant delays in primary closure of open globe injuries. Injuries that were transferred to a tertiary care center before receiving surgical intervention on average resulted in worse final visual acuities.
Keywords: eye injury, open globe injury, ocular trauma, surgery, visual outcomes, transfer
Background
Ocular trauma due to eye injuries continues to be a significant cause of permanent vision damage and vision loss in the United States.1 The incidence of open globe injury in the US is estimated to be 4.49 injuries per 100,000 population.2 While advancements in the management of ocular trauma have greatly improved patient outcomes, there continue to be controversies over the timing of surgical intervention in the setting of ocular injury.3
Open globe injuries are a severe form of ocular trauma involving full-thickness disruption of the eyewall.4 Patients with open globe injuries require urgent evaluation by an ophthalmologist, and therefore, may need to be transferred to a Level I or II trauma center.5 The visual outcomes of an open globe injury rely on a wide variety of prognostic factors. Previous studies have investigated risk factors that determine final visual acuity and the development of complications, such as endophthalmitis and retinal detachment. Some risk factors that have been associated with worse prognosis include poor visual acuity at presentation, mode and setting of injury, ocular trauma score, zone of injury, presence of an intraocular foreign body (IOFB), endophthalmitis, and time elapsed between injury and primary wound closure.6–16 Knowledge of these risk factors can help physicians predict patient recovery and guide important management decisions. It is well known that delaying surgical intervention by more than 24 hours increases the risk of endophthalmitis7,8,11–14 and reduced final visual acuity.9,10,15,16 In general, it has been determined that rapid surgical closure of an open globe injury promotes the best visual outcomes, and it is recommended that all open globe injuries be closed within 24 hours of injury.5
Patients with open globe injuries are frequently transferred from community-based facilities to larger tertiary care hospitals for surgical intervention. Our institution is an academic tertiary care center that frequently receives transferred open globe patients from rural facilities with limited access to ophthalmologic care. The process of receiving, evaluating, and transferring a patient from an outside facility for definitive care inevitably results in a delay to surgical closure. While some of the effects of delaying globe repair by more than 24 hours have been investigated in prior studies, the effects of delaying closure by up to 24 hours are still unclear.
The purpose of this study was two-fold: (1) to determine the average delay in time between injury and primary repair of open globe patients that are transferred to a second trauma center before receiving surgical treatment as compared to patients that are not transferred, (2) to determine the final visual outcomes and incidence of postoperative complications in open globe injury patients that are transferred to a second trauma center for surgical repair as compared to patients that are not transferred.
Methods
This was a retrospective cohort study of all open globe injuries received by the University of North Carolina Medical Center Emergency Department (UNC ED) from January 2005 to December 2020. Subjects were identified using data provided by the UNC Hospital Trauma Registry, all acquired data was protected and anonymized to maintain patient data confidentiality. Subjects were divided into two groups by transfer history: transfer and non-transfer. The transfer group included subjects who presented to an outside emergency department (ED) before being transferred to our academic center and surgically treated by the ophthalmology department. The non-transfer group included subjects who presented directly to our institution without being transferred from an outside hospital (OSH). This study was approved by the UNC Institutional Review Board (21-0165) and was completed in accordance with the ethical standards of the Declaration of Helsinki. The study received approval from the IRB to waive informed consent given the research involved no more than minimal risk to subjects.
Review of the subjects’ medical records included ED admission notes, ophthalmology consult notes, primary and subsequent surgical notes, and outpatient follow-up notes. The data collected during chart review included demographics (age, gender, county of residence, insurance coverage), ocular and medical history, information on the referring facility, reason for transfer (if available), transfer times, time of injury and surgery, injury type and mechanism, presence of an IOFB, zone of injury (ZOI), ocular trauma score (OTS), initial visual acuity (VA), surgical procedures performed, and outcomes (final VA, additional surgeries needed, and enucleation). Visual acuity calculations were made using the logMAR scale with the following values assigned to the lowest visual acuities: anophthalmic or NLP (no light perception) − 3, LP (light perception) − 2.8, HM (hand motion) − 2.3, CF (count fingers) − 1.85.17–19
The ZOI was defined based on the anatomic location of the rupture or laceration. Zone 1 injuries involved the cornea and/or limbus, zone 2 injuries involved the area of the sclera within 5 mm of the limbus, and zone 3 injuries involved the sclera further than 5 mm from the limbus.5 The OTS was recorded from the subject’s medical record or calculated using the formula proposed by Kuhn et al that takes into consideration the following variables: initial VA, rupture, endophthalmitis, perforating injury, retinal detachment, and afferent pupillary defect.20 An OTS of 1 indicates the highest level of severity, while an OTS of 5 indicates the lowest level of severity.
The study group included a mix of isolated and non-isolated open globe injuries. Other associated injuries included subconjunctival hemorrhage, hyphema, traumatic cataract, intraocular foreign body, dislocated lens, retinal detachment, vitreous hemorrhage, eyelid laceration, facial laceration, orbital fracture, nasal fracture, cerebral contusion, and trauma to other areas of the body.
Referring Facilities and Reasons for Transfer
The name, trauma level, and number of patients sent were recorded for each referring facility, as well as the distance in miles from the referring facility to our emergency department. Official representatives of each facility were contacted by the study team to determine: (i) whether the ED had ophthalmologists on call, (ii) the number of ophthalmologists providing coverage for hospital consultations, and (iii) the hours of ophthalmology coverage. We were able to obtain the reasons for transfer to our institution through the transfer notes, however, not all transfer notes contained this information.
Time to Surgical Intervention and Transfer Times
For each subject, four different time intervals were calculated between the time of injury, the time of presentation at the ED, the time of presentation at our institution, and the time of surgery. Additionally, three time intervals were calculated only for the transfer subjects, these included: (i) average time from initial presentation at the OSH to initiation of transit to the academic center, (ii) average transit time between facilities, and (iii) average time from presentation at the OSH to presentation at the academic center. Subjects were excluded if they did not present to the ED within 24 hours of their injury, if they did not undergo primary repair of their open globe within 24 hours of arrival at our department due to the need to perform a more urgent non-ophthalmic surgery first, or if their chart did not have sufficient information on time of injury, presentation, or surgery. In total, 114 subjects were excluded. A detailed diagram of the inclusion and exclusion of subjects for the evaluation of time to surgical intervention and transfer times can be found in Figure 1.
Vision and Ocular Outcomes
The following variables were measured to assess visual and ocular outcomes: final VA, number of additional surgeries needed, and incidence of enucleation or evisceration. Before comparing visual outcomes, OTS, ZOI, and prevalence of IOFBs in each group were compared using a Mann Whitney U-test to ensure there was no statistically significant difference in injury type or severity between the transfer and non-transfer subjects. Subjects were excluded if their OTS or ZOI were unidentifiable, if they were lost to follow-up within the first 2 months after surgical repair and did not undergo enucleation during that time, if their chart did not have sufficient information on the time of injury, or if surgical closure was not possible due to the extent of the injury resulting in immediate enucleation. In total, 97 subjects were excluded. A detailed diagram of the inclusion and exclusion of subjects for the evaluation of vision and ocular outcomes can be found in Figure 2.
Statistical Methods
The time intervals between injury and surgery were compared between the transfer group and the non-transfer group using a Mann Whitney U-test. Average final VA, OTS, and number of additional surgeries in each group were compared using a Mann Whitney U-test. The ZOI, prevalence of IOFBs, and incidence of enucleation in each group were compared using a Fisher’s Exact test. To further control for confounding, the data was divided by OTS. Within each OTS category final VA was compared between transfer and non-transfer groups using the Mann Whitney U-test. The non-parametric Mann Whitney U-test and Fisher’s Exact test were used due to non-gaussian distribution of the data.
Results
Subject Demographics
Of the 238 open globe injury patients evaluated, 197 were transferred from an outside hospital and 41 presented directly at our emergency department. There were 180 males and 58 females, and the average age of the subjects was 36 years. The number of self-pay subjects was 69 (35.2%) in the transfer group, and 9 (21.4%) in the non-transfer group. Average duration of follow-up was 13.1 months for transferred subjects and 13.8 for non-transferred subjects.
Referring Facilities and Reasons for Transfer
In total, 197 patients were transferred from 36 referring facilities. The referring facilities included 3 Level I trauma centers and 3 Level II trauma centers. Nine of the facilities had 24/7 ophthalmology call coverage, 8 facilities had part-time ophthalmology coverage, and 18 facilities did not have any ophthalmology coverage. Of the transfer patients, 78 (39.6%) were transferred from an emergency department with ophthalmologists on call 24/7 and 44 (22.3%) were transferred from an emergency department with ophthalmologists on call part-time (Table 1). Additionally, 30 patients (15.2%) were transferred from a Level I trauma center and 14 patients (7.1%) were transferred from a Level II trauma center. Our academic center was the closest Level I trauma center for only 5 of the 36 referring facilities. Of the transferred patients, 15 patients (7.6%) were transported an extra 75+ miles to reach our institution despite there being another Level I trauma center closer to the referring facility.
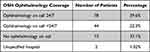 |
Table 1 Percentage of Patients Sent from Hospitals with Varying Levels of Ophthalmology Coverage |
Reasons for transfer included: lack of an on-call ophthalmologist, injuries requiring ophthalmology subspecialty care, non-ophthalmic injuries requiring specialty care not offered at the referring facility (ie, burn unit, neurosurgery, trauma), improper equipment needed to repair the injury, and recommendation by the on-call ophthalmologist to transfer the patient for a higher level of care. We were unable to obtain the reasons for transfer for all subjects.
Transfer Times and Times from Injury to Surgery
Out of 129 open globe injuries evaluated for transfer times and time from injury to surgery, 104 were included in the transfer group and 25 in the non-transfer group. On average, transfer patients spent 4 hours and 0 minutes at the outside hospital and 1 hour and 29 minutes in transit. In total, it took an average of 5 hours and 29 minutes for transfer patients to arrive at the academic center after presenting at the OSH (Table 2). On average, time from injury to surgery was 14 hours and 37 minutes for transfer patients, and 10 hours and 46 minutes for non-transfer patients. Compared to non-transfer patients, transfer patients had longer delays between injury and surgery (p = 0.0012), between presentation at the initial ED and surgery (p < 0.0001), and between injury and arrival at the academic center (p < 0.0001). The time from presentation at the initial ED (the OSH ED for transfer patients, and our ED for non-transfer patients) to surgery was an average of 12 hours and 53 minutes for transfer patients, and 8 hours and 0 minutes for non-transfer patients. Time from injury to surgery was greater than 24 hours for 8 patients in the transfer group and 1 patient in the non-transfer group. Time from initial presentation to surgery was greater than 24 hours for 4 patients in the transfer group. There were no patients in the non-transfer group who were delayed by more than 24 hours from initial presentation to surgery. Once patients arrived at our institution, there was no significant difference in time from arrival to surgery between the two groups (Table 3).
 |
Table 2 Time Transferred Open Globe Patients Spent in OSH and in Transit |
 |
Table 3 Average Time Open Globe Injury Patients Spent Between Injury, Presentation at the ED, and Surgery |
Vision and Ocular Outcomes
Out of 146 open globe injuries evaluated for visual outcomes, 117 were included in the transfer group and 29 in the non-transfer group. In total, 60 (41.1%) of the open globe injuries had an OTS of 1, 49 (33.6%) had an OTS of 2, 26 (17.8%) had an OTS of 3, 8 (5.5%) had an OTS of 4, and 3 (2.1%) had an OTS of 5. The first, second, and third ZOIs were involved in 93 (63.7%), 74 (50.7%), and 44 (30.1%) cases, respectively (56 cases involved multiple zones of injury). There were a total of 31 open globe injuries with intraocular foreign bodies. A total of 7 subjects developed endophthalmitis within the perioperative period, of those, 6 subjects were in the transfer group and 1 subject was in the non-transfer group. Six of the 7 subjects with endophthalmitis presented to the ED more than 24 hours after their injury (the time between injury and presentation at the ED ranged from 16.5 hours to 120.6 hours). The 6 subjects who presented greater than 24 hours after injury were diagnosed with endophthalmitis prior to surgical intervention. The patient who presented within 24 hours of injury was diagnosed after initial surgical intervention.
When comparing the injuries seen in each group, there was no significant difference in ocular trauma score (p = 0.055), zone of injury (ZOI 1: p = 0.67, ZOI 2: p = 1, ZOI 3: p = 0.26) or prevalence of IOFBs (p = 0.80). On average, the transfer group suffered from worse final visual acuities than the non-transfer group (p = 0.044). The average final visual acuity was 1.84 logMAR in the transfer group and 1.35 logMAR in the non-transfer group (Table 4). Further analysis was performed comparing subjects within each OTS group and no significant difference in final visual acuity between transfer and non-transfer patients was found (p = 0.051, p = 0.44, p = 0.77, and p = 0.63 for OTS 1 2, 3, and 4–5, respectively). Since there was no plan for adjustment of p-values for multiple comparisons, no definite conclusions can be drawn regarding these comparisons. There was no significant difference in the number of additional surgeries or the rate of enucleation when comparing the transfer and non-transfer subjects (Table 4).
 |
Table 4 Comparing Visual Outcomes in the Transfer and Non-Transfer Groups, While Controlling for OTS, ZOI, and Presence of an IOFBa |
Discussion
It is widely accepted in the field of ophthalmology that open globe injuries should have primary closure within 24 hours of injury to prevent complications.5 Our study shows that inter-hospital transfer within our state leads to a significant delay in primary closure of open globe injuries. Additionally, our study found that on average transferred patients had worse final visual acuities than their non-transferred counterparts. There was no difference in the incidence of enucleation or the need for additional surgeries between the two groups.
In this study, the majority of patients were male with an average age of 36 years. This is consistent with previous studies which found open globe injuries to be more common in young males.21–24 Analysis of health insurance status showed that nearly one-third of these patients were uninsured. The percentage of uninsured patients in both the transfer and non-transfer groups was higher than the average uninsured rate in their corresponding counties.25,26 This is consistent with other studies that found individuals who suffer from open globe injuries have higher uninsured rates than the general population.27
A total of 197 patients were transferred from 36 different hospitals for treatment of their open globe injuries. A large portion of these patients (37.1%) were transferred from a hospital without ophthalmology coverage. The remainder of the patients were transferred from hospitals with 24/7 ophthalmology coverage (39.6%) or part-time ophthalmology coverage (22.3%). We were able to obtain many of the reasons for transfer to our institution through the transfer notes, however we were not able to find this information for all subjects. Of the patients transferred from a level 1 trauma center, the recorded reasons for transfer included: need for ophthalmology subspecialty care, need for non-ophthalmic specialty care, improper equipment at referring facility, and recommendation by the on-call ophthalmologist to transfer the patient for a higher level of care. Additionally, our institution is one of the few centers in the state that is able to offer financial assistance to uninsured patients. This may have influenced the transfer of uninsured patients and may account for the higher percentage of uninsured patients in the transfer group. The data we were able to collect indicate that a majority of transfers from level 1 trauma centers were related to a lack of resources and specialized care in rural areas of our state. Efforts to increase the number of subspecialists and surgical equipment at level 1 trauma centers across the state may help mitigate the quantity and length of transfers, as well as, improve visual outcomes for patients living in rural areas.
We found that for patients that required transfer from a referring facility, there was a significant delay in time from injury to primary surgical repair. The average time from injury to primary surgical closure in transferred patients was 3 hours and 51 minutes longer in the transfer group compared to the non-transfer group (p = 0.0012) and the average time from initial presentation to surgery was 4 hours and 52 minutes longer in the transfer group (p < 0.0001). We found the average time from injury to surgical closure was 14 hours and 37 minutes in the transfer group, however there were 8 cases in which the additional time needed for transfer resulted in delays greater than 24 hours. The higher rate of subjects in the transfer group with delays greater than 24 hours would be assumed to result in an average lower final visual acuity, as previous studies have shown that a delay in primary closure greater than 24 hours leads to higher rates of complications and worse visual outcomes.7,9–11,14
Our study found that, on average, transfer subjects had worse final visual acuities than non-transfer subjects (p = 0.044) (Table 4). It is likely that the worse outcomes seen in the transfer group were the result of a variety of factors acting as mediators on final visual acuity. Possible mediators that may have influenced final visual outcomes in the transfer group include, but are not limited to, longer time from injury to surgical intervention, greater opportunity for non-medical globe manipulation with delayed closure, and longer travel distance for follow up appointments. It is also possible that the difference in vision outcomes was influenced by OTS acting as a confounding variable. While there was no difference in OTS between the transfer and non-transfer groups (p = 0.055), when subjects were compared only to those within the same category of OTS, we did not find a significant difference in the final VAs of transfer vs non-transfer subjects. Interestingly, within the OTS 1 group the difference in final VA approached statistical significance (p = 0.051). From these results, it can be hypothesized that open globe injuries with the greatest level of severity were most negatively affected by the process of inter-hospital transfer. However, the reduced sample size within each OTS category should be considered when interpreting the results of these comparisons. Further investigation with a higher-powered study is required to better understand the relationship between final visual acuity, transfer history, time from injury to surgery, and OTS.
Limitations
While this is the first study looking at the effects of inter-hospital transfer on open globe injuries, it does have the limitation of being a retrospective study. Since it is retrospective in nature, times from injury to surgery were likely influenced by discrepancies in the reported times of injury. For certain patients, time of injury was estimated due to the patient experiencing loss of consciousness or altered mental status during the injury. Due to a change in our center’s medical record system in 2014, there was variability in the records reviewed for this study. For records prior to 2014 the time of surgery was determined by the operative note and after 2014 the time of surgery was obtained more precisely by the procedure start time.
Additionally, there may have been limitations in the ocular exam results due to the nature of the injury preventing a complete assessment of ocular structures. Inability to assess pupils for relative afferent pupillary defect or the posterior pole for retinal detachment may have influenced calculations of the ocular trauma score. Transfer times were likely influenced by the variation in mode of transport from the referring hospital. Patients were transferred by helicopter, ambulance, or personal vehicle.
Another limitation of this study is small sample size. For the evaluation of ocular outcomes, exclusions were due mostly to inability to assess OTS or ZOI, missing information on time of injury or surgery, and loss to follow up. Given that OGIs are relatively rare injuries, a multicenter study may be required to obtain a larger sample size. Furthermore, it is difficult to compare visual outcomes of open globe injuries given the complexity and differing mechanisms of injury, as well as the wide variety of concurrent injuries that may affect visual prognosis.
A very small percentage of the open globe injuries included in the study had ocular trauma scores of 4 or 5, possibly due to less severe injuries being treated more frequently at the outside hospital, instead of being transferred. This could result in our study having a higher percentage of more severe injuries resulting in poorer final visual outcomes.
Conclusion
This study shows that inter-hospital transfer leads to an approximately 4-hour delay in surgical intervention for open globe injuries. In addition, the study found that transferred open globe injuries, on average, resulted in poorer final visual acuities. Many hospitals in this study transferred open globe patients despite having ophthalmology coverage or a closer Level I trauma center, which likely resulted in a delay to surgical intervention. Although the transferred subjects had worse final visual acuities in our study, further investigation is required to rule out the possibility of OTS as a confounding variable. A larger, multi-center study that focuses on the effects of OTS on outcomes and accounts for the high variability between open globe cases is warranted to further our knowledge of trauma outcomes and time-to-surgery.
Abbreviations
IOFB, intraocular foreign body; ED, emergency department; ZOI, zone of injury; OTS, ocular trauma score; VA, visual acuity; OSH, outside hospital; UNC, University of North Carolina.
Funding
Funding for this investigation was provided by the UNC Medical Alumni.
Disclosure
The authors report no conflicts of interest in this work.
References
1. May DR, Kuhn FP, Morris RE, et al. The epidemiology of serious eye injuries from the United States Eye Injury Registry. Graefes Arch Clin Exp Ophthalmol. 2000;238(2):153–157. doi:10.1007/pl00007884
2. Mir TA, Canner JK, Zafar S, et al. Characteristics of open globe injuries in the United States From 2006 to 2014. JAMA Ophthalmol. 2020;138(3):268–275. doi:10.1001/jamaophthalmol.2019.5823
3. Agrawal R, Shah M, Mireskandari K, Yong GK. Controversies in ocular trauma classification and management: review. Int Ophthalmol. 2013;33(4):435–445. doi:10.1007/s10792-012-9698-y
4. Kuhn F, Morris R, Witherspoon CD, Heimann K, Jeffers JB, Treister G. A standardized classification of ocular trauma. Graefes Arch Clin Exp Ophthalmol. 1996;234(6):399–403. doi:10.1007/BF00190717
5. UpToDate. Open globe injuries: emergency evaluation and initial management. Available from: https://www.uptodate.com/contents/open-globe-injuries-emergency-evaluation-and-initial-management?search=open%20globe%20injury&source=search_result&selectedTitle=1~18&usage_type=default&display_rank=1#H29.
6. Ojuok E, Uppuluri A, Langer PD, et al. Predictive factors of enucleation after open globe injuries. Graefes Arch Clin Exp Ophthalmol. 2021;259(1):247–255. doi:10.1007/s00417-020-04794-6
7. Ahmed Y, Schimel AM, Pathengay A, et al. Endophthalmitis following open-globe injuries. Eye. 2012;26(2):212–217. doi:10.1038/eye.2011.313
8. Zhang Y, Zhang MN, Jiang CH, et al. Endophthalmitis following open globe injury. Br J Ophthalmol. 2010;94(1):111–114. doi:10.1136/bjo.2009.164913
9. Blanch RJ, Bishop J, Javidi H, Murray PI. Effect of time to primary repair on final visual outcome after open globe injury. Br J Ophthalmol. 2019;103(10):1491–1494. doi:10.1136/bjophthalmol-2017-311559
10. Agrawal R, Rao G, Naigaonkar R, et al. Prognostic factors for vision outcome after surgical repair of open globe injuries. Indian J Ophthalmol. 2011;59(6):465–470. doi:10.4103/0301-4738.86314
11. Thompson JT, Parver LM, Enger CL, et al. Infectious endophthalmitis after penetrating injuries with retained intraocular foreign bodies. National Eye Trauma System. Ophthalmology. 1993;100(10):1468–1474. doi:10.1016/s0161-6420(93)31454-5
12. Duch-Samper AM, Chaqués-Alepuz V, Menezo JL, Hurtado-Sarrió M. Endophthalmitis following open-globe injuries. Curr Opin Ophthalmol. 1998;9(3):59–65. doi:10.1097/00055735-199806000-00011
13. Loporchio D, Mukkamala L, Gorukanti K, et al. Intraocular foreign bodies: a review. Surv Ophthalmol. 2016;61(5):582–596. doi:10.1016/j.survophthal.2016.03.005
14. Asencio MA, Huertas M, Carranza R, et al. A case-control study of post-traumatic endophthalmitis at a Spanish hospital. Int Ophthalmol. 2016;36(2):185–194. doi:10.1007/s10792-015-0099-x
15. Cruvinel Isaac DL, Ghanem VC, Nascimento MA, et al. Prognostic factors in open globe injuries. Ophthalmologica. 2003;217(6):431–435. doi:10.1159/000073075
16. Al-Mezaine HS, Osman EA, Kangave D, Abu El-Asrar AM. Prognostic factors after repair of open globe injuries. J Trauma. 2010;69(4):943–947. doi:10.1097/ta.0b013e3181c9f395
17. Schulze-Bonsel K, Feltgen N, Burau H, Hansen LL, Bach M. Visual acuities “Hand Motion” and “Counting Fingers” can be quantified using the Freiburg Visual Acuity Test. Invest Ophthalmol Vis Sci. 2006;47:1236–1240. doi:10.1167/iovs.05-0981
18. Lange C, Feltgen N, Junker B, Schulze-Bonsel K, Bach M. Resolving the clinical acuity categories “hand motion” and “counting fingers” using the Freiburg Visual Acuity Test (FrACT). Graefes Arch Clin Exp Ophthalmol. 2009;247(1):137–142. doi:10.1007/s00417-008-0926-0
19. Bach M, Schulze-Bonsel K, Feltgen N, Burau H, Hansen LL. Author response: numerical imputation for low vision states [electronic letter]. Invest Ophthalmol Vis Sci. 2007;2007:2474126416680670.
20. Kuhn F, Maisiak R, Mann L, et al. The Ocular Trauma Score (OTS). Ophthalmol Clin North Am. 2002;15(2):163–vi. doi:10.1016/s0896-1549(02)00007-x
21. Batur M, Seven E, Esmer O, et al. Epidemiology of adult open globe injury. J Craniofac Surg. 2016;27(7):1636–1641. doi:10.1097/SCS.0000000000003001
22. Mansouri M, Faghihi H, Hajizadeh F, et al. Epidemiology of open-globe injuries in Iran: analysis of 2340 cases in 5 years (report no. 1). Retina. 2009;29(8):1141–1149. doi:10.1097/IAE.0b013e3181a395ac
23. Knyazer B, Bilenko N, Levy J, et al. Open globe eye injury characteristics and prognostic factors in southern Israel: a retrospective epidemiologic review of 10 years experience. Isr Med Assoc J. 2013;15(3):158–162.
24. Koo L, Kapadia MK, Singh RP, Sheridan R, Hatton MP. Gender differences in etiology and outcome of open globe injuries. J Trauma. 2005;59(1):175–178. doi:10.1097/01.ta.0000173624.37438.d6
25. U.S. Census Bureau. Small area health insurance estimates. Available from: https://www.census.gov/data-tools/demo/sahie/#/.
26. The Cecil G. Sheps center for health services research, county estimates of the number of uninsured in North Carolina 2005 update. Chapel Hill, North Carolina. Available from: https://www.shepscenter.unc.edu/product/county-estimates-of-the-number-of-uninsured-in-north-carolina-2005-update/.
27. Ojuok E, Uppuluri A, Langer PD, et al. Demographic trends of open globe injuries in a large inpatient sample. Eye. 2021;35(8):2270–2276. doi:10.1038/s41433-020-01249-4
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


