Back to Journals » Clinical Ophthalmology » Volume 16
Comparison of Three Tonometers in Measuring Intraocular Pressure in Eyes That Underwent Myopic Laser in situ Keratomileusis and Photorefractive Keratectomy
Authors Ang RET , Bargas NVR, Martinez GHA , Sosuan GMN , Nabor-Umali MI
Received 14 February 2022
Accepted for publication 16 May 2022
Published 27 May 2022 Volume 2022:16 Pages 1623—1637
DOI https://doi.org/10.2147/OPTH.S362344
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Robert Edward T Ang,1– 3 Neiman Vincent R Bargas,1 Gladness Henna A Martinez,1 George Michael N Sosuan,3 Maria Isabel Nabor-Umali2
1Department of Ophthalmology, Cardinal Santos Medical Center, San Juan City, Metro Manila, Philippines; 2Cornea and Refractive Surgery Service, Asian Eye Institute, Makati City, Metro Manila, Philippines; 3Glaucoma Service, Asian Eye Institute, Makati City, Metro Manila, Philippines
Correspondence: Robert Edward T Ang, Cornea and Refractive Surgery and Glaucoma Services, Asian Eye Institute, Makati City, Metro Manila, Philippines, Email [email protected]
Objective: To compare the intraocular pressure (IOP) obtained by Goldmann applanation tonometer (GAT), correcting applanation tonometer surface (CATS) and biomechanically corrected IOP (bIOP) of Corvis ST tonometer (CVS); and to determine the effects of manifest refraction spherical equivalent (MRSE), central corneal thickness (CCT) and mean corneal curvature (Km) on the IOP measurements of corneal refractive patients.
Methods: This was a single-center, retrospective, cross-sectional study of 120 eyes of 64 patients from May 1, 2020 to June 1, 2021 who underwent laser in situ keratomileusis (LASIK) or photorefractive keratectomy (PRK). The level of agreement between the three tonometers was evaluated, and correlation between parameters was calculated using Pearson correlation.
Results: Mean preoperative to postoperative IOP in LASIK and PRK was 15.1 ± 3 to 11.3 ± 2.1 and 14.4 ± 2.6 to 12.1 ± 3 using GAT, 16.4 ± 2.8 to 13.1 ± 2.3 and 15.9 ± 2.6 to 13.7 ± 3 using CATS and 14.8 ± 2.4 to 12.9 ± 1.5 and 14.2 ± 2.4 to 12.6 ± 1.9 using CVS-bIOP. Preoperative IOP correlation between each tonometer pair showed that the lowest mean difference was between GAT and CVS-bIOP (0.32 in LASIK, 0.15 in PRK). Preoperative to postoperative IOP correlation of each tonometer resulted in a difference of 3.77, 2.30 in GAT; 3.32, 2.28 in CATS and 1.88, 1.62 in CVS-bIOP in the LASIK and PRK groups, respectively. Percentage change in CCT and Km was not correlated while change in MRSE had a weak relationship with percentage change in CVS-bIOP.
Conclusion: Preoperatively, GAT and CVS-bIOP had the best agreement in IOP measurements. CATS recorded the highest IOP preoperatively and postoperatively. IOP decreased in the three tonometers after LASIK and PRK with GAT having the largest decrease. CVS-bIOP had the lowest change between preoperative and postoperative IOP measurements. Only percentage change in MRSE was correlated with percentage change in CVS-bIOP in the LASIK group.
Keywords: IOP, GAT, CATS, CVS, LASIK, PRK
Background
The pressure inside the eye necessary for it to continue to function normally and to maintain its normal structure is called the intraocular pressure (IOP). An IOP of 10–21 mm Hg is considered normal in humans.1,2 Tonometers are instruments used for measuring IOP and several of them are available in the market with each one having its own principle, advantages and disadvantages.2–4 The accuracy and reproducibility of a tonometer are influenced by several ocular parameters.5 With the growing numbers of corneal refractive surgeries and the increasing prevalence of glaucoma, accurate IOP measurement is a major concern.6
The techniques for measuring IOP can be classified as applanation, indentation, rebound, dynamic contour and non-contact type. Tonometers that use applanation are Goldmann applanation tonometer (GAT) and Correcting applanation tonometer surface (CATS, Reichert, USA), indentation is pneumotonometer (Pneumotonometer, Reichert, USA), both applanation and indentation are Tono-pen (Tono-Pen, Reichert, USA), and rebound is i-Care (i-Care, USA), dynamic contour is Dynamic contour tonometer (DCT, Pascale, Switzerland), and non-contact are air-puff tonometers such as Corvis ST (CVS, Oculus, Germany) and Ocular response analyzer (ORA, Reichert, USA).
GAT was introduced in the 1950s and is based on Imbert-Fick’s principle and assumes that the cornea is dry, infinitely thin, perfectly elastic and flexible. However, none of these features holds true with the cornea.3,4,7 Several studies have shown that GAT is affected by corneal properties like central corneal thickness (CCT),8,9 where IOP readings tend to overestimated or underestimated in thick and thin corneas. Along with CCT, other parameters that may influence IOP readings were corneal curvature, tear film and biomechanical properties of the cornea.10–12 Several authors have developed nomograms to correct GAT based on varying CCT.13–16 However, the use of these nomograms remains controversial.15,16 Corneal refractive surgeries which include LASIK and PRK are done to correct ametropia. These procedures use an excimer laser modifying the corneal biomechanics.17–19 LASIK and PRK, in particular myopic corrections, cause significant GAT reductions postoperatively due to deeper central ablation depths.6,19 Many authors have tried to developed formulas for IOP correction but none gained acceptance.20,21 Despite the inaccuracies of GAT, it remained as the reference standard for IOP measurements.
Newer devices and techniques continue to be developed for measuring IOP such as the CATS and CVS. CATS is a modification of the original GAT prism that uses a sinusoidal curved (concave centrally and convex peripherally) surface that matches the curvature of the cornea. The prism was designed to minimize IOP measurement errors made by GAT. Furthermore, it does not require recalibration and uses the same measurement protocol as GAT.22–26 Clinical studies have demonstrated that CATS measurements are less affected by changes in CCT, corneal curvature, tear film and biomechanical properties of the cornea.22,23 Another device, the CVS is a combination of a non-contact tonometer that uses an air puff and an ultra-high speed Scheimpflug camera that captures a series of images to analyze corneal biomechanics.27–37 It has a unique capability of providing a biomechanically corrected IOP (bIOP) that gives more accurate IOP readings independent of the effect of CCT and biomechanical properties of the cornea.27,33
The accurate measurement of IOP is difficult after LASIK and PRK because of changes in corneal thickness and corneal curvature. Topical steroids are routinely used postoperatively but erroneous measurements may be masking the incidence and severity of steroid-induced ocular hypertension. Some patients may develop glaucoma later in life and would need accurate IOP measurements to diagnose glaucoma, monitor progression, and assess adequacy of treatment. Since GAT has been found to be less accurate in post-LASIK and post-PRK eyes, it is crucial to evaluate other tonometers that may be least affected by changes in corneal metrics and corneal biomechanics.
Previous studies have studied the accuracy of IOP measurements of CVS compared to GAT in post-refractive eyes, while comparative studies between CATS and GAT were performed on unoperated eyes or eyes with glaucoma. To the best of our knowledge, this was the first study to compare the IOP measurements on LASIK and PRK eyes preoperatively and postoperatively at 3 months using these three devices, GAT, CATS and CVS. The aim of the study is to compare the IOP obtained by GAT, CATS bIOP of CVS, and to determine the effects of MRSE, CCT and Km on the IOP measurements of corneal refractive patients.
Methods
This was a single-center, retrospective, cross-sectional study of patients who underwent LASIK surgery or PRK in an ambulatory eye center in the Philippines. The study adhered to the tenets of Declaration of Helsinki and the Data Privacy Act of 2012. Ethics approval was obtained before the conduct of study (ERC#2021-004, February 22, 2021).
The study included patients 18 years old and above who underwent uneventful LASIK or PRK in one or both eyes performed by the one surgeon from May 1, 2020, to June 1, 2021. Only eyes that were previously myopic, had a target refraction of emmetropia and had IOP measurements taken by GAT, CATS and CVS-bIOP preoperatively and at 3 months postoperatively were included in the study. Exclusion criteria were eyes that had any previous ocular surgeries, diagnosed with glaucoma, had any corneal pathologies that may affect IOP readings such as corneal scars, edema and dystrophies. Records with incomplete follow-up data were also excluded from the study.
Preoperatively and at 3 months postoperatively, a complete ophthalmic examination was performed on each patient, including visual acuity measurement and slit lamp biomicroscopy. The data collected included age, gender, manifest refraction, central corneal thickness, mean corneal curvature, intraocular pressure, maximum ablation depth, and type of surgery performed. Manifest refraction was done using a phoropter. Measurements of central corneal thickness and mean corneal curvature were obtained using the Pentacam (Oculus Optikgerate GmbH, Wetzlar, Germany, software version: 6.08r33). IOP were measured using GAT (model: AT900) and CATS (model: CATS-R) and bIOP was measured using the CVS (Corvis ST, Oculus Optikgerate GmbH, Wetzlar, Germany, software version: 6.08r190). Maximum ablation depth was collected from the excimer laser (Teneo II, Bausch and Lomb, Germany). The 3 months postoperative time point was chosen to eliminate the influence of corneal edema, stabilize corneal astigmatism and avoid the effects of topical corticosteroids on IOP measurements. To eliminate bias and standardize the testing sequence of measuring the IOP, all participants underwent the following tests in a single session and in the same order: CVS, GAT and CATS. The CVS measurements are routinely performed by diagnostic technicians who underwent machine training. Only measurements with an “OK” quality scan indicating a good image quality were included in the study. Measurements using the GAT and CATS were done by any one of three trained clinicians. A drop of topical anesthetic and a drop of fluorescent dye was instilled to each eye, and excess dye was wiped off prior to IOP measurement. Applanation tonometry was done first using the GAT, then replacing it with a CATS prism. Only a single measurement was performed for each eye. Results were then noted in the patient’s medical record.
During the LASIK procedure, a femtosecond laser (Victus, Bausch and Lomb, Germany) was used to cut a 120-micron flap. The flap was retracted, laser photoablation performed using the excimer laser (Teneo II, Bausch and Lomb, Germany), and the flap repositioned immediately afterwards. In the PRK procedure, the epithelial layer was removed either manually using 30-second alcohol exposure and manual debridement or in an automated fashion using the excimer laser (Teneo II, Bausch and Lomb, Germany), in the transepithelial PRK mode. A predetermined amount of stromal tissue was ablated and a bandage contact lens applied afterwards.
Statistical Analysis
All data collected were anonymized and manually inputted into an electronic spreadsheet. (Microsoft Excel 2021, software version 16.45). The statistical analyses were performed using SPSS statistical software package (SPSS 2018, version 20.0 software, IBM, Corp, Armonk, NY, USA). Descriptive statistical results included means, standard deviations, range, change and percentage change of parameters. Gender distribution of patients who underwent LASIK and PRK was shown using ratio of frequency. The difference between pre- and post-surgery MRSE, CCT, Km and IOP values were analyzed using paired-sample t-test. Comparison of the three tonometers within the LASIK and PRK group was performed using one-way analysis of variance (ANOVA). Waller-Duncan was used as post hoc analysis to determine within group difference in means. The comparison of percentage change in MRSE, CCT, Km and IOP between LASIK and PRK (interclass) was assessed through the independent t-test. The linear fit of correlation was obtained using Pearson bivariate correlation analysis. Bland-Altman analysis was used to evaluate the level of agreement. Statistical significance is set at p value of less than 0.05.
Results
A database search was performed for patients who had undergone standard refractive screening and successful LASIK or PRK surgery from May 1, 2020 to June 1, 2021. All eyes underwent IOP measurements using the GAT, CATS and CVS tonometers preoperatively and at the 3-month postoperative visit. The search yielded 203 eyes of 105 patients who underwent LASIK and PRK during the study period. Eighty-three eyes were excluded due to lack of 3-month post-operative follow-up. A final tally of 120 eyes of 64 patients were included in the study.
Mean age (29.7±7.6 vs 29.2±8.1 years, p = 0.727) and male:female ratio (20:40 vs 19:41, p = 0.845) were similar between LASIK and PRK. Comparing with LASIK preoperatively, patients who underwent PRK had significantly thinner mean CCT (563.8±22.1 vs 540.7±32.6 um, p = 0.000) with higher mean MRSE (−3.9±1.4 vs −5.2±1.7 D, p = 0.000) that led to a higher maximum ablation depth (79.6±21.7 vs 90.7±26.7 um, p = 0.013). Although the Km range was wider in PRK group, the mean Km between groups was not statistically different (43.4±1.1 D vs 43.4±1.2 D, p = 0.883) (Table 1).
 |
Table 1 Baseline Characteristics of Eyes That Had LASIK and PRK |
Preoperative mean IOP measurements comparing each tonometer between LASIK and PRK were comparable [p (inter) >0.05]. CATS had the highest mean IOP reading in both groups, followed by GAT, then CVS-bIOP (Table 2). Post-hoc analysis showed that the CATS measurement was significantly different from both the GAT and CVS-bIOP. Correlation between the preoperative IOP measurements of the three tonometer pairs showed a direct relationship in both LASIK (p = 0.000) and PRK (p = 0.000 to 0.027) (Table 3). The Bland-Altman plots illustrated the level of agreement with 95% confidence between the IOP measurements of the tonometer pairs preoperatively in both LASIK and PRK. The tonometer pair CATS-CVS-bIOP had the highest mean difference followed by GAT-CATS, indicating that preoperative CATS measurement was the most different to GAT and CVS-bIOP, consistent with the post-hoc analysis above. GAT-CVS-bIOP had the least mean difference in preoperative IOP measurements in LASIK and PRK groups, meaning they are the most similar preoperatively (Figure 1).
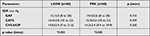 |
Table 2 Baseline IOP of Eyes That Had LASIK and PRK |
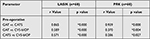 |
Table 3 Pearson Correlation Analysis of Preoperative Mean IOP Measurements Between 2 Tonometers (Tonometer Pairs) |
When comparing the preoperative to postoperative IOP measurements, all three tonometers decreased significantly in both the LASIK and PRK groups (p = 0.000) (Table 4). The IOP measured by each tonometer preoperatively was directly correlated to the IOP measured postoperatively for both LASIK and PRK (p < 0.005) (Table 5). Bland Altman analysis showed the difference between preoperative and postoperative mean IOP measurements per tonometer (Figure 2). GAT had the highest mean difference from preoperative to postoperative measurements closely followed by CATS. CVS-bIOP had the lowest mean difference in IOP values before and after surgery, indicating that CVS-bIOP is the most minimally affected IOP measurement. These trends are consistent after both LASIK and PRK procedures.
 |
Table 4 Changes in IOP Before and After LASIK or PRK |
 |
Table 5 Pearson Correlation Analysis of Preoperative and Postoperative Measurements of Each Tonometer |
Mean postoperative GAT and CATS measurements were strongly correlated in both LASIK and PRK. Postoperative CVS-bIOP measurements were not correlated with GAT and CATS measurements in the LASIK group and mildly correlated in the PRK group (Table 6).
 |
Table 6 Pearson Correlation Analysis of Postoperative Mean IOP Measurements Between 2 Tonometers (Tonometer Pairs) |
In terms of percentage change or magnitude of change in IOP measurements before and after refractive surgery, GAT and CATS were strongly correlated both in LASIK and PRK while CVS-bIOP was mildly correlated with GAT and CATS in LASIK but not correlated with GAT and CATS in PRK (Table 7).
 |
Table 7 Pearson Correlation Analysis of Percentage Change (%Δ) Before and After LASIK and PRK Between 2 Tonometers (Tonometer Pairs) |
The mean MRSE, CCT and Km decreased significantly in both the LASIK and PRK groups after refractive correction (p = 0.000) with higher changes seen in the PRK group (Tables 8 and 9). We calculated to determine if there was a correlation between the percentage change in MRSE, Km, and CCT with percentage change in IOP of each tonometer. The percentage change in GAT and CATS was not found to be correlated with the percentage change in MRSE, CCT and Km both in LASIK and PRK. Only the percentage change in MRSE was shown to have a weak relationship with the percentage change in CVS-bIOP in the LASIK group (r=−0.347, p = 0.007) (Table 10).
 |
Table 8 Changes in MRSE, CCT and Km Before and After LASIK and PRK |
 |
Table 9 Percentage Change (%Δ) in MRSE, CCT and Km Before and After LASIK or PRK (Inter) |
 |
Table 10 Pearson Correlation Analysis Between Percentage Change (%Δ) in IOP Measurements versus Percentage Change (%Δ) in MRSE, CCT and Km in LASIK and PRK |
Discussion
Corneal refractive surgeries such as LASIK and PRK have gained widespread popularity for patients desiring clear vision. These procedures, which use an excimer laser to reshape the cornea, involve ablation of stromal tissue, thereby altering corneal thickness, curvature and corneal biomechanics. Alterations in these parameters have been shown in previous studies to affect intraocular pressure measurements, especially with the use of the GAT.8–12 Thus, it is of great importance to find the most accurate way of measuring IOP for post-refractive patients.6,8,17,21,28–30,33
Two novel tonometers designed to be minimally affected by changes in corneal properties were evaluated and compared with GAT. The CATS prism is a modified version of the GAT prism that uses a sinusoidal (concave-convex) curved surface that matches the curvature of the cornea. The CVS is a non-contact air-puff tonometer with an ultra-high speed Scheimpflug camera that measures biomechanical index and biomechanical IOP. Both devices were developed to reduce errors in IOP measurements induced by corneal thickness, curvature, tear film and biomechanical properties.
In our practice, we screen a good number of patients for refractive surgery and perform both LASIK and PRK. It is important for us to determine if we are getting accurate IOP readings after surgery. In this endeavor, we are making the assumption that the internal eye is unchanged after corneal laser refractive surgery, therefore the IOP should be the same or very similar. Comparing the IOP measurements using the GAT, CATS and CVS-bIOP without serving judgment of which is the correct IOP, we wanted to find out which device would give the closest measurements to preoperative values despite the change in corneal thickness, corneal curvature, and manifest refraction.
This study included 120 eyes (64 patients) who underwent LASIK and PRK during the study period. To qualify for LASIK, based on our screening protocol, patients should have thicker CCT of at least 500 microns, an estimated residual stromal bed thickness of at least 250 microns and regular topographies. Patients who did not meet these criteria underwent PRK. PRK patients had a thinner preoperative CCT and tended to have higher MRSE necessitating higher maximum ablation and lesser residual bed thickness that violated our LASIK qualification parameters. Patients with forme fruste or keratoconus were disqualified from both LASIK and PRK.
In our study, GAT had the highest mean decrease from preoperative to postoperative measurements. Even if the mean change in CATS was comparable with GAT, CATS still registered the highest IOP values measured either preoperatively or postoperatively. Although CVS-bIOP recorded the lowest mean IOP value, it had the best level of agreement with preoperative GAT. More importantly, CVS-bIOP had the lowest percentage difference in preoperative to postoperative IOP measurement, suggesting that it may be the least affected in post-refractive IOP measurements. Further analysis showed that post-operative IOP measurement using the CVS-bIOP did not follow the same pattern as GAT and CATS in LASIK eyes but seemed to follow the same pattern in post-PRK eyes. We found that CVS-bIOP behaves differently in LASIK versus PRK eyes compared to GAT and CATS. This observation may be explained by the compensatory biomechanical adjustments in IOP measurement in the CVS software which detected the “softer” eye with a flap versus a stiffer eye which underwent PRK. However, we feel that the magnitude of IOP change may be a stronger predictor of the robustness of CVS-bIOP measurements in post-refractive eyes, not the postoperative mean IOP values per se. Our study results showed that GAT and CATS were both strongly correlated with the magnitude of IOP change both in LASIK and PRK. Larger changes in CATS are consistently seen alongside large changes in GAT. CVS-bIOP, on the other hand, was only mildly correlated to the magnitude of IOP change in LASIK but not correlated at all in PRK. We postulate that the LASIK procedure tends to decrease biomechanical stiffness of the cornea a lot more than PRK because of the flap cut and the ablation performed deeper into the stroma, so CVS-bIOP is still mildly affected in IOP measurements. PRK eyes, on the other hand, still have an intact corneal structure being without a flap but is now much thinner after surgery, so the CVS is able to negate the effect of the thinner CCT and therefore tends to perform IOP measurements differently compared to GAT and CATS.
GAT has been accepted as the reference standard in IOP measurements and normal-abnormal values in treatment protocols such as glaucoma are based on GAT measurements. Numerous studies have shown that GAT is significantly affected by CCT and corneal curvature. In our study comparing the three tonometers, we arrived at two important findings. First, GAT had the lowest mean IOP values postoperatively compared to CATS and CVS-bIOP. Second, the largest difference in IOP measurements before and after surgery was also with GAT. Earlier studies have likewise reported significant reduction in GAT after corneal refractive surgery.28–30 These findings suggest that GAT is the most affected tonometer by corneal laser surgery and this is thought to be brought about by the changes in refractive correction (MRSE), removal of corneal tissue (CCT) and corneal curvature changes (Km) accompanying LASIK and PRK.
Physicians have the longest experience with GAT and there has been universal acceptance that CCT does have a strong influence on GAT measurements. Shafiq reported the influence of CCT on IOP measurements with GAT in normal individuals. Their study had a mean IOP value of 15.35 mm Hg and mean CCT value of 531.50 um in 500 eyes and concluded that CCT was significantly correlated with intraocular pressure in which a thicker cornea overestimates IOP and thinner cornea underestimates IOP.38 Lat-Luna et al investigated 222 Filipino eyes and also determined the correlation of CCT and GAT. The study revealed a significant linear correlation between CCT and GAT of which IOP is noted to increase by 4.3 mm Hg/100 um CCT.39 On the other hand, Marjanović et al observed that CCT had no influence on IOP measurements with GAT in a population between healthy and glaucomatous eyes.40 Chang et al mentioned that the change in CCT associated with refractive change in LASIK and PRK explained less than 1% of the change in measured GAT, therefore parameters other than CCT might influence IOP measurement error using applanation tonometry.38 Liu et al made a model wherein IOP readings from applanation tonometry are not always reflective of the true IOP value when corneal thickness, curvature and biomechanical properties deviate from the normal. Their model predicted that variations in CCT could cause a deviation in IOP readings within a range of 2.87mm Hg, variations in curvature by 1.76mm Hg and variations in corneal biomechanics by 17.26mm Hg.8 They also found that the effect of CCT and curvature on IOP is actually nonlinear. A study by Kyei et al also reported that there was no significant association between CCT and GAT and this is due to the viscoelastic property of the cornea in which stiffness is associated with the degree of application of tension.41 In our study, we found no correlation between CCT preoperatively as well as change in CCT postoperatively to IOP measurements of the three tonometers. Our observation is that the magnitude of decrease in CCT was not proportional or linear in relationship with the magnitude of change in IOP measurements, therefore direct correlations were not found.
With respect to corneal curvature, a study by Mark et al of 200 patients (400 eyes) reported that there were variations in corneal curvature between different eyes and it had a small but definite effect on GAT IOP measurements. Their study showed that a 3 diopter increase of corneal curvature led to an increase of 1mm Hg rise in the GAT.42 Gunvant et al also studied the influence of corneal curvature to GAT and found that a 1 diopter increase in mean corneal curvature corresponds to a 1.14 mm Hg increase in GAT.43 However, there are also studies that refute the correlation of corneal curvature with GAT. Rask et al examined 30 healthy eyes and 9 keratoconus patients and showed no correlation between the two.44 A study by Kaufmann et al consisting of 228 eyes compared IOP measurements with 2 tonometers, namely, GAT and Dynamic contour tonometer (DCT) and the effect of corneal curvature. They also concluded that there was no correlation between either of the two tonometers with corneal curvature.45 The previous studies mentioned trends between corneal curvature increase and IOP. Our study deals with myopic treatments which lead to flattening of corneal curvature. This may be the reason why our study did not find a correlation or perhaps there was truly no correlation at all between Km (corneal curvature) and IOP. Future research may be able to determine whether a relationship exists.
In terms of refractive error, Nomura et al reported that in 1855 subjects, there was a positive correlation between GAT and increasing degrees of myopia even after adjusting for age, CCT and other relevant factors.46 Another author, Schallhorn et al postulated a nomogram for myopic LASIK and PRK wherein a 1 diopter increase in the amount of myopia corrected lowered the postoperative IOP by 0.4 mm Hg.19 There are also contradicting studies regarding refractive error and IOP. Yassin et al observed in eyes of 458 participants, that variations in IOP by refractive error were not statistically significant.47 Even Bonomi et al compared IOP between two eyes in anisometropic subjects with unilateral high myopia and also found no statistical difference.48
In our study, we did not find a positive statistical correlation between changes in MRSE, CCT, Km and GAT measurements, whether postoperative or magnitude of change before and after surgery. Possible explanations are that the population in our study had a degree of CCT that is within a narrow range and it would take a very large number of eyes to show statistical correlation, that these parameters are truly not significant factors as concluded by previous studies or that biomechanical changes are the more likely cause of the changes in GAT measurements postoperatively. Several attempts have been made to address this problem by either quantifying the effect of CCT and other corneal parameters that affect corneal stiffness. Others attempted to create algorithms for GAT IOP correction20,21 while others developed new techniques to reduce the dependence of IOP measurement on corneal properties.25,28,32
At the time of writing, only 2 studies22,23 have been published on CATS in measuring IOP in unoperated eyes and no published study was found on post-refractive eyes. The protocol and the measurement technique between GAT and CATS are the same. CATS prism was designed to measure the same pressure as the GAT, however, under nominal conditions only, which includes average CCT, average corneal curvature, average rigidity and average tear film. However, the CATS prism attempts to reduce sensitivities to several corneal properties. First, the design yielded a decreased CCT sensitivity of 5 mm Hg/1 mm compared to GAT. This reduction was due to the contact surface that supports the central section of the cornea thereby the stress during applanation is evenly distributed. Second, it reduced the sensitivity to an individual’s average corneal elasticity or rigidity from ± 8 mm Hg error in GAT to ±2 mm Hg only in CATS. Third, the design also reduced sensitivity to corneal curvature from ± 2.5 mm Hg of GAT to ±1.5 mm Hg. Fourth, the surface tension between the cornea, tear film and the tonometer was reduced to approximately 45% with CATS prism. Last, with different variations in the corneal geometry, the CATS design also reduced the average attractive force to approximately 1.5 mm Hg.26 McCafferty et al performed a clinical study composed of 243 eyes. One hundred and seventy-three eyes had average corneas while the rest were grouped into low CCT (<500 um) and high CCT (>600 um), high astigmatism (>3 diopters) and low astigmatism (<3 diopters), low IOP (<16 mm Hg), moderate IOP (16–23 mm Hg) and high IOP (>23 mm Hg). The study concluded the overall mean difference between GAT and CATS was 0.43 mm Hg higher with CATS, and this was not statistically significant.22,23 Our results also showed that CATS measurements were higher than GAT. However, the mean difference we found was higher, at 1.33 mm Hg in preoperative LASIK and 1.57 mm Hg in preoperative PRK groups. Despite the difference in IOP values, GAT and CATS behaved very similarly probably because their mode of measurement is both applanation. CATS is positively correlated with GAT in preoperative, postoperative measurements and change in IOP and like GAT, CATS was not found to be correlated with change in MRSE, CCT and Km. The reduction in contact area to the cornea of CATS is postulated to make the CATS better but additional studies are needed in establishing its value and accuracy in post-refractive eyes.
CVS-bIOP is the latest technology that addresses the need to accurately measure IOP that takes into account biomechanical qualities of the cornea while negating the influence of other factors such as corneal thickness and curvature. Nakao et al evaluated GAT and CVS-bIOP in 71 eyes with primary open angle glaucoma (POAG) and showed that GAT had higher values while CVS-bIOP had lower values and a narrower, albeit better, level of agreement. They concluded that GAT and CVS-bIOP had no proportional bias and that both tonometers are not interchangeable.49 Vinciguerra et al analyzed both healthy eyes and eyes with ocular hypertension, POAG, and normal-tension glaucoma. The study revealed that GAT and CVS-bIOP had significant differences, that CVS-bIOP was significantly lower than GAT in all of the groups and that CCT seemed to no longer influence IOP in these groups. Therefore, differences in corneal biomechanics in every individual have a greater impact on IOP measurement errors rather than CCT or corneal curvature.33,42 There were other studies which compared the CVS-bIOP and GAT in post-refractive eyes. A study by Lee et al composed of 129 eyes who underwent LASIK and PRK evaluated the CVS-bIOP. They reported that CVS-bIOP remained stable after LASIK and PRK since the values were almost the same preoperatively and postoperatively.29 Chen et al used a database composed of 144 myopes who underwent LASIK, PRK and small-incision lenticule extraction (SMILE) and compared four tonometers namely, GAT, DCT, Ocular response analyzer (ORA) and CVS. Their study found that among the four tonometers, CVS-bIOP had the smallest differences before and after surgery, that GAT had the largest difference and wider level of agreement among the tonometers and that the PRK group had smaller reductions in IOP readings than LASIK.30 These findings are similar to our study. We found only one study contrary with ours. Ye et al studied 122 eyes who had ocular hypertension and POAG and concluded that CVS-bIOP measurements tended to overestimate IOP by 1.17 mm Hg in compared to GAT.50
Roberts et al mentioned that any corneal refractive procedure will cause a biomechanical response that will influence IOP measurements made by the CVS.51 This is seen specifically with LASIK wherein flap creation and removal of stromal tissue changes the ability of the cornea to absorb or dissipate energy or could cause an asymmetric corneal response to applanation. After myopic LASIK, the central cornea will be thinner per diopter of correction. This will cause falsely low IOP measurements and post-LASIK CCT may not be addressed. Our study showed that the percentage change in CVS-bIOP had a weak relationship with percentage change in MRSE. We, therefore, investigated that MRSE will dictate the ablation depth, hence the “stiffness” of the cornea postoperatively. Thus, the behavior of the relationship reflects the biomechanical correction of the CVS-bIOP in LASIK.
CVS, particularly the bIOP it measures, is a very promising technology because it has a built-in formula to compensate for factors that we observe have been influencing the consistency of GAT measurements, namely CCT and Km. Knowledge about the association between refractive error change and the changes in corneal biomechanics should further be investigated that could provide more insights into the relationship we found in our study. CVS-bIOP can become the new reference standard but it needs additional data and analysis to develop a more robust database and the clinical experience of surgeons to determine normal and abnormal cut-off values which can be useful in treatment decision-making.
Of interest to us is if there is an influence in IOP measurements in eyes with a flap (LASIK) versus eyes without a flap (PRK). There were lesser decreases in IOP after PRK compared to LASIK with all three tonometers. With regard to changes in IOP measurements from preoperative to postoperative values, GAT and CATS showed a high correlation whether in LASIK or PRK. A large decrease in GAT after surgery will also yield a large decrease in CATS in both LASIK and PRK eyes. CVS-bIOP showed low correlation to GAT or CATS in LASIK eyes and no correlation to GAT or CATS in PRK eyes. Even if there is a large decrease in GAT and CATS values from preoperative to postoperative measurements, the decrease in IOP in LASIK eyes will be small or the decrease may not even manifest in PRK eyes when the CVS-bIOP was used. This leads us to conclude that CVS-bIOP is not as sensitive to changes in IOP measurements and this is more evident in PRK eyes wherein structurally, it may be more robust compared to post-LASIK eyes. There is a need to consider the biomechanical difference of LASIK and PRK on IOP measurements using GAT, CATS and CVS-bIOP and this should be the subject of further investigation.
The advantage of the current study informed practitioners and researchers on the modalities to consider in the measurement of intraocular pressure among post refractive patients. There are still many questions to be answered regarding the biomechanical properties of the cornea which is not within the scope of this study. Although CVS-bIOP is designed to take into account corneal biomechanics, its clinical usefulness requires continuing research. Corneal biomechanics therefore can be a significant confounding factor for IOP measurement that should be considered in clinical decision-making.
The present study had several limitations. First, this was a retrospective study with a relatively small sample size limited to myopic LASIK and PRK only. Second, the IOP measurements were done once, not in a masked fashion and recorded without controlling for diurnal variation and intraobserver and interobserver variability. Perhaps it may be worthwhile to include corneal volume, corneal hysteresis, corneal stiffness and other corneal biomechanical properties in future analyses.
Conclusion
Two novel tonometers were evaluated and compared with GAT in measuring IOP before and after laser vision correction. CATS recorded the highest IOP preoperatively and postoperatively while GAT had the largest decrease in IOP after LASIK and PRK. CVS-bIOP gave the lowest change and had the best agreement between preoperative and postoperative measurements among the three tonometers. PRK had lesser IOP change compared to LASIK probably due to the absence of a corneal flap and lesser change in corneal biomechanics. Percentage change in corneal thickness, corneal curvature and refractive correction were not found to be directly correlated to IOP measurements. CVS-bIOP had minimal correlation to GAT and CATS in post-LASIK eyes and no correlation to GAT and CATS in PRK eyes. Our findings in this study suggest that factors affecting IOP measurements other than CCT, keratometry and refractive error correction were being compensated for in CVS-bIOP measurements, and this could be corneal biomechanics.
Abbreviations
IOP, Intraocular pressure; LASIK, Laser assisted keratomileusis; PRK, Photorefractive keratectomy; MRSE, Manifest refraction spherical equivalent; CCT, Central corneal thickness; Km, Mean corneal curvature; GAT, Goldmann applanation tonometer; CATS, Correcting applanation tonometer surface; CVS, Corvis ST tonometer; bIOP, biomechanically corrected intraocular pressure; TBI, Tomographic biomechanical Index; CBI, Corvis biomechanical Index; DCT, Dynamic contour tonometer; ORA, Ocular response analyzer.
Data Sharing Statement
The datasets used and analyzed in the current study are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
Approval and adherence to the tenets of the Declaration of Helsinki was assessed by the St. Cabrini Medical Center-Asian Eye Institute (SCMC-AEI) Review Committee and was conducted upon approval (ERC#2021-004, February 22, 2021). Since all data collected were retrospective, the requirement of the informed consent is waived by the review committee. The patient anonymity and confidentiality were and are protected and preserved with identifiable data omitted.
Acknowledgments
The authors thank the Asian Eye Institute for the support and guidance in making this paper.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Wang YX, Xu L, Wei WB, Jonas JB. Intraocular pressure and its normal range adjusted for ocular and systemic parameters. The Beijing Eye Study 2011. PLoS One. 2018;13(5). doi:10.1371/Journal.Pone.0196926
2. Yolcu U, Ilhan A, Tas A. Conventional intraocular pressure measurement techniques. In: wound healing - new insights into ancient challenges. Intech. 2016. doi:10.5772/64611
3. Aziz K, Friedman DS. Tonometers - which one should I use? Eye. 2018;32(5):931–937. doi:10.1038/S41433-018-0040-4
4. Singh P. Tonometry: an overview. Vol 13; 2014. Available from: Www.Iosrjournals.Orgwww.Iosrjournals.Org.
5. Messenio D, Ferroni M, Boschetti F. Goldmann tonometry and corneal biomechanics. Appl Sci. 2021;11(9):4025. doi:10.3390/App11094025
6. Kozobolis V, Konstantinidis A, Sideroudi H, Labiris G. The effect of corneal refractive surgery on glaucoma. J Ophthalmol. 2017;2017:1–8. doi:10.1155/2017/8914623
7. Konstantinidis A, Panagiotopoulou E-K, Panos GD, Sideroudi H, Mehmet A, Labiris G. The effect of antiglaucoma procedures (trabeculectomy vs. ex-PRESS glaucoma drainage implant) on the corneal biomechanical properties. J Clin Med. 2021;10(4):802. doi:10.3390/Jcm10040802
8. Liu J, Roberts CJ. Influence of corneal biomechanical properties on intraocular pressure measurement: quantitative analysis. J Cataract Refract Surg. 2005;31(1):146–155. doi:10.1016/J.Jcrs.2004.09.031
9. Whitacre MM, Stein R. Major review sources of error with use of Goldmann-type tonometers. Survey Ophthalmol. 1993;38:1–30. doi:10.1016/0039-6257(93)90053-a
10. Sosuan GMN, Yap-Veloso MIR. Central corneal thickness among Filipino patients in an ambulatory eye surgery center using anterior segment optical coherence tomography. Clin Ophthalmol. 2021;15:2653–2664. doi:10.2147/OPTH.S320281
11. Francis BA, Varma R, Chopra V, Lai MY, Shtir C, Azen SP. Intraocular pressure, central corneal thickness, and prevalence of open-angle glaucoma: the Los Angeles Latino Eye Study. Am J Ophthalmol. 2008;146(5):741–746. doi:10.1016/J.Ajo.2008.05.048
12. Lleo A, Marcos A, Calatayud M, Alonso L, Rahhal SM, Sanchis-Gimeno JA. The relationship between central corneal thickness and Goldmann applanation tonometry. Clin Exp Optometry. 2003;86:104–108. doi:10.1111/j.1444-0938.2003.tb03068.x
13. Stodtmeister R. Applanation tonometry and correction according to corneal thickness. Acta Ophthalmologica Scandinavica. 1998;76:319–324. doi:10.1034/j.1600-0420.1998.760313.x
14. Ehlers N, Bramsen T, Sperling S. Applanation tonometry and central corneal thickness. Acta Ophthalmol. 2009;53(1):34–43. doi:10.1111/J.1755-3768.1975.Tb01135.X
15. Gunvant P, James O’leary D, Baskaran M, Broadway DC, Watkins RJ, Vijaya L. Evaluation of tonometric correction factors. J Glaucoma. 2005;14:337–343. doi:10.1097/01.ijg.0000176940.81799.33
16. Feltgen N, Leifert D, Funk J, Feltgen N, Leifert D, Funk J. Correlation between central corneal thickness, applanation tonometry, and direct intracameral IOP readings. Vol 85; 2001. Available from: Www.Bjophthalmol.Com.
17. De Bernardo M, Cembalo G, Rosa N. Reliability of intraocular pressure measurement by Goldmann applanation tonometry after refractive surgery: a review of different correction formulas. Clin Ophthalmol. 2020;14:2783–2788. doi:10.2147/OPTH.S263856
18. Shortt AJ, Allan BDS, Evans JR. Laser-Assisted In-Situ Keratomileusis (LASIK) Versus Photorefractive Keratectomy (PRK) for myopia. Cochrane Database Syst Rev. 2013;2013(1). doi:10.1002/14651858.CD005135.Pub3
19. Schallhorn JM, Schallhorn SC, Ou Y. Factors that influence intraocular pressure changes after myopic and hyperopic lasik and photorefractive keratectomy: a large population study. In: Ophthalmology. Vol. 122. Elsevier Inc.; 2015:471–479. doi:10.1016/J.Ophtha.2014.09.033
20. Helmy H, Hashem O. Intraocular pressure calculation in myopic patients after laser-assisted in situ keratomileusis. Clin Ophthalmol. 2020;14:509–516. doi:10.2147/OPTH.S239329
21. Svedberg H, Chen E, Hamberg-Nyström H. Changes in corneal thickness and curvature after different excimer laser photorefractive procedures and their impact on intraocular pressure measurements. Graefes Arch Clin Exp Ophthalmol. 2005;243(12):1218–1220. doi:10.1007/S00417-005-0072-X
22. McCafferty SJ, Tetrault K, Mccolgin A, Chue W, Levine J, Muller M. modified Goldmann prism intraocular pressure measurement accuracy and correlation to corneal biomechanical metrics: multicentre randomised clinical trial. Br J Ophthalmol. 2019;103(12):1840–1844. doi:10.1136/Bjophthalmol-2018-313470
23. McCafferty S, Tetrault K, Mccolgin A, Chue W, Levine J, Muller M. Intraocular pressure measurement accuracy and repeatability of a modified Goldmann prism: multicenter randomized clinical trial. Am J Ophthalmol. 2018;196:145–153. doi:10.1016/J.Ajo.2018.08.051
24. McCafferty SJ, Enikov ET, Schwiegerling J, Ashley SM. Goldmann tonometry tear film error and partial correction with a shaped applanation surface. Clin Ophthalmol. 2018;12:71–78. doi:10.2147/OPTH.S152492
25. McCafferty S, Lim G, Duncan W, et al. Goldmann tonometer error correcting prism: clinical evaluation. Clin Ophthalmol. 2017;11:835–840. doi:10.2147/OPTH.S135272
26. McCafferty S, Lim G, Duncan W, Enikov E, Schwiegerling J. Goldmann tonometer prism with an optimized error correcting applanation surface. Transl Vision Sci Technol. 2016;5(5). doi:10.1167/Tvst.5.5.4
27. Bao FJ, Huang ZX, Huang JH, et al. Clinical evaluation of methods to correct intraocular pressure measurements by the Goldmann applanation tonometer, ocular response analyzer, and corvis ST tonometer for the effects of corneal stiffness parameters. J Glaucoma. 2016;25(6):510–519. doi:10.1097/IJG.0000000000000359
28. Chen KJ, Joda A, Vinciguerra R, et al. Clinical evaluation of a new correction algorithm for dynamic scheimpflug analyzer tonometry before and after laser in situ keratomileusis and small-incision lenticule extraction. J Cataract Refract Surg. 2018;44(5):581–588. doi:10.1016/J.Jcrs.2018.01.023
29. Lee H, Roberts CJ, Kim TI, Ambrósio R, Elsheikh A, Yong Kang DS. Changes in biomechanically corrected intraocular pressure and dynamic corneal response parameters before and after transepithelial photorefractive keratectomy and femtosecond laser–assisted laser in situ keratomileusis. J Cataract Refract Surg. 2017;43(12):1495–1503. doi:10.1016/J.Jcrs.2017.08.019
30. Chen S, Lopes BT, Huang W, et al. Effectiveness of 4 tonometers in measuring IOP after femtosecond laser-assisted LASIK, SMILE, and transepithelial photorefractive keratectomy. J Cataract Refract Surg. 2020;46(7):967–974. doi:10.1097/J.Jcrs.0000000000000204
31. Bao F, Huang W, Zhu R, et al. Effectiveness of the Goldmann applanation tonometer, the dynamic contour tonometer, the ocular response analyzer and the corvis ST in measuring intraocular pressure following FS-LASIK. Curr Eye Res. 2020;45(2):144–152. doi:10.1080/02713683.2019.1660794
32. Joda AA, Shervin MMS, Kook D, Elsheikh A. Development and validation of a correction equation for corvis tonometry. Comput Methods Biomechan Biomed Eng. 2015;19(9):943–953. doi:10.1080/10255842.2015.1077515
33. Vinciguerra R, Elsheikh A, Roberts CJ, et al. Influence of pachymetry and intraocular pressure on dynamic corneal response parameters in healthy patients. J Refract Surg. 2016;32(8):550–561. doi:10.3928/1081597X-20160524-01
34. Salouti R, Bagheri M, Shamsi A, Zamani M, Ghoreyshi M, Hossein Nowroozzadeh M. Corneal parameters in healthy subjects assessed by corvis ST. J Ophthal Vision Res. 2020;15(1):24–31. doi:10.18502/Jovr.V15i1.5936
35. Margarita Lat-Luna ML, Guerrero PI. Correlation of central corneal thickness and Goldmann applanation tonometry among Filipinos. Ophthalmology. 2004;29:79–82.
36. Stevens S. Nurse advisor to the community eye. Health J. 2007;20:44–45.
37. Ceruti P, Morbio R, Marraffa M, Marchini G. Comparison of Goldmann applanation tonometry and dynamic contour tonometry in healthy and glaucomatous eyes. Eye. 2009;23(2):262–269. doi:10.1038/Sj.Eye.6703102
38. Shafiq I. Influence of Central Corneal Thickness (CCT) on Intraocular Pressure (IOP) measured with Goldmann Applanation Tonometer (GAT) in normal individuals. Pak J Ophthalmol. 2008;24:89.
39. Margarita Lat-Luna ML, Guerrero PI, Vincent Policarpio Flores JD, Epi M, Margarita Lat-Luna M. Correlation of central corneal thickness and Goldmann applanation tonometry among Filipinos. Ophthalmology. 2004;29:79–82.
40. Marjanović I, Kontić D, Hentova-Senćanić P, Marković V, Božić M. Correlation between central corneal thickness and intraocular pressure in various age groups. Srp Arh Celok Lek. 2010;138(5–6):279–286. doi:10.2298/SARH1006279M
41. Kyei S, Assiamah F, Kwarteng MA, Gboglu CP. The association of central corneal thickness and intraocular pressure measures by non-contact tonometry and Goldmann applanation tonometry among glaucoma patients. Ethiop J Health Sci. 2020;30(6):999–1004. doi:10.4314/Ejhs.V30i6.18
42. Mark HH. Corneal curvature in applanation tonometry. Am J Ophthalmol. 1973;76(2):223–224. doi:10.1016/0002-9394(73)90164-5
43. Gunvant P, Baskaran M, Vijaya L, et al. Effect of corned parameters on measurements using the pulsatile ocular blood flow tonograph and Goldmann applanation tonometer. Br J Ophthalmol. 2004;88(4):518–522. doi:10.1136/Bjo.2003.019331
44. Rask G, Behndig A. Effects of corneal thickness, curvature, astigmatism and direction of gaze on Goldmann applanation tonometry readings. Ophthalmic Res. 2005;38(1):49–55. doi:10.1159/000089762
45. Kaufmann C, Bachmann LM, Thiel MA. Comparison of dynamic contour tonometry with Goldmann applanation tonometry. Investig Ophthalmol Visual Sci. 2004;45(9):3118–3121. doi:10.1167/Iovs.04-0018
46. Nomura H, Ando F, Niino N, Shimokata H, Miyake Y. The relationship between intraocular pressure and refractive error adjusting for age and central corneal thickness. Ophthalmic and Physiological Optics. 2004;24:41–45. doi:10.1046/j.1475-1313.2003.00158.x
47. Yassin SA, Al-Tamimi ER. Age, gender and refractive error association with intraocular pressure in healthy Saudi participants: a cross-sectional study. Saudi J Ophthalmol. 2016;30(1):44–48. doi:10.1016/J.Sjopt.2015.11.007
48. Bonomi L, Mecca E, Massa F. Intraocular Pressure in Myopic Anisometropia. Vol. 5. Dr W. Junk Pubhshers; 1982.
49. Nakao Y, Kiuchi Y, Okumichi H, Mohan RR. Evaluation of biomechanically corrected intraocular pressure using corvis ST and comparison of the corvis ST, noncontact tonometer, and Goldmann applanation tonometer in patients with glaucoma. PLoS One. 2020;15:e0238395. doi:10.1371/Journal.Pone.0238395
50. Ye Y, Yang Y, Fan Y, Lan M, Yu K, Yu M. Comparison of biomechanically corrected intraocular pressure obtained by corvis ST and Goldmann applanation tonometry in patients with open-angle glaucoma and ocular hypertension. J Glaucoma. 2019;28(10):922–928. doi:10.1097/IJG.0000000000001348
51. Roberts C. Biomechanics of the cornea and wavefront-guided laser refractive surgery. J Refract Surg. 2002;18:589–592. doi:10.3928/1081-597X-20020901-18
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


