Back to Journals » Clinical Ophthalmology » Volume 17
Comparison of Surgical Outcomes for Uncomplicated Primary Retinal Detachment Repair
Authors Heydinger S , Ufret-Vincenty R , Robertson ZM , He YG, Wang AL
Received 3 February 2023
Accepted for publication 10 March 2023
Published 17 March 2023 Volume 2023:17 Pages 907—915
DOI https://doi.org/10.2147/OPTH.S405913
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Stanton Heydinger,1 Rafael Ufret-Vincenty,2,3 Zachary M Robertson,2,3 Yu-Guang He,2,3 Angeline L Wang2,3
1University of Texas Southwestern Medical School, University of Texas Southwestern, Dallas, TX, USA; 2Department of Ophthalmology, University of Texas Southwestern, Dallas, TX, USA; 3Department of Ophthalmology, Parkland Hospital, Dallas, TX, USA
Correspondence: Stanton Heydinger, Department of Ophthalmology, University of Texas Southwestern, 5323 Harry Hines Blvd, Dallas, TX, USA, Tel +1 816-500-9088, Email [email protected]
Purpose: To compare the outcomes of primary uncomplicated rhegmatogenous retinal detachment (RRD) repair using pars plana vitrectomy (PPV), scleral buckling (SB), or combined scleral buckling with vitrectomy (SB/PPV).
Patients and Methods: Single-institution, retrospective, observational study of 179 patients with primary RRD managed at a large academic hospital system. We excluded patients with less than 6 months of follow-up, previous vitrectomy or buckle, giant retinal tears, aphakia, recurrent forms of RRD, or extensive proliferative vitreoretinopathy (Grade C or worse) documented on exam or requiring membrane peel. Outcome measures included primary anatomical success at 6 months, functional success defined as BCVA ≥ 20/200, and best corrected visual acuity (BCVA) using logMAR scoring. Subgroup analysis was performed in the following patient groups: phakic, pseudophakic, inferior detachments, and prior pneumatic retinopexy.
Results: Primary anatomical success was achieved in 145 of 179 eyes (81.0%), with SB/PPV showing a significantly greater success rate (p = 0.046) when compared to SB and PPV. Functional success was achieved in 137 of the 145 anatomically successful eyes (94.5%), with values ranging between 92% and 97% amongst the interventions (p = 0.552). No difference was found in final BCVA (p = 0.367). Patients with inferior detachment had an odds ratio of 2.15 for primary anatomic failure. Prior pneumatic retinopexy did not significantly affect any of the primary outcomes.
Conclusion: SB/PPV yielded a significantly better primary anatomical success rate when compared to SB and PPV. Functional success and final BCVA was similar amongst the interventions. Inferior detachments were associated with worse primary anatomic outcomes. Prior pneumatic retinopexy did not significantly affect surgical outcomes.
Keywords: anatomical success, retina, scleral buckling, vitrectomy
Introduction
The mainstay of treatment for uncomplicated rhegmatogenous retinal detachment (RRD) is surgical repair. Cases that are not ideally suited for pneumatic retinopexy can be repaired with scleral buckling (SB) surgery, pars plana vitrectomy (PPV), or a combined procedure (SB/PPV).1,2 Scleral buckling is performed by indenting the eyeball with a band, tire, or sponge that supports the tear externally.2,3 This external support leads to reduction in the magnitude of vitreous traction applied on the retina. Pars plana vitrectomy is conducted using small surgical instruments that allow for direct passage through the pars plana into the vitreous cavity.3,4 The vitreous humour is removed, subretinal fluid is drained, breaks are sealed with laser, and a gas or oil tamponade is added into the eye.2 There is currently debate surrounding if either method is superior amongst various patient populations, or if a combined procedure may yield the best results.
Over the past 20 years, PPV has overtaken SB as the primary surgical intervention for uncomplicated RRD in all patients due to technical advances made in vitrectomy.5,6 Combining the procedures to perform SB/PPV has increased in frequency in order to maximize the benefits of both procedures for phakic patients.7 While these trends have been observed, it has not been shown consistently that either procedure results in superior surgical outcomes. Our study investigates the surgical outcomes of SB versus PPV versus SB/PPV through the metrics of single-operation anatomical success, functional success, and best-corrected visual acuity.
Materials and Methods
Retrospective, observational study of 179 consecutive patients at an academic training institution, including a large county hospital and a large university hospital, treating a diverse, urban population with primary RRD repaired via SB, PPV, or SB/PPV between July 2015 and June 2020. Patients were identified through procedure codes for scleral buckling (67107) and pars plana vitrectomy with or without additional scleral buckling (67108). Preoperative patient characteristics and demographics were obtained and analyzed while primary success rates, final anatomical success rates, functional success rates and best corrected visual acuity (BCVA) were compared amongst surgical interventions.
Primary success was defined as restoring the anatomical integrity of the retina following one surgical intervention at a minimum follow-up of 6 months after surgery. Functional success was defined as measuring a BCVA of 20/200 or better. BCVA was obtained using the Snellen eye chart and converted to logarithm of minimum angle of resolution (logMAR) for comparison between groups. These outcome measures were evaluated at 6 months amongst surgical interventions and further analysis was performed separating groups by lens status. Final anatomical success was defined as sustained anatomical integrity following one or more procedures. Following final anatomical success, average number of surgeries needed for anatomical success was calculated for each surgical intervention.
We excluded patients with less than 6 months of follow-up and those with incomplete clinical records, prior vitrectomy or scleral buckle, giant retinal tears, aphakia, recurrent forms of RRD or extensive proliferative vitreoretinopathy documented on exam (grade C or worse) or requiring a membrane peel. The following preoperative patient characteristics were recorded: age, gender, laterality, duration of RRD symptoms, prior laser and/or pneumatic retinopexy, myopic status, lens status, number of tears observed, tear location, detachment location, macular involvement, Snellen best-corrected visual acuity (BCVA).
All patients underwent either SB, PPV or a combined SB/PPV for their primary intervention. Surgeries were performed by 9 different surgeons and the choice of intervention was made through patient-centered decision-making. The scleral buckling procedure used a variety of band, tire and sleeve elements based on surgeon preference. PPV operations used either 23-gauge or 25-gauge instrumentation. The extent of endolaser (at the existing retinal tear, covering the extent of the detachment, or circumferentially for 180° or 360°), choice of tamponade agent (C3F8 gas, SF6 gas or silicone oil), and method of fluid drainage (through the original break, posterior retinotomy, or with the help of perfluoron heavy liquid) was made at the operating surgeon’s discretion.
Statistics were calculated for results using multiple methods. Comparison between surgical interventions underwent ANOVA testing for quantitative data and Fisher Exact Test for qualitative measures.
Results
Preoperative Features of All Eyes
A total of 501 patients were initially identified based on procedure codes 67107 and 67108. After applying inclusion and exclusion criteria, 179 patients with primary RRD who underwent SB, PPV or SB/PPV were included in the study. Of the 322 excluded patients, the most common exclusion criteria applied were lack of follow-up and non-rhegmatogenous retinal detachments. Preoperative characteristics are listed in Table 1. The mean age at presentation was 57.4 years (standard deviation, 14.5 years) and the mean follow-up duration was 19.9 months (standard deviation, 13.5 months). Most patients included were male (67.0%). Most eyes operated on were myopic (60.9%), with 19% of the patient population presenting with high myopia (−6 diopters or higher). Symptoms most often presented with a duration between 1 week to 1 month (41.9%). The vast majority of eyes were deemed to have a posterior vitreous detachment (74.3%). Lattice degeneration was noted in 65 patients (36.3%). Most patients still possessed their natural lens (63.1%). The detachment involved the macula in 125 patients (69.8%). The RRD involved the inferior retina in 124 eyes (69.3%), with 73 patients having a tear visualized inferiorly (40.8%). Ten patients were classified as having a total detachment (5.6%). When reviewing prior interventions, it is worth noting that 62 patients had previously received laser retinopexy (34.6%) and 33 had previously undergone pneumatic retinopexy (18.4%).
 |
Table 1 Preoperative Characteristics of All Eyes (n = 179) |
Preoperative Features Amongst Surgical Interventions
Preoperative characteristics are stratified by surgical intervention in Table 2. In our study, 55% of patients received PPV, 28% received SB, and 17% received SB/PPV. Patients receiving PPV as their primary surgical intervention were significantly older (p < 0.001) than those who underwent SB or SB/PPV, with average age of 62.5 compared to 50.0 and 54.3, respectively. SB (p < 0.0001) and SB/PPV (p = 0.01) had a significantly higher proportion of phakic patients when compared to PPV alone. Patients designated to undergo SB had better preoperative best-corrected visual acuity when compared to SB/PPV (p = 0.038). Most other preoperative characteristics including laterality, gender distribution, duration of symptoms, myopic status, number of tears and involvement of the macula were similarly distributed among the study groups.
 |
Table 2 Characteristics by Surgical Intervention (n = 179) |
Intraoperative Features of PPV
Intraoperative features of 129 eyes receiving PPV or SB/PPV are recorded in Table 3. PPV was significantly more likely than combined SB/PPV to use 25-gauge instrumentation (p = 0.03) versus 23-gauge. Subretinal fluid drainage was completed by creation of a posterior retinotomy more frequently in SB/PPV cases when compared to PPV alone (p = 0.02). Similarly, endolaser treatment was more likely to be limited to the causative retinal tear (in addition to posterior retinotomy if present) rather than the entire peripheral extent of the detachment or 360 degrees circumferentially in SB/PPV cases when compared to PPV alone (p = 0.01). Both surgical interventions tended to use C3F8 as the tamponade of choice.
 |
Table 3 Intraoperative Features of Surgeries Including PPV (n = 129) |
Outcome Measures Amongst Surgical Interventions
Outcome measures relating to primary anatomical success, functional success, and BCVA are recorded by surgical intervention in Table 4. SB/PPV showed significantly greater anatomical success (p = 0.046) when compared to SB and PPV. Functional success ranged between 92.7% and 97.1% amongst the three interventions, with SB showing a marginally better rate than SB/PPV and PPV, which was not significant (p = 0.552). SB resulted in the best final BCVA, but the differences were not statistically significant (p = 0.367). It is worth noting that the SB group started with a significantly better initial BCVA when compared to SB/PPV (p = 0.038). Final anatomical success rates (defined as success following more than one surgical intervention) were extremely similar amongst groups, ranging from 98% to 100%. Average number of surgeries to achieve anatomical success were as follows: SB/PPV (1.10), PPV (1.18), SB (1.29). Both PPV (44%) and SB/PPV (64.5%) were associated with significantly more cataract progression when compared to SB (10%) (p < 0.00001).
 |
Table 4 Outcomes by Surgical Intervention (n = 179) |
Outcome Measures Amongst Phakic Patients
Outcome measures were stratified for all 113 phakic patients by surgical intervention in Table 5. Within the phakic patient population: 41% received PPV alone, 39% received SB alone, and 20% received combined SB/PPV. For phakic patients, combined SB/PPV showed the best results for primary anatomical success (87% success vs 84.8% for PPV and 70.5% for SB). SB/PPV also had the best functional success (100% vs 92.3% for PPV and 96.8% for SB). SB led to the best final BCVA. However, none of these differences reached statistical significance.
 |
Table 5 Outcome Measures for Phakic Eyes |
Outcome Measures Amongst Pseudophakic Patients
Outcome measures were stratified for pseudophakic patients by surgical intervention in Table 6. Within the pseudophakic patient population: 79% received PPV, 12% received combined SB/PPV, and 9% received SB. SB/PPV yielded the best results for primary anatomical success (100% vs 82.7% for PPV and 66.7 for SB). SB resulted in the best functional success (100% vs 93% for PPV and 87.5% for SB/PPV), and final BCVA (logMAR of 0.09 vs 0.36 for PPV and 0.60 for SB/PPV). However, none of these differences were statistically significant (see Table 6).
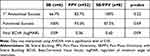 |
Table 6 Outcome Measures for Pseudophakic Eyes |
Success Rates Amongst Patients with Inferior Detachments
As seen in Table 1, 69.3% of patients presented with a retinal detachment involving the inferior portion of the retina. However, these patients represented 81.3% of the patients who did not attain primary anatomical success. Within this population, there was a primary anatomical success rate of 79%. For the rest of the population, the primary anatomical success rate was 89%. An odds ratio of 2.15 was calculated for primary anatomical failure in patients with inferior detachments meaning this preoperative feature had a negative impact on anatomical success. These findings of inferior detachments over-representing failed surgeries were noted and further stratified by surgical intervention. For these patients with detachments involving the inferior retina, we calculated primary success rates of: SB/PPV (88%), PPV (80%), and SB (71%). The differences amongst surgical groups were not deemed statistically significant.
Success Rates Amongst Patients with Prior Pneumatic Retinopexy
Among the PPV group, when comparing patients (number of patients/total number of PPV) who had undergone unsuccessful pneumatic retinopexy prior to PPV versus those who went straight to PPV (number of patients/total number of PPV), there was no significant difference in primary anatomical success rates (p = 0.30), functional success (p = 0.20), of final BCVA (p = 0.14). This data suggests that history of failed pneumatic retinopexy did not negatively impact patient outcomes and was not a negative predictive factor for surgical success by our outcome measures. There were too few patients in the combined PPV/SB group to compare outcomes for patients who previously failed pneumatics.
Comparing Use of Tamponade Agents
There was no significant difference in the number of patients receiving each tamponade agent (SF6, C3F8 or SO) between PPV and SB/PPV groups as seen in Table 3. Preoperative characteristics also were similar between groups. Primary anatomic success rates were similar between the three tamponade agents ranging between 86% and 90%.
Discussion
The combined surgical approach (SB/PPV) yielded the greatest primary anatomical success rate (p = 0.046) amongst the interventions. In a recent meta-analysis including nearly 3000 eyes, the combined procedure was shown to be equally efficacious with regard to primary anatomical success when compared to SB or PPV alone.8 Nonetheless, Totsuka et al calculated an odds ratio of 1.70 for primary anatomical success when comparing combined SB/PPV to PPV in a ten study meta-analysis.9 Further supporting this, multiple studies have shown greater primary success rate for SB/PPV in comparison to PPV alone.8,10,11 The primary anatomical success rates noted in our study for SB/PPV (90.3%), PPV (83.7%), and SB (70.0%) were on par with success rates published by other groups. Success rates have ranged between 64% and 89% for PPV, 53% and 91% for SB, and 86% and 88% for combined SB/PPV.4,10–15 We were unable to significantly differentiate final anatomical success rates as all of the surgical interventions showed highly successful results; this is consistent with past research where final success rates have ranged from 90% to 100%.4,11,13
SB was calculated to have the greatest final best-corrected visual acuity of the three surgical interventions (p = 0.367), although results were similar amongst the interventions. Final BCVA measured in logMAR scoring for comparison were: 0.34 for SB, 0.41 for PPV, and 0.49 for SB/PPV. Our results are similar to the findings of Heimann et al who reported better final BCVA in patients who underwent SB, showing a benefit with regard to BCVA in phakic patients.4
All interventions resulted in a similar improvement in BCVA compared to baseline, suggesting that the differences in final acuity may be mostly due to differences in baseline BCVA. Both the SB/PPV group and PPV group were more likely to develop cataracts (p < 0.00001) when compared to SB, which may also contribute to the better final BCVA in SB patients. Following subgroup analysis, results for pseudophakic patients lacked an adequate number of patients to draw significant conclusions. In phakic patients, no differences were noted amongst the interventions.
Functional success was defined as the percentage of eyes with BCVA greater than or equal to 20/200 at 6-months. Patients who had not achieved primary anatomical success were excluded from this measure. All three surgical interventions showed high functional success rates (97.1% for SB, 96.4% for SB/PPV, and 92.7% for PPV). There was no difference between the groups (p = 0.552). Our functional success rates were on par with other studies, with one study finding the best results amongst SB patients, as seen in our patients.15,16
For patients with inferior detachments, we were unable to differentiate a superior surgical approach in regards to primary anatomical success (p = 0.26). We believe this result is a byproduct of our study not having enough patients in this group to delineate this metric. However, Inferior detachments were associated with worse primary anatomical outcomes with a calculated odds ratio of 2.15 for primary failure. Inferior detachments might be more difficult to manage due to the anatomical location being more prone to the effects of postoperative PVR. We were unable to determine if any surgical intervention was superior for management of these cases, although SB/PPV showed the greatest primary anatomical success rate (88%). It has previously been suggested that PPV/SB offers higher success rates when compared to PPV for the management of patients with inferior detachments.17
When studying patients who had prior pneumatic retinopexy before surgical intervention, there was a notable cohort in the PPV group. There were not enough cases in the SB/PPV or SB groups to draw meaningful conclusions. Analysis of our data showed that prior pneumatic retinopexy was not a negative predictive factor for surgical success in patients who underwent PPV. All outcome measures including primary anatomical success rates (p = 0.30), functional success (p = 0.20), and final BCVA (p = 0.14) were not significantly different between groups. This is agreeable with data seen in other studies that showed similar rates of reattachment and final BCVA between patients who had and had not previously undergone pneumatic retinopexy.18
Comparing the three tamponade agents used in this study (C3F8, SF6, Silicone Oil) revealed no difference in primary anatomical success rates. These tamponade agents have been compared in the literature extensively for macular hole repair and the data supports our results, that there has been no difference associated between the agents when comparing primary anatomical success.19
A trend toward PPV as the primary surgical intervention, with or without scleral buckling, was observed in this hospital system (72.1% of patients receiving PPV or SB/PPV). Over the past 20 years, PPV has overtaken SB as the primary surgical intervention for uncomplicated RRD in all patients due to technical advances made in vitrectomy.5,6 Falkner et al20 noted a similar overall trend moving towards vitrectomy as the primary intervention while shying away from scleral buckling regardless of lens status.
Population size was the primary limitation when drawing conclusions between interventions. Increasing the number of cases could be achieved by expanding the time frame of the study or including additional surgical locations.
Conclusion
In conclusion, combined scleral buckle/pars plana vitrectomy showed the greatest anatomical success rate of the three surgical interventions studied. SB had marginally better visual outcomes that could very well be attributed to variability in patient groups and cataract formation. All three procedures showed excellent functional outcomes. Given the substantially better primary anatomical success, our results support the use of SB/PPV.
Ethics Statement
This study has been approved through the University of Texas Southwestern IRB and granted the identification STU-2021-0302. Informed consent was obtained from study participants and this research followed the guidelines outlined in the Declaration of Helsinki.
Funding
The research in the manuscript was supported by Research to Prevent Blindness and NEI Core Grant P30EY030413.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Yorston D. Emergency management: retinal detachment. Commun Eye Health J. 2018;31(103):63.
2. Feltgen N, Walter P. Rhegmatogenous retinal detachment--an ophthalmologic emergency. Dtsch Arztebl Int. 2014;111(1–2):12–22. doi:10.3238/arztebl.2014.0012
3. Kuhn F, Aylward B. Rhegmatogenous retinal detachment: a reappraisal of its pathophysiology and treatment. Ophthalmic Res. 2014;51(1):15–31. doi:10.1159/000355077
4. Heimann H, Bartz-Schmidt KU, Bornfeld N, et al. Scleral buckling versus primary vitrectomy in rhegmatogenous retinal detachment: a prospective randomized multicenter clinical study. Ophthalmology. 2007;114(12):2142–2154. doi:10.1016/j.ophtha.2007.09.013
5. McLaughlin MD, Hwang JC. Trends in vitreoretinal procedures for medicare beneficiaries, 2000 to 2014. Ophthalmology. 2017;124(5):667–673. doi:10.1016/j.ophtha.2017.01.001
6. Fujii GY, De JE, Humayun MS, et al. A new 25-gauge instrument system for transconjunctival sutureless vitrectomy surgery. Ophthalmology. 2002;109(10):1807–1812. doi:10.1016/S0161-6420(02)01179-X
7. Ryan EH, Ryan CM, Forbes NJ, et al. Primary retinal detachment outcomes study report number 2: phakic retinal detachment outcomes. Ophthalmology. 2020;127(8):1077–1085. doi:10.1016/j.ophtha.2020.03.007
8. Popovic MM, Muni RH, Nichani P, et al. Pars plana vitrectomy, scleral buckle, and pneumatic retinopexy for the management of rhegmatogenous retinal detachment: a meta-analysis. Surv Ophthalmol. 2021;67(1):184–196. doi:10.1016/j.survophthal.2021.05.008
9. Totsuka K, Inui H, Roggia MF, et al. Supplemental scleral buckle in vitrectomy for the repair of rhegmatogenous retinal detachment: a systematic review of literature and meta-analysis. Retina. 2015;35(11):2423–2431. doi:10.1097/IAE.0000000000000797
10. Echegaray JJ, Vanner EA, Zhang L, et al. Outcomes of pars plana vitrectomy alone versus combined scleral buckling plus pars plana vitrectomy for primary retinal detachment. Ophthalmol Retina. 2021;5(2):169–175. doi:10.1016/j.oret.2020.09.013
11. Mehta S, Blinder KJ, Shah GK, et al. Pars plana vitrectomy versus combined pars plana vitrectomy and scleral buckle for primary repair of rhegmatogenous retinal detachment. Can J Ophthalmol. 2011;46(3):237–241. doi:10.1016/j.jcjo.2011.05.003
12. Soni C, Hainsworth DP, Almony A. Surgical management of rhegmatogenous retinal detachment: a meta-analysis of randomized controlled trials. Ophthalmology. 2012;120(7):1440–1447. doi:10.1016/j.ophtha.2012.12.033
13. Haugstad M, Moosmayer S, Bragadόttir R. Primary rhegmatogenous retinal detachment - surgical methods and anatomical outcome. Acta Ophthalmol. 2017;95(3):247–251. doi:10.1111/aos.13295
14. Orlin A, Hewing NJ, Nissen M, et al. Pars plana vitrectomy compared with pars plana vitrectomy combined with scleral buckle in the primary management of noncomplex rhegmatogenous retinal detachment. Retina. 2014;34(6):1069–1075. doi:10.1097/IAE.0000000000000050
15. Mohamed YH, Ono K, Kinoshita H, et al. Success rates of vitrectomy in treatment of rhegmatogenous retinal detachment. J Ophthalmol. 2016;2016:2193518. doi:10.1155/2016/2193518
16. Wong CW, Wong WL, Yeo IY, et al. Trends and factors related to outcomes for primary rhegmatogenous retinal detachment surgery in a large asian tertiary eye center. Retina. 2014;34(4):684–692. doi:10.1097/IAE.0b013e3182a48900
17. Starr MR, Obeid A, Ryan EH, et al. Retinal detachment with inferior retinal breaks: primary vitrectomy versus vitrectomy with scleral buckle (PRO study report No 9). Retina. 2021;41(3):525–530. doi:10.1097/IAE.0000000000002917
18. Demircan A, Alkın Z, Cakir I, et al. Comparison of pars plana vitrectomy for retinal detachment after failed pneumatic retinopexy and primary pars plana vitrectomy. J francais d’ophtalmologie. 2019;42(2):146–152. doi:10.1016/j.jfo.2018.09.004
19. Hecht I, Mimouni M, Blumenthal E, et al. Sulfur Hexafluoride (SF6) versus Perfluoropropane (C3F8) in the intraoperative management of macular holes: a systematic review and meta-analysis. J Ophthalmol. 2019;2019:1820850. doi:10.1155/2019/1820850
20. Falkner-Radler CI, Myung JS, Moussa S, et al. Trends in primary retinal detachment surgery: results of a Bicenter study. Retina. 2011;31(5):928–936. doi:10.1097/IAE.0b013e3181f2a2ad
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
