Back to Journals » Clinical Interventions in Aging » Volume 13
Comparison of sevoflurane and desflurane on effect-site concentration of remifentanil for preventing anesthetic emergence cough in elderly female patients undergoing laparoscopic cholecystectomy
Authors Kim HY, Moon YR, Seok S, Kim B, Kim JE, Lee SY
Received 18 May 2018
Accepted for publication 24 July 2018
Published 13 September 2018 Volume 2018:13 Pages 1769—1777
DOI https://doi.org/10.2147/CIA.S174626
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Richard Walker
Ha Yeon Kim,1 Yeo Rae Moon,2 Suhyun Seok,1 Bora Kim,1 Ji Eun Kim,1 Sook Young Lee1
1Department of Anesthesiology and Pain Medicine, Ajou University School of Medicine, Suwon, Republic of Korea; 2Office of Biostatistics, Ajou Research Institute for Innovation Medicine, Ajou University School of Medicine, Suwon, Republic of Korea
Purpose: Among inhalational anesthetics, desflurane is widely believed to provoke upper airway irritation including coughing and laryngospasm. Remifentanil has been generally used to prevent cough due to its unique pharmacodynamics. However, there was no study that compared optimal remifentanil effect-site concentration (Ce) to prevent emergence cough according to the type of inhalational agent in elderly female patients. Thus, we investigated the Ce of remifentanil for preventing cough during emergence from sevoflurane and desflurane anesthesia in elderly female patients.
Methods: Forty-three female patients between 60 and 75 years of age undergoing laparoscopic cholecystectomy were randomly allocated to sevoflurane group (n=22) or desflurane group (n=21). The optimal remifentanil Ce using target-controlled infusion for 50% of patients (EC50) and 95% of patients (EC95) was assessed by Dixon’s up-and-down method or isotonic regression method with a bootstrapping approach.
Results: By Dixon’s up-and-down method, the EC50 of remifentanil in sevoflurane group (2.08±0.47 ng/mL) was comparable with that in desflurane group (2.25±0.40 ng/mL) (P=0.385). The EC50 (83% CIs) and EC95 (95% CIs) by isotonic regression also did not show significant difference between two groups [2.06 (1.45–2.23) and 2.46 (2.35–2.48) ng/mL in sevoflurane group and 2.14 (1.45–2.56) and 2.88 (2.47–2.98) ng/mL in desflurane group, respectively].
Conclusion: There was no difference in the remifentanil Ce to prevent emergence cough between sevoflurane and desflurane anesthesia. Therefore, the clinicians may not need to adjust the remifentanil Ce to prevent emergence cough according to inhalational agents in elderly female patients.
Keywords: aging, cough, inhalational anesthetics, opioid, women
Introduction
Cough is a normal reaction for removing foreign body and secretion from airway. During emergence from general anesthesia, cough is caused by stimulation of the endotracheal tube, inhalational agents, or secretion.1 However, cough during emergence may lead to various adverse effects including increased intraocular and intracranial pressures, wound disruption, surgical site bleeding, and detrimental hemodynamic changes.2
To prevent emergence cough, several methods have been studied, such as intravenous opioid, dexmedetomidine, ketamine, or propofol infusion or lidocaine administration via intravenous or intraendotracheal tube cuff.3–6 Of these, remifentanil has been shown to prevent emergence cough due to its unique pharmacodynamics. It can control various levels of external stimuli even in patients with renal or hepatic dysfunction.7,8 However, remifentanil infusion may lead to respiratory depression, delayed emergence, nausea, and vomiting like other opioids.9 Therefore, it is important to find the optimal effect-site concentration (Ce) of remifentanil to have the cough inhibitory effect with minimal complications.
Various studies have been performed to evaluate the optimal Ce of remifentanil using target-controlled infusion (TCI) for preventing emergence cough.10–14 Cough reflex and a degree of airway irritation differed according to age15,16 and the type of anesthetic agent.17,18 Recently, the remifentanil Ce for preventing emergence cough showed difference according to sex.19–21 A study reported no difference of remifentanil Ce between sevoflurane and desflurane for preventing emergence cough in female patients aged 20–65 years.22 However, there has been no study that compared the optimal remifentanil Ce for preventing emergence cough according to the type of inhalational agent in elderly female patients. We hypothesized that the remifentanil Ce for preventing emergence cough in elderly female patients differs according to the type of inhalational agent because aging affects cough reflex.
The aim of the present study was to compare remifentanil Ce for preventing cough during emergence from sevoflurane and desflurane anesthesia in elderly female patients.
Methods
Study population
This study was approved by the Ajou University Hospital Institutional Review Board (AJIRB-MED-OBS-16-147) and registered at http://cris.nih.go.kr (KCT0002883). Written informed consent was obtained from all participants. Female patients with American Society of Anesthesiologists physical status of 1 or 2 at the age of 60–75 years who underwent scheduled laparoscopic cholecystectomy under general anesthesia were included from June 2016 to April 2018. Exclusion criteria were as follows: 1) those who had a body mass index (BMI) >30 kg/m2, uncontrolled hypertension or diabetes mellitus, or significant coronary disease; 2) those who had a history of recent upper airway infection within 2 weeks, chronic respiratory disease, difficult intubation, smoking, or chronic opioids dependency; 3) those who were illiterate, who were foreigners, who refused to participate in this study, or who lacked decision-making ability.
Anesthetic management
After arrival in the operating room without premedication, basic monitoring including pulse oximetry, electrocardiography, and noninvasive blood pressure cuff and bispectral index (BIS™ Quatro Sensor; Covidien, Boulder, CO, USA) was performed on the patient. After preoxygenation via facial mask, anesthesia was inducted with thiopental sodium 4–5 mg/kg and 1–5 ng/mL target concentration of remifentanil (Ultiva, GlaxoSmithKline, Brentford, UK) using TCI mode based on Minto’s pharmacokinetic model.23 After loss of consciousness, manual mask ventilation with 100% oxygen and inhalational agent according to the assigned group [sevoflurane (Sevorane®, Abbott Laboratories, Abbott Park, IL, USA) or desflurane (Suprane®, Baxter Healthcare, Deerfield, IL, USA)] was started and followed by rocuronium (1.0 mg/kg). After enough oxygenation and muscular relaxation, orotracheal intubation was done with a cuffed endotracheal tube of 7.0 mm inner diameter. Cuff pressure was adjusted at 20–25 mmHg using a hand pressure gauge.
Mechanical ventilation was initiated with a tidal volume of 8–10 mL/kg and an inspired oxygen fraction of 0.5 at a 3 L fresh gas flow. Anesthesia was maintained using 0.7–1.3 minimal alveolar concentration (MAC) of inhalational agent and 1–3 ng/mL remifentanil of TCI mode. Anesthetic depth was controlled using a bispectral index (BIS) value targeting 40–55 and a heart rate (HR) and mean arterial pressure (MAP) maintained within 20% of baseline. Approximately 15 minutes prior to the end of surgery, inhalational agent was reduced to a BIS value of 60, and the remifentanil Ce was set at the predetermined Ce. Then, 30 mg of IV ketorolac and 0.3 mg of ramosetron were administered for postoperative pain control and antiemetics. At the end of surgery, inhalational agent was stopped, and the fresh gas flow was increased to 10 L/min. Sugammadex of 3 mg/kg was administered to reverse a residual neuromuscular block. Mechanical ventilation was then switched to manual ventilation while supporting the patient’s spontaneous breathing. After the patients opened the eyes to verbal command without other stimulation and adequate self-ventilation was confirmed, extubation was done. Immediately after extubation, remifentanil infusion was stopped and 100% oxygen was supplied via facial mask. After closed observation for 3 minutes, patients were transferred to the postanesthesia care unit (PACU).
Study protocol and outcome measurement
According to randomization using R 3.4.0 (Vienna, Austria; http://www.R-project.org/), participants were randomly assigned to one of the following two groups: sevoflurane group or desflurane group. By Dixon’s up-and-down method, the patients were sequentially enrolled until they reached six success-failure pairs. If one group reached six success-failure pairs, then all subsequent patients were enrolled in the other group. Except in-room outcome assessor, preoperative and postoperative outcome assessors and patients were blinded to the type of intervention.
Preoperative data including age, weight, smoking history, and past medical history were collected. During anesthetic induction, intubation attempts and numbers of endotracheal tube repositioning were recorded. The data including HR, MAP, and peripheral saturation via pulse oximetry were recorded at five time points: baseline (before induction), the end of surgery, immediate before and after extubation, and 3 minutes after extubation.
Cough was defined as a sudden contraction of abdominal muscle. Cough during emergence was recorded from the end of surgery until 3 minutes after extubation. To determine the optimal remifentanil Ce, Dixon’s sequential allocation design was used. The first patient in each group was started with 2 ng/mL of remifentanil Ce. The predetermined Ce of the next patient was set by the cough response during emergence of the previous patient. If the patient did not cough during emergence, we defined it as smooth emergence. Then, the predetermined Ce of the next patient was set 0.5 ng/mL lower than the previous patient. If the patient coughed more than once during emergence, we defined it as failed smooth emergence, and the predetermined Ce of the next patient was set 0.5 ng/mL higher than the previous patient.
Time to extubation was defined as the duration from the end of surgery and stop of inhalational agent to extubation. The MAC of end-tidal inhalational agent was recorded when the patients opened their eyes on verbal command. Respiratory complications including hypoventilation (respiratory rate <8 breaths/minute), laryngospasm, and desaturation (saturation <95%) for 3 minutes after extubation were recorded. Sedation score using the Ramsay Sedation Scale (six levels; 1=Anxious and agitated or restless or both, 6=No response to a light glabellar tap or loud auditory stimulus)24 and nausea, vomiting, and pain score using numeric rating scale (NRS) (0=none, 10=the worst) were assessed at 30 minutes after PACU arrival. Fentanyl of 0.5 mcg/kg was administered when an NRS was 5 or greater.
Statistical analysis
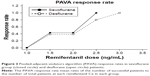
The primary outcomes were the effective concentration of remifentanil to prevent emergence cough in 50% of patients (EC50) and in 95% of patients (EC95). The EC50 by the Dixon’s up-and-down method needs at least six pairs of success-failure, and 20 patients were calculated as mean by midpoints of remifentanil Ce of six success-failure pairs.25 The EC50 was compared between the two groups using independent t-test. The EC50 and EC95 were also calculated by isotonic regression method based on a pooled-adjacent-violators algorithm (PAVA) and 83% and 95% CIs were estimated through a bootstrapping approach.26 If the EC50 and EC95 did not overlap at the 83% CIs and 95% CIs, the values were regarded as showing statistical differences.25,27
The secondary outcomes were time to extubation; respiratory complications during emergence including bradypnea, laryngospasm, and desaturation; sedation score; NRS; and the number of patients receiving fentanyl at the PACU. Of the secondary outcomes, categorical variables including respiratory complications during emergence; sedation score; and the number of patients receiving fentanyl at the PACU were presented as number and frequency. They were compared using chi-squared test or Fisher’s exact test. Continuous variables were tested for normality using the Kolmogorov–Smirnov test. Continuous variables showing normality such as age, height, weight, and BMI were analyzed using Student’s t-test and expressed as mean ± SD. Continuous variables not showing normality such as time to extubation, operation time, anesthetic time, sevoflurane volume percentile at eye opening, and NRS at the PACU were analyzed using the Mann–Whitney test and expressed as median (IQR). The repeated measures variables over time including HR and MAP were analyzed using a linear mixed model. Time and group were entered as interaction terms and the crossover effect was analyzed. A P-value of <0.05 was considered statistically significant. The SPSS package (version 23.0, IBM Corporation, Armonk, NY, USA) including R (version 3.2.5, The R foundation for Statistical Computing; https://www.r-project.org) was used for statistical analyses.
Results
By Dixon’s up-and-down method, the patients were randomly, sequentially allocated and enrolled until they reached six success-failure pairs. A total of 43 patients were assessed. One patient was missing data in PACU but was not withdrawn because we could assess preoperative and intraoperative data from the patient. Finally, 22 and 21 patients were enrolled in the sevoflurane and the desflurane groups without withdrawal, respectively. The CONSORT flow chart is shown in Figure 1. Demographics of patients and operation details were not significantly different between the two groups (Table 1).
  | Figure 1 The CONSORT flow diagram. |
  | Table 1 Patients’ characteristics and intraoperative details |
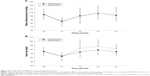
The success and failure of smooth emergence are presented in Figure 2. Isotonic regression curve based on PAVA response rate is shown in Figure 3. The EC50 by Dixon’s method and the EC50 and EC95 by isotonic regression are described in Table 2. The EC50 of remifentanil to prevent emergence cough by Dixon’s method was analyzed as mean from midpoints of pairs from failure to success and the two groups were comparable (2.08±0.47 ng/mL in the sevoflurane group and 2.25±0.40 ng/mL in the desflurane group, P=0.385). Using isotonic regression based on the PAVA response rate, the EC50 (83% CIs) and EC95 (95% CIs) values of remifentanil to prevent emergence cough were 2.06 (1.45–2.23) ng/mL and 2.46 (2.35–2.48) in the sevoflurane group and 2.14 (1.45–2.56) ng/mL and 2.88 (2.47–2.98) in the desflurane group, respectively. They were also comparable between two groups because the 83% and 95% CIs were overlapped. The MAP and the HR at each time point are presented in Figure 4. The MAP did not show any significant difference according to time and group (P=0.649). However, the HR was significantly higher during emergence period in the desflurane group than in the sevoflurane group (P=0.019).
The emergence and recovery outcomes are presented in Table 3. The time to extubation and MAC when eyes are open were comparable between the two groups. Among respiratory complications, five patients in the sevoflurane group and two patients in the desflurane group showed bradypnea within 3 minutes after extubation. Those in the sevoflurane group consisted of one patient each at 1.0 ng/mL and 2.5 ng/mL of remifentanil Ce, two at 2.0 ng/mL, and one at 2.5 ng/mL. Those in the desflurane group all showed bradypnea at 2.0 ng/mL of remifentanil Ce. However, all seven patients who showed bradypnea responded to encouragement of breathing and no-one showed laryngospasm or desaturation. At the PACU, respiratory complications did not occur, and sedation status was observed within the range of awake levels (sedation scores 1, 2, and 3).
Discussion
In this study, we investigated the Ce of remifentanil for preventing cough during emergence from general anesthesia in elderly female patients, according to inhalational agents (sevoflurane or desflurane). We found that EC50 and EC95 for preventing cough during emergence by the Dixon’s method or isotonic regression method did not show significant differences between sevoflurane and desflurane anesthesia in elderly female patients.
Cough reflex and the effect of opioid were known to differ according to sex.15,16,28 Several studies demonstrated that the remifentanil Ce preventing emergence cough showed significant differences according to sex.19–21 Along with sex, aging also was known to be related to cough reflex15,16 and the effect of opioid.29,30 Recently, Yoo et al reported no difference in the remifentanil Ce between adult and elderly patients during emergence from sevoflurane anesthesia.12 However, the influence of aging on remifentanil Ce could not be confirmed because Yoo et al included both male and female patients. The elderly patients are more vulnerable to adverse effects of opioid than young adult patients.31 Finally, emergence cough is especially more dangerous in elderly patients due to multiple comorbidity. Therefore, we included only elderly female patients as subjects in this study, considering the influences of age and sex on evaluating remifentanil Ce to prevent emergence cough.
It is widely believed that desflurane provokes upper airway irritation including coughing and laryngospasm.32 A meta-analysis revealed that desflurane caused a higher incidence of emergence cough than sevoflurane.33 In this study, the EC50 of remifentanil by Dixon’s method and the EC50 and EC95 by isotonic regression method to prevent emergence cough were comparable between sevoflurane group and desflurane group among elderly female patients. These results are consistent with those of Lee et al’s study that evaluated the remifentanil Ce to prevent emergence cough according to anesthetic agents in young and middle aged (20–65 years) female patients.22 Therefore, it may be suggested that the remifentanil Ce preventing emergence cough is similar regardless of the type of inhalational agents in female patients.
With regard to our comparable remifentanil Ce between sevoflurane and desflurane, there are some possible explanations. First, because endotracheal tube is regarded as a relatively more potent airway irritant compared with inhalational agents, the degree of pungency between sevoflurane and desflurane would have been negligible. Actually, most of the studies, which reported significant difference of emergence cough between two inhalational agents, were performed on patients using facial mask or laryngeal mask airway and not on endotracheal intubation.17,34,35 However, the evaluation of the remifentanil Ce between sevoflurane and desflurane is of great clinical importance because the intubated patients generally have greater medical complexity compared with those managed with laryngeal mask airway and thus are exposed to a greater risk of adverse events regarding extubation. Second, the simultaneous administration of opioid might decrease airway response regardless of the type of inhalational agents. The aforementioned studies, which reported significant differences in emergence cough according to inhalational agents, did not use opioid with inhalational agents around the end of surgery and emergence.17,34,35 Whereas other studies, which did not show significant differences between two inhalational agents, used inhalational agents with opioids such as fentanyl or remifentanil.14,22,36 Therefore, the remifentanil infusion during emergence would decrease the distinction of influences according to inhalational agents. Third, in this study, sugammadex was administered for reversal of muscle relaxant in all patients. Cough is one of the commonly reported adverse events with sugammadex.37 It should be distinguished from previous studies using neostigmine or pyridostigmine to reverse muscle relaxation.
Meanwhile, we had performed similar designed study to evaluate sex-related differences in remifentanil Ce for preventing emergence cough in elderly patients.19 Comparing the EC50s in elderly female patients between this study and previous study, the EC50s seem to be quite different despite similar study circumstances (2.14 vs 1.67 ng/mL). However, the comparison of absolute values may be inappropriate because of the differences between the practitioners or the differences between pairs chosen for EC50 (eg, success-failure pairs or failure-success pairs).
Although desflurane was known to have a more rapid awakening and a faster recovery of airway reflex,32 time to extubation and MAC of inhalational agents at eye opening did not show significant difference between two groups in this study. On the contrary, although a balanced anesthesia with desflurane and remifentanil had been shown to conceal a desflurane-induced increase in HR,38 this study showed significant increases in HR in desflurane group compared with sevoflurane group during emergence period (Figure 4). However, this study targeted the remifentanil Ce by Dixon’s method as primary outcomes; the results of secondary outcomes were not specifically powered. To evaluate secondary outcomes, a large volume study is needed that targeted these values.
There were several limitations in this study. First, this study was not double-blinded design. Because the outcome assessors in the operating room were not blinded to predetermined remifentanil Ce, it is possible to affect in-room outcomes. Second, the EC50 of remifentanil by isotonic regression method was calculated from 22 patients’ and 21 patients’ groups by Dixon’s up-and-down allocation method. Because CIs by isotonic regression are more precise at a large sample size, the difference at the EC50 of remifentanil by isotonic regression method may not be reliable.25 Third, because the elderly patients have a large individual variation of biologic capacity, the concealed comorbidities may affect the results. Fourth, although the sugammadex was administered in two groups equally, it was difficult to completely exclude the effect of sugammadex on cough.
Conclusion
Despite the airway irritant property of desflurane, there was no difference in the remifentanil Ce to prevent emergence cough between sevoflurane and desflurane anesthesia. Therefore, the clinicians may not need to adjust the remifentanil Ce to prevent emergence cough according to inhalational agents in elderly female patients.
Disclosure
The authors report no conflicts of interest in this work.
References
Kim ES, Bishop MJ. Cough during emergence from isoflurane anesthesia. Anesth Analg. 1998;87(5):1170–1174. | ||
Irwin RS. Complications of cough: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(1 Suppl):54s–58s. | ||
Diachun CA, Tunink BP, Brock-Utne JG. Suppression of cough during emergence from general anesthesia: laryngotracheal lidocaine through a modified endotracheal tube. J Clin Anesth. 2001;13(6):447–451. | ||
Navarro LH, Lima RM, Aguiar AS, et al. The effect of intracuff alkalinized 2% lidocaine on emergence coughing, sore throat, and hoarseness in smokers. Rev Assoc Med Bras. 2012;58(2):248–253. | ||
Ozturk T, Acikel A, Yilmaz O, Topçu I, Çevikkalp E, Yuksel H. Effects of low-dose propofol vs ketamine on emergence cough in children undergoing flexible bronchoscopy with sevoflurane-remifentanil anesthesia: a randomized, double-blind, placebo-controlled trial. J Clin Anesth. 2016;35:90–95. | ||
Safavi M, Honarmand A, Khazaei M. The effects of propofol, ketamine and combination of them in prevention of coughing and laryngospasm in patients awakening from general anesthesia: a randomized, placebo-controlled, double blind clinical trial. Adv Biomed Res. 2016;5:64. | ||
Beers R, Camporesi E. Remifentanil update: clinical science and utility. CNS Drugs. 2004;18(15):1085–1104. | ||
Mandel JE. Considerations for the use of short-acting opioids in general anesthesia. J Clin Anesth. 2014;26(1 Suppl):S1–S7. | ||
Servin FS, Billard V. Remifentanil and other opioids. Handb Exp Pharmacol. 2008;182(182):283–311. | ||
Jun NH, Lee JW, Song JW, Koh JC, Park WS, Shim YH. Optimal effect-site concentration of remifentanil for preventing cough during emergence from sevoflurane-remifentanil anaesthesia. Anaesthesia. 2010;65(9):930–935. | ||
Lee B, Lee JR, Na S. Targeting smooth emergence: the effect site concentration of remifentanil for preventing cough during emergence during propofol-remifentanil anaesthesia for thyroid surgery. Br J Anaesth. 2009;102(6):775–778. | ||
Yoo JY, Kim JY, Kwak HJ, et al. Effect-site concentration of remifentanil for preventing cough during emergence in elderly patients undergoing nasal surgery: a comparison with adult patients. Clin Interv Aging. 2016;11:1247–1252. | ||
Kim H, Choi SH, Choi YS, Lee JH, Kim NO, Lee JR. Comparison of the antitussive effect of remifentanil during recovery from propofol and sevoflurane anaesthesia. Anaesthesia. 2012;67(7):765–770. | ||
Cho HB, Kim JY, Kim DH, Kim DW, Chae YJ. Comparison of the optimal effect-site concentrations of remifentanil for preventing cough during emergence from desflurane or sevoflurane anaesthesia. J Int Med Res. 2012;40(1):174–183. | ||
Katsumata U, Sekizawa K, Ebihara T, Sasaki H. Aging effects on cough reflex. Chest. 1995;107(1):290–291. | ||
Ebihara S, Ebihara T, Kohzuki M. Effect of aging on cough and swallowing reflexes: implications for preventing aspiration pneumonia. Lung. 2012;190(1):29–33. | ||
White PF, Tang J, Wender RH, et al. Desflurane versus sevoflurane for maintenance of outpatient anesthesia: the effect on early versus late recovery and perioperative coughing. Anesth Analg. 2009;109(2):387–393. | ||
Lema FE, Tafur LA, Giraldo C, Delgado MA. Incidence of cough after desflurane and sevoflurane administration through a laryngeal mask: a controlled clinical trial. Rev Esp Anestesiol Reanim. 2010;57(3):141–146. | ||
Lee SY, Jeong YY, Lee BH, Kim JE. Sex-related differences in effect-site concentration of remifentanil for preventing anesthetic emergence cough in elderly patients. Clin Interv Aging. 2018;13:81–89. | ||
Soh S, Park WK, Kang SW, Lee BR, Lee JR. Sex differences in remifentanil requirements for preventing cough during anesthetic emergence. Yonsei Med J. 2014;55(3):807–814. | ||
Cui XL, Ma MJ, Wang L, et al. Influence of sex on remifentanil’s cough-prevention effect during anesthetic emergence. Zhongguo Yi Xue Ke Xue Yuan Xue Bao. 2015;37(3):335–338. | ||
Lee JH, Choi SH, Choi YS, Lee B, Yang SJ, Lee JR. Does the type of anesthetic agent affect remifentanil effect-site concentration for preventing endotracheal tube-induced cough during anesthetic emergence? Comparison of propofol, sevoflurane, and desflurane. J Clin Anesth. 2014;26(6):466–474. | ||
Minto CF, Schnider TW, Shafer SL. Pharmacokinetics and pharmacodynamics of remifentanil. II. Model application. Anesthesiology. 1997;86(1):24–33. | ||
Ramsay MA, Savege TM, Simpson BR, Goodwin R. Controlled sedation with alphaxalone-alphadolone. Br Med J. 1974;2(5920):656–659. | ||
Pace NL, Stylianou MP. Advances in and limitations of up-and-down methodology: a précis of clinical use, study design, and dose estimation in anesthesia research. Anesthesiology. 2007;107(1):144–152. | ||
Dilleen M, Heimann G, Hirsch I. Non-parametric estimators of a monotonic dose-response curve and bootstrap confidence intervals. Stat Med. 2003;22(6):869–882. | ||
Payton ME, Greenstone MH, Schenker N. Overlapping confidence intervals or standard error intervals: what do they mean in terms of statistical significance? J Insect Sci. 2003;3:34. | ||
Fillingim RB, Gear RW. Sex differences in opioid analgesia: clinical and experimental findings. Eur J Pain. 2004;8(5):413–425. | ||
Wilder-Smith OH. Opioid use in the elderly. Eur J Pain. 2005;9(2):137–140. | ||
Minto CF, Schnider TW, Egan TD, et al. Influence of age and gender on the pharmacokinetics and pharmacodynamics of remifentanil. I. Model development. Anesthesiology. 1997;86(1):10–23. | ||
Martin CM, Forrester CS. Anticipating and managing opioid side effects in the elderly. Consult Pharm. 2013;28(3):150–159. | ||
Jakobsson J. Desflurane: a clinical update of a third-generation inhaled anaesthetic. Acta Anaesthesiol Scand. 2012;56(4):420–432. | ||
de Oliveira GS, Girao W, Fitzgerald PC, Mccarthy RJ. The effect of sevoflurane versus desflurane on the incidence of upper respiratory morbidity in patients undergoing general anesthesia with a Laryngeal Mask Airway: a meta-analysis of randomized controlled trials. J Clin Anesth. 2013;25(6):452–458. | ||
Saros GB, Doolke A, Anderson RE, Jakobsson JG. Desflurane vs. sevoflurane as the main inhaled anaesthetic for spontaneous breathing via a laryngeal mask for varicose vein day surgery: a prospective randomized study. Acta Anaesthesiol Scand. 2006;50(5):549–552. | ||
Terriet MF, Desouza GJ, Jacobs JS, et al. Which is most pungent: isoflurane, sevoflurane or desflurane? Br J Anaesth. 2000;85(2):305–307. | ||
de Oliveira GS, Fitzgerald PC, Ahmad S, Marcus RJ, Mccarthy RJ. Desflurane/fentanyl compared with sevoflurane/fentanyl on awakening and quality of recovery in outpatient surgery using a laryngeal mask airway: a randomized, double-blinded controlled trial. J Clin Anesth. 2013;25(8):651–658. | ||
Mirakhur RK. Sugammadex in clinical practice. Anaesthesia. 2009;64 (Suppl 1):45–54. | ||
Fanelli G, Berti M, Casati A. Fast-track anaesthesia for laparoscopic cholecystectomy: a prospective, randomized, multicentre, blind comparison of desflurane-remifentanil or sevoflurane-remifentanil. Eur J Anaesthesiol. 2006;23(10):861–868. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.