Back to Journals » Clinical Ophthalmology » Volume 18
Comparison of Refractive Prediction Error by Axial Length in Flanged Intrascleral Intraocular Lens Fixation
Authors Kabata Y , Oki T , Nakano T
Received 15 December 2023
Accepted for publication 14 March 2024
Published 21 March 2024 Volume 2024:18 Pages 895—900
DOI https://doi.org/10.2147/OPTH.S455178
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Yoshiaki Kabata,1 Tetsutaro Oki,1 Tadashi Nakano2
1Department of Ophthalmology, Jikei University School of Medicine, Daisan Hospital, Tokyo, Japan; 2Department of Ophthalmology, The Jikei University School of Medicine, Tokyo, Japan
Correspondence: Yoshiaki Kabata, Department of Ophthalmology, Jikei University School of Medicine, Daisan Hospital, 4-11-1 Izumihontyou, Komae-si, Tokyo, 125-8506, Japan, Tel +81334801151, Fax +81334805700, Email [email protected]
Purpose: To evaluate the refractive prediction error in flanged intrascleral intraocular lens (IOL) fixation using the SRK/T formula and compare the axial length using a single IOL.
Methods: Seventy-six eyes from 70 patients (45 males and 25 females) were included in this study. The mean age at the time of surgery was 73.4 ± 12.3 years. The patients underwent flanged IOL fixation using a PN6A (Kowa). All surgeries were performed by two surgeons (Y. K. and T. O.) between Jan 2020 and Dec 2022 at Jikei University Daisan Hospital. IOL power was calculated using the SRK/T formula with IOL Master 700 (Carl Zeiss) as the bag power. The recommended value of 119.0 was used for the A-constant. The actual refractive spherical equivalent was calculated and compared with preoperative predictions. Refractive prediction errors were defined as the deviation of the actual postoperative spherical equivalent refraction in diopters from the predicted preoperative spherical equivalent refraction. The patients were divided into three groups according to axial length: < 22.0 mm (short eyes), 22.0– 24.5 mm (medium eyes), and > 24.5 mm (long eyes), and the refractive prediction errors and mean absolute errors were compared.
Results: The mean refractive prediction error was − 0.20 ± 0.52D. The mean absolute error was 0.44 ± 0.33D. The mean refractive prediction errors were not significantly different between the 22.0– 24.5 mm (medium eyes) and > 24.5 mm (long eyes) groups. (P=0.06) The mean absolute errors were not significantly different between the two groups (P=0.10).
Conclusion: The SRK/T formula worked well regardless of whether the eyes were medium or long according to the axial length in the flanged intrascleral IOL fixation.
Keywords: flanged intrascleral IOL fixation, refractive prediction error, SRK/T formula, axial length
Introduction
Secondary intraocular lens implantation surgery is a procedure used to address various issues that may arise after primary cataract surgery or in specific clinical scenarios. In these cases, the IOL must be fixed in other positions, such as the anterior chamber, iris, sulcus, or sclera.1 Commonly performed surgical procedures are iris fixation and scleral-sutured, but with complications of corneal endothelial cell loss and suture knot erosion.2
The flanged intrascleral intraocular lens (IOL) fixation method reported by Yamane et al demonstrated excellent visual outcomes, predictable postoperative refractive errors, a low rate of endothelial cell loss, and relatively few complications.3 The Yamane technique has gained popularity, and several modifications have been described.3–5 This technique requires haptics of the IOL to form a flange with heat. Furthermore, haptics must be durable and flexible for grasping with forceps.3,4 Polyvinylidene is a suitable material for haptics; thus, X-70 (Santen, Osaka, Japan) and PN6A (Kowa, Tokyo, Japan) are commonly used in Japan.4 We used PN6A for intrascleral fixation because of its optical flexibility and easy operability within the anterior chamber.
Flanged intrascleral IOL fixation has a low complication rate, and the surgeon’s interest has shifted to accurate predictive refractive values for patient satisfaction. In cataract surgery, refractive prediction errors in intrascleral fixation reduce visual acuity in the naked eye and are a major cause of patient dissatisfaction.6,7 We consider that preoperative biometric measurements and the choice of IOL power calculation formula are important. According to a clinical survey conducted by the Japanese Society of Cataract and Refractive Surgery in 2018, the SRK/T formula is still the most commonly used formula for IOL power calculation in Japan. In intrascleral IOL fixation, the preoperative anterior chamber depth is not accurately measured; therefore, the SRK/T is the main formula used for IOL calculation. Axial length is a major factor affecting refractive prediction error,8 and the selection of IOL calculation based on axial length is not commonly known in intrascleral IOL fixation. There are many reports of refractive prediction error in intrascleral fixation with other IOLs have been seen,4,5,9–12 but few reports have used PN6A,3,4 and we consider it very important to understand the trend of refractive prediction error at each institution.
This study aimed to evaluate the refractive prediction error in flanged intrascleral IOL fixation using the SRK/T formula and to compare the axial length using PN6A.
Materials and Methods
This study was approved by the ethics committee of the Jikei University School of Medicine: 35–348 (11980). The study protocol was conducted in accordance with the tenets of the Declaration of Helsinki, and informed consent was obtained from all the patients.
The patients underwent flanged IOL fixation for aphakia, a subluxated lens, or a dislocated IOL. PN6A was used in all IOL fixation procedures. All surgeries were performed by two surgeons (Y. K. and T. O.) between January 2020 and December 2022 at the Jikei University Daisan Hospital. All patients were followed up for at least six months after surgery.
Exclusion criteria were previous intraocular surgery, trauma, silicone oil tamponade, scleral buckle, corneal ectasia, corneal degeneration, corneal dystrophy, post-corneal surgery status, open-globe trauma, advanced macular disease, and dropout.
IOL power was calculated using the SRK/T formula with the IOL Master 700 (Carl Zeiss Meditec, Jena, Germany). A recommended value of 119.0 was used for the A-constant. The actual refractive spherical equivalent was compared with the preoperative prediction. Refractive prediction errors were defined as the deviation of the actual postoperative spherical equivalent refraction in diopters (D) from the predicted preoperative spherical equivalent. The postoperative spherical equivalent was measured 2–3 months after surgery.
Surgical Technique: After induction of post-glottic anesthesia with 0.75% ropivacaine, a 25-gauge pars plana vitrectomy was performed. For patients with a subluxated lens, the lens was removed using a 25-gauge cutter, and phacoemulsification and aspiration were performed. In patients with IOL dislocation, the IOL was removed through a 4.0–6.0 mm L-shaped corneoscleral incision. The capsular bags were removed using a cutter or forceps.
Angled sclerotomy was performed through the conjunctiva using a 30-gauge thin-walled needle (TSK ultra-thin-wall needle; Tochigi Seiko, Tochigi, Japan) 2 mm from the limbus. The leading haptic was threaded into the lumen of the needle using forceps. A second sclerotomy was performed using a 30-gauge thin-walled needle at 180° from the first sclerotomy. The trailing haptic was inserted into the lumen of the second needle, and the first needle was placed on the eyelid. Both haptics were externalized to the conjunctiva by using a double needle. The ends of the haptics were cauterized using an ophthalmic cautery device (Accu-Temp Cautery; Beaver Visitec, Waltham, MA, USA) to create a 0.3-mm diameter flange. The flanges of the haptics were pushed back and fixed in scleral tunnels. To avoid IOL iris capture, peripheral iridotomy was performed using a vitrectomy cutter after miosis.3
The patients were divided into three groups according to axial length: <22.0 mm (short eyes), 22.0–24.5 mm (medium eyes), and >24.5 mm (long eyes), and refractive prediction errors and mean absolute prediction errors were compared. The Mann–Whitney U-test, a nonparametric statistical test, used to compare refractive prediction errors and mean absolute errors. Statistical significance was set at P < 0.05. Statistical analysis was performed using JMP®11 (SAS Institute Inc., Cary, NC).
Results
This study analyzed 76 eyes of 70 patients (45 males and 25 females). The mean age at the time of surgery was 73 ± 12 years, with an average follow-up period of 237 days (range 190–920 days). Postoperative complications included high intraocular pressure (16 eyes), vitreous hemorrhage (four eyes), IOL iris capture (two eyes), choroidal detachment (one eye), iris exposure from the wound (one eye), and macular edema (three eyes). Scatter plots of the refractive prediction errors for all patients are shown in Figure 1. The mean refractive prediction error was −0.20 ± 0.52D.
 |
Figure 1 Scatter plots of all patients’ refractive prediction errors. |
The patients were divided into three groups according to axial length: <22.0 mm (short eyes), 22.0–24.5 mm (medium eyes), and >24.5 mm (long eyes), and the characteristics of each group are shown in Table 1. The short eye group was excluded from the statistical analysis because there were two cases.
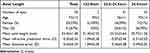 |
Table 1 Characteristics of Patients Divided into Three Groups by Axial Length |
Box-and-whisker diagrams of the refractive prediction errors are shown in Figure 2. The mean refractive prediction errors were not significantly different between the 22.0–24.5 mm (medium eyes) and >24.5 mm (long eyes) groups. (P=0.06) Box-and-whisker diagrams of mean absolute errors are shown in Figure 3. The mean absolute errors were not significantly different between the two groups. (P=0.10)
Discussion
In this study, the mean refractive prediction error in all patients was −0.20 ± 0.52D, the mean prediction absolute error was 0.44 ± 0.33D. Compared with previous reports (−0.17 ± 0.88D3, 0.93 ± 0.75D4) of the same IOL: PN6A, the prediction errors were no significant difference. There were also no significant differences in postoperative complications.3,4 All groups showed a tendency toward myopia; however, the mean refractive prediction errors were not significantly different between the medium and long eye groups, so there was no need to change the IOL calculation method in the long eyes.
The flanged intrascleral IOL fixation technique requires haptics of the IOL to form a flange with heat.3 Polyvinylidene is a suitable material for haptics; thus, X-70 and PN6A are commonly used in Japan. In this study, we used PN6A for intrascleral fixation because of the flexibility of its optical part and its easy maneuverability within the anterior chamber. Iris capture was observed in 2 (0.03%). Although PN6A is a 6-mm optic IOL, the incidence of iris capture was lower than that previously reported,3,4,12,13 as all patients underwent iridectomy. A peripheral iridotomy may reduce the pressure difference between the anterior and posterior chambers; thus, iris capture is less likely to occur in 6-mm optic IOL.4
Third-generation formulas such as Holladay 1, Hoffer Q, and SRK/T have been used to predict the estimated lens power using the axial length, corneal curvature, and A-constant.14 Fourth-generation formulas, such as Haigis, also consider the preoperative anterior chamber depth.6,7 These modern formulas for predicting IOL power have much greater accuracy; however, the anterior chamber depth cannot be measured in cases of intrascleral fixation because of lens displacement in patients presenting for preoperative assessment.
Inaccuracies in IOL calculations have various reasons, including errors in measuring the axial length, IOL A-constant used, and assumed effective lens position location.5,9,11 Errors in axial length measurement are critical because they can change the calculated lens power three times.11 Greater accuracy in axial length measurement has been shown when utilizing optical biometry versus ultrasonography,15,16 and we used the IOL Master 700 for all patients.
IOL formulas assume that a lens is placed in a capsular bag. Standardizing the placement of the fixation at a distance posterior to the limbus helps to minimize some of the variations. The final IOL position may be affected if the capsule has not been completely removed. The peripheral capsule can harbour retained lens material, which may affect the anterior position of the IOL.11 It was suggested that intrascleral fixation with complete removal of the lens capsule, unaffected by the contraction of the lens capsule, may result in fewer refractive prediction errors after a long time. The strength and flexibility of haptics can also affect lens position or damage haptics. In this regard, IOLs with polyvinylidene haptics are considered best suited for flanged intrascleral IOL fixation.4 Anatomical variations with posttraumatic or highly myopic eyes may also contribute to errors in effective lens position; however, the details of these factors and how they contribute to the lens position in flanged fixation remain unknown.11 As all lens capsules are removed in this study, it is assumed that there is no effect of capsular bag’s shrinkage.
This study evaluated the accuracy of the SRK/T formula for flanged intrascleral IOL fixation with PN6A fixed 2 mm posteriorly to the limbus. The heterogeneity in the scleral fixation methods has resulted in the absence of data on refractive outcomes for PN6A.3,4 Previously, SRK/T demonstrated good results for long and short axial lengths.6,11,14,15,17 Our results also showed no significant prediction errors between medium and long eyes. The SRK/T formula worked well regardless of whether the eyes were medium or long according to the axial length in the flanged intrascleral IOL fixation. A constant can also be a source of error. In high myopia, manufactured A-constants are more accurate than recommended A-constants.11 In this study, the mean refractive prediction error tended to be less than predicted; thus, the A-constant of PN6A needs to be adjusted at The Jikei University Daisan Hospital.
The limitation of our study is that a statistical study of small eyes could not be performed. Therefore, cases with small eyes need to be considered; thus, more cases and longer follow-up periods are required. Furthermore, IOL tilt must be considered, and cases with a large IOL tilt should be excluded.3 This study could not consider the tilt because of the lack of data.
Conclusion
This study highlighted the accuracy of the SRK/T formula for flanged intrascleral IOL fixation using PN6A. The SRK/T formula worked well regardless of whether the eyes were medium or long according to the axial length in the flanged intrascleral IOL fixation.
Disclosure
Tadashi Nakano: grants – Crewt Medical Systems, Kyowa Medical, Kuribara Medical Instruments, Tomey, MSD, Pfizer, Alcon Japan, NIDEK, AMO Japan, Bayer, IOL Medical, All Nippon Airway, Japan Airlines; personal fees – Nitto Medic, Nikon; grants and personal fees – Kowa, Otsuka Pharmaceutical, Senju Pharmaceutical, Santen Pharmaceutical, Carl Zeiss, outside the submitted work. The other authors declare no conflicts of interest.
References
1. Vounotrypidis E, Schuster I, Mackert MJ, Kook D, Priglinger S, Wolf A. Secondary intraocular lens implantation: a large retrospective analysis. Graefes Arch Clin Exp Ophthalmol. 2019;257(1):125–134. doi:10.1007/s00417-018-4178-3
2. Hoffman RS, Fine HI, Packer M, Rozenberg I. Scleral fixation using suture retrieval through a scleral tunnel. J Cataract Refract Surg. 2006;32(8):1259. doi:10.1016/j.jcrs.2006.02.065
3. Yamane S, Sato S, Maruyama-Inoue M, Kadonosono K. Flanged intrascleral intraocular lens fixation with double-needle technique. Ophthalmology. 2017;124(8):1136–1142. doi:10.1016/j.ophtha.2017.03.036
4. Miura Y, Harada Y, Kiuchi Y. Comparison of different IOL types in the flanged IOL fixation technique. J Ophthalmol. 2020;2020:8534028. doi:10.1155/2020/8534028
5. Randerson EL, Bogaard JD, Koenig LR, Hwang ES, Warren CC, Koenig SB. Clinical outcomes and lens constant optimization of the Zeiss CT Lucia 602 lens using a modified Yamane technique. Clin Ophthalmol. 2020;14:3903–3912.
6. Kane JX, Chang DF. Intraocular lens power formulas, biometry, and intraoperative aberrometry: a review. Ophthalmology. 2021;128(11):e94–e114. doi:10.1016/j.ophtha.2020.08.010
7. Stopyra W, Langenbucher A, Grzybowski A. Intraocular lens power calculation formulas—a systematic review. Ophthalmol Ther. 2023;12(6):2881–2902. doi:10.1007/s40123-023-00799-6
8. Doshi D, Limdi P, Parekh N, Gohil N. A comparative study to assess the predictability of different IOL power calculation formulas in eyes of short and long axial length. J Clin Diagn Res. 2017;11(1):NC01–NC04. doi:10.7860/JCDR/2017/22095.9136
9. McMillin J, Wang L, Wang MY, et al. Accuracy of intraocular lens calculation formulas for flanged intrascleral intraocular lens fixation with double-needle technique. J Cataract Refract Surg. 2021;47(7):855–858. doi:10.1097/j.jcrs.0000000000000540
10. Malach DS, Guest JM, Adam C, et al. Intraocular lens formula comparison of flanged intrascleral intraocular lens fixation with double needle technique. Clin Ophthalmol. 2023;17:837–842. doi:10.2147/OPTH.S389325
11. Ohr MP, Wisely CE. Refractive outcomes and accuracy of IOL power calculation with the SRK/T formula for sutured, scleral-fixated Akreos AO60 intraocular lenses. Graefes Arch Clin Exp Ophthalmol. 2020;258(10):2125–2129. doi:10.1007/s00417-020-04721-9
12. Rocke JR, McGuinness MB, Atkins WK, et al. Refractive outcomes of the Yamane flanged intrascleral haptic fixation technique. Ophthalmology. 2020;127(10):1429–1431. doi:10.1016/j.ophtha.2020.03.032
13. Nowomiejska K, Haszcz D, Onyszkiewicz M, et al. Double-needle Yamane technique using flanged haptics in ocular trauma—a retrospective survey of visual outcomes and safety. J Clin Med Res. 2021;10(12):2562.
14. Razmjoo H, Atarzadeh H, Kargar N, Behfarnia M, Nasrollahi K, Kamali A. The comparative study of refractive index variations between haigis, Srk/T and Hoffer-Q formulas used for preoperative biometry calculation in patients with the axial length >25 mm. Adv Biomed Res. 2017;6:78. doi:10.4103/2277-9175.210657
15. Karabela Y, Eliacik M, Kaya F. Performance of the SRK/T formula using A-scan ultrasound biometry after phacoemulsification in eyes with short and long axial lengths. BMC Ophthalmol. 2016;16:96. doi:10.1186/s12886-016-0271-8
16. De Bernardo M, Cione F, Capasso L, Coppola A, Rosa N. A formula to improve the reliability of optical axial length measurement in IOL power calculation. Sci Rep. 2022;12(1):18845. doi:10.1038/s41598-022-23665-0
17. Sanders DR, Retzlaff JA, Kraff MC, Gimbel HV, Raanan MG. Comparison of the SRK/T formula and other theoretical and regression formulas. J Cataract Refract Surg. 1990;16(3):341–346. doi:10.1016/S0886-3350(13)80706-7
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


