Back to Journals » Journal of Pain Research » Volume 10
Comparison of QuadrapolarTM radiofrequency lesions produced by standard versus modified technique: an experimental model
Authors Safakish R
Received 5 January 2017
Accepted for publication 23 March 2017
Published 2 June 2017 Volume 2017:10 Pages 1377—1382
DOI https://doi.org/10.2147/JPR.S129478
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Katherine Hanlon
Video abstract presented by Ramin Safakish
Views: 20492
Ramin Safakish
Allevio Pain Management Clinic, Toronto, ON, Canada
Abstract: Lower back pain (LBP) is a global public health issue and is associated with substantial financial costs and loss of quality of life. Over the years, different literature has provided different statistics regarding the causes of the back pain. The following statistic is the closest estimation regarding our patient population. The sacroiliac (SI) joint pain is responsible for LBP in 18%–30% of individuals with LBP. Quadrapolar™ radiofrequency ablation, which involves ablation of the nerves of the SI joint using heat, is a commonly used treatment for SI joint pain. However, the standard Quadrapolar radiofrequency procedure is not always effective at ablating all the sensory nerves that cause the pain in the SI joint. One of the major limitations of the standard Quadrapolar radiofrequency procedure is that it produces small lesions of ~4 mm in diameter. Smaller lesions increase the likelihood of failure to ablate all nociceptive input. In this study, we compare the standard Quadrapolar radiofrequency ablation technique to a modified Quadrapolar ablation technique that has produced improved patient outcomes in our clinic. The methodology of the two techniques are compared. In addition, we compare results from an experimental model comparing the lesion sizes produced by the two techniques. Taken together, the findings from this study suggest that the modified Quadrapolar technique provides longer lasting relief for the back pain that is caused by SI joint dysfunction. A randomized controlled clinical trial is the next step required to quantify the difference in symptom relief and quality of life produced by the two techniques.
Keywords: lower back pain, radiofrequency ablation, sacroiliac joint, Quadrapolar radiofrequency ablation
Introduction
Lower back pain (LBP) is defined as any back pain from the ribs to proximal thigh.1,2 LBP is a global public health issue and is associated with substantial financial costs and loss of quality of life.3–6 In different age groups, the pathology of different structures are responsible for LBP. In adults, aged <45 years, LBP is the most common cause of activity limitations and LBP, after arthritis, is the second most common cause of activity limitations in individuals aged 45–65 years old.1 One well-known cause of LBP is sacroiliac (SI) joint pain.7 SI joint pain is responsible for LBP in 18%–30% of individuals.7
The SI joint plays an important role in load transfer between the spine and lower extremities. The innervation of the SI joint is not well understood. It has been reported that the joint receives innervation from the L4, L5 (L5DR), and the S1-to-S3 dorsal rami along with contributions from S4.8–10 Others have reported that the SI joint receives innervation from the ventral rami of L4 and L5, the dorsal rami of L5, S1, and S2.11,12 Variability exists between individuals in the path of the sacral lateral branches leaving the posterior foramina. These sacral lateral branches may travel along the surface of the sacrum or run distally into the posterior ligaments.11,12 Findings from immunohistological studies indicate that nociceptors are present throughout the joint capsule and ligaments. Nociceptors are also present throughout the subchondral bone; however, to a lesser extent.13 SI joint pain is often caused by ligament laxity or asymmetric laxity.14,15
Radiofrequency ablation is currently a commonly used treatment for SI joint pain. Radiofrequency ablation involves the ablation of nerves using heat generated from alternating current in the range of 350–500 kHz.16 However, the standard radiofrequency procedures are not always effective at ablating all the sensory nerves. The major limitation of standard radiofrequency ablation is that it produces small lesions (~4 mm in diameter). The smaller the lesion, the higher the likelihood of failure to ablate all nociceptive input. To overcome this limitation, we have developed an alternative technique that we hypothesized would produce larger lesions. In clinic, this technique has been associated with improved patient outcomes including greater reductions in pain (as assessed using the visual analogue scale) and improved quality of life (as assessed using the McGill Quality of Life questionnaire) (unpublished data, Allevio Clinic internal quality control). To investigate whether the modified technique is effective at producing larger lesions, we used an in vitro experimental model using a chicken breast to compare the lesion size produced by the standard and modified technique. Below we describe the standard and modified techniques. We then present findings from experimental model comparing lesion size between the two techniques.
The diagnosis of SI joint caused pain is made by using a diagnostic procedure of SI joint block with local anesthetic guided by fluoroscopy. Following the diagnosis, the patient is given the choice of having the standard or modified Quadrapolar™ radiofrequency technique.
Quadrapolar radiofrequency ablation: standard technique
After usual preparation, sterile preparation and draping the surrounding area, with the guide of fluoroscopy, in anterior–posterior view, the location of L5–S1 facet joint as well as S1– S3 are bilaterally identified.
In anterior–posterior, the skin infiltrates in several different locations, to form a hypothetical continuous line, 1 cm lateral to neuroforamina of S1–S3. The skin is prepared for L5–S1 posterior rami ablation by a bipolar radiofrequency ablation.
Four radiofrequency cannulae are inserted posterioanteriorly, perpendicular to skin fluoroscopy tunnel view, until they reach the structure of the sacrum. The Quadrapolar radiofrequency machine will make a lesion between 4 cannulae. The lesion would make a continuous area of thermal damage in the tissue, 1 cm lateral to neuroforamina. Depending on the size of the patient, a second lesion could be necessary along the first lesion to cover all the lateral aspects of all 3 neuroforamina. By doing this, an interruption of the somatosensory branches of S1–S3 toward the joint is achieved. The width of the lesion along the somatosensory nerve will depend on the size of the radiofrequency cannula (RF) cannula.
Quadrapolar radiofrequency ablation: modified technique
In the modified technique, by changing the orientation of radiofrequency cannulae, we expect to be able to produce a larger interruption in nociceptor messages from the SI joints. Moreover, the location of the lesion in the interosseous ligaments could potentially increase the stability of the SI joints. This large lesion is made of two smaller lesions, overlapping each other. Each lesion is formed using four radiofrequency cannulae. We start from the most inferior–posterior part of the joint and make the first lesion by inserting each cannula about 1 cm superior to the last cannula. The second lesion is made superior to the first one. The orientation of the cannulae are from posteriomedial, starting from midline to anterolateral, ending just medial to the joint line or in interosseous ligaments.
Given that each SI joint has a different degree of anteroposterior rotation, the correct angle of the inferior part of the SI joint is detected by rotating the C-arm away from the side of the joint to produce the most suitable view for cannulae insertion. In this article, due to considerable individual variation in the anatomy of the sacrum and SI joints, the exact angles of the C-arm are seldom mentioned for cannulae insertion. As a general rule, even when the anatomy is atypical, the anteroposterior or the tunnel view of the SI joints is used. The angle of the SI joint is more mediolateral than anteroposterior. To obtain a tunnel view of the joint space, one should rotate the C-arm to the ipsilateral side. In addition, the angle of the joint along the vertical axis varies as gender, race, and anatomical variation play a role in joints development. Cognizance of these facts is of paramount importance to attain a successful outcome.
Considering the above observations, we have come to realize that the mediolateral approach is more logical than the current (posteroanterior) approach described in the standard Quadrapolar technique. By altering the standard technique, the procedure is technically simpler. Moreover, the modified thermal lesion in the interosseous ligaments could potentially shrink the ligaments during the healing process. By doing so, the RF procedure would potentially stabilize the SI joints.
In general, radiofrequency of the SI joints has two different stages. The first stage is the same in standard and modified technique. In both techniques, L5–S1 posterior rami would be ablated by a bipolar radiofrequency ablation.
The second stage, ablation of the SI joint, is different in two techniques. Therefore, we would focus on the second step of the procedure. The first four cannulae are inserted posterior and parallel to the midline of the sacrum. For ease of explanation, the cannulae would be labeled as C-1, C-2, C-3, and C- 4. The following are different steps of performing the modified approach to perform radiofrequency ablation of the SI joints:
- C-1 is inserted in midline, in the same level as the most posterior–inferior part of the SI joints. General direction of each cannulae would be anterolateral. The tip of the C-1 targets the most posterior, inferior part of SI joint. Once the practitioner feels that the tip of the cannula has reached the bony surface of the sacrum, the position of the tip would be confirmed by fluoroscopy. The last mentioned image would be taken to ensure that the tip of the cannula is not intraforaminal or lateral to the joint line. At this point, the hub of the curved cannulae would be rotated to be parallel to the sacrum and the cannulae would be advanced to be located just medial to the joint line. By doing so, the entire length of active tip would be positioned adjacent and parallel to the bony surface of the sacrum.
- The next three cannulae would be inserted 1 cm superior to the previous one and angled to be parallel to the first one.
- The tip of each cannula is inserted 0.5 cm lateral and 1 cm superior to the lower one for the first Quadrapolar lesions.
- In most of the average size adults, the tip of C-4 would be located in nonsynovial portion of the SI joint. Therefore, the cannula could be inserted into the joint space.
- The “second” Quadrapolar lesion would be made as described below.
- C-1, C-2, C-3, and C-4 would be withdrawn to the skin level.
- C-1 would be advanced, aiming to the point that C-4 tip had been (in the first lesion).
- C-2, C-3, and C-4 would be advanced in the same way as described for the first lesion. The main difference is the final position of the tip of each cannulae. Each endpoint would be located as far lateral as possible, within the interosseous ligaments.
- By locating C-1 to the location of C-4 in the first lesion, a continuous lesion would be produced.
- To increase the size of the lesion, we intentionally position the tip of C-2 and C-4, 10 mm lateral to C-1 and C-3. One long lesion, consisting of two sets of Quadrapolar lesions, is created. The procedure is repeated on the contralateral SI joint if necessary, through the same entry points.
Experimental model
Materials and methods
To evaluate the area of the lesion produced using the modified Quadrapolar technique, we used chicken breast (used in many studies to visualize lesions generated by RF lesioning), to compare the length, width, and surface area of lesions produced using the conventional and modified Quadrapolar RF techniques. We hypothesized that the prolonged relief experienced by patients could be due to the larger area of the lesion in modified method, compared to the conventional Quadrapolar technique. In previous studies regarding the efficacy of radiofrequency neurotomy, the lesion size was considered the most contributing factor in the duration of the pain relief.
The chicken breasts were purchased from a local store. The packages were never frozen and stored in a fridge at about ±1°C. Immediately before the experiment, the meat was warmed up using the double dish hot water until the core temperature reached 37°C. During the experiment, a Study Light with a hot lamp, 200 W light bulb, was used to prevent temperature dropping in the specimen. Before each lesion, the temperature was monitored again to make sure it was not <36°C centigrade. If the temperature dropped below 36°C, the double dish hot water was used to increase the temperature of the specimen.
The lesion dimensions and area produced by the conventional Quadrapolar (Diros Technology, Markham, Ontario ON, Canada) and modified Quadrapolar techniques (Diros Technology) were examined using chicken breast in a method previously reported by Cohen et al.17 The temperature of the chicken breast was measured using a temperature probe inserted 3 cm into the chicken breast and maintained at 37±1°C. Experiment #1 demonstrated the lesion size produced using the conventional Quadrapolar technique while experiment #2 showed the lesion size created by the modified Quadrapolar technique. Three trials were conducted for each experiment, and the average lesion size was calculated. For both experiments #1 and #2, the ablation temperature was set at 85°C for 3 minutes, the same setting that we use for traditional RF of the SI joints, including 1-minute ramp up to 85°C. For experiment #1, four cannulae were inserted into the chicken perpendicularly through a foam pad (Figure 1) with the needles 1 cm apart. For experiment #2, the chicken breast was sliced parallel to the surface and needles were placed parallel to the meat, 1 cm apart. In the modified technique, a staggered conformation was used, with adjacent needles being alternated in depth by 10 mm (Figure 2).
  | Figure 1 Sample lesion from experiment #1. Notes: Sample lesion produced by standard Quadrapolar™ radriofrequency lesion in chicken breast. Lesion length (A) and width (B). |
  | Figure 2 Sample lesion from experiment #2. Notes: Sample lesion produced by modified Quadrapolar™ radriofrequency lesion in chicken breast. Lesion length (A) and width (B). |
The length of each lesion was measured end to end using a digital caliper ruler (Precise). The width of the lesion was measured with calipers at the widest point of the lesion. Images of the lesions were taken using a Canon camera mounted on a tripod above the chicken breast and area was calculated using Image J software.
Results
Lesion dimensions
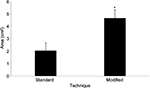
The modified Quadrapolar technique produced lesions that were significantly wider when compared to the conventional Quadrapolar technique (t=−6.097; df=4; p=0.004; Figure 3). There was a trend toward increased lesion length in the modified Quadrapolar technique compared to the conventional Quadrapolar technique (t=−2.605; df=4; p=0.060; Figure 3).
Lesion area
The modified Quadrapolar technique produced a lesion with an area approximately two times the area of the lesion by standard technique (t=3.622; df=4; p=0 .022; Figure 4).
Discussion
Findings from our in vitro investigation revealed that the modified technique produced lesions that were significantly larger in area compared to the lesion produced using the standard Quadrapolar technique. The increase in area produced by the modified Quadrapolar technique was driven by an increase in width of the lesion.
The increased width of the lesion produced by the modified technique could potentially increase the success rate due to the larger interruption of the sensory pathway. We hypothesized that when the lesion is at the same track as the anatomical path of the dorsal rami, the chance for a larger interruption of the nociceptive stimulus through the correlated dorsal rami exists. The sensory nerves of the SI joint run from medial to lateral (starting from the neuroforamina close to midline and travel toward the joints).
In the standard approach, the active tip of the RF cannulae is positioned along the anterior–posterior axis, almost perpendicular to the sensory nerves of the SI joint. Considering that the radius of the effective lesion extends only within 2 mm from the outer wall of the cannula, the overall lesion size would not be very large. The major part of the lesion would be in the soft tissue and ligaments. In the best case scenario, the sensory nerves would be in contact with the tip of the cannula in a cross-sectional fashion. In the modified technique of Quadrapolar radiofrequency ablation of the SI joints, the active tip of the cannula is placed along the mediolateral axis, parallel to the sensory nerves of the SI joint. Therefore, ablation of the sensory nerves occurs along the length of the active tip of the cannula, which is about 10 mm. Therefore, it is logical to assume that in the modified technique, the larger ablation subsequently would cause a greater interruption of sensory input from the joints.
The modified technique has a secondary advantage, which is producing a thermal lesion within the interosseous ligaments. We speculated that the “damaged” tissue would be replaced by scar tissue, and consequently, the ligaments would be contracted. Since it has been reported that SI joint pain is often caused by ligament laxity and asymmetric laxity of joints,14,15 contracture of interosseous ligaments by modified quadrapolar technique potentially could stabilize the joints and thereby, could reduce dysfunction of the SI joints.
Finally, limited number of the skin puncture sites with the modified technique would theoretically shorten the recovery period and time-off-work. As well, the patient may experience minor postprocedural pain due to less soft tissue damage. The reduction of postprocedural pain is just a retrospective observation and was not proven. We suggest a prospective randomized trial to compare the recovery period between two techniques because we did not study this aspect of the modified technique. The findings from this experimental model on chicken breast, as well as direct feedback from our patients, suggest that the modified Quadrapolar technique could provide a longer lasting pain relief to individuals with LBP caused by the SI joint dysfunction, as well as a shortened recovery period.
To date, we have performed the modified technique on >50 patients with LBP due to SI joint dysfunction. The results show that we could potentially extend the duration of relief and reduce the soft tissue trauma because of fewer needle puncture sites. Retrospectively, in 2015, an internal quality control survey of the first 52 patients showed the satisfaction rate was 96.4%. We defined “patient’s satisfaction” as 50% pain reduction on average (unpublished data, internal audit of the practice at Allevio Pain Management Clinic). Retrospectively, in over 50 patients treated with this technique, 26 required a repeat procedure (September 2016), with the duration of improvement between 9 and 17 months.
Limitations
As the investigation of lesion size was done using an experimental model using chicken breast as a medium, we cannot confirm that lesion sizes will be identical in human tissue in vivo conditions. However, we expect that the relative differences in the surface area of lesions between the standard and modified techniques will be comparable in patients in vivo.
Future directions
The next step to this investigation will involve exploring the difference in patient outcomes between the two techniques in a randomized clinical trial. Outcome measures that must be investigated include duration of pain relief, magnitude of pain relief, and change in overall quality of life. In addition, an assessment of adverse events and recovery time following the procedure is required to examine whether the modified technique is associated with a decrease in adverse events and a shortened recovery period.
Conclusion
In this study, we compare methodological differences between the standard and modified Quadrapolar radiofrequency techniques. In addition, we present findings from an in vitro experimental model demonstrating that the modified technique produces larger ablative lesions compared to the standard Quadrapolar radiofrequency technique. Quadrapolar radiofrequency technique produces larger lesions than the standard Quadrapolar radiofrequency technique that would allow for greater ablation of nociceptive input. Further studies are required to evaluate whether this technique produces improved patient outcomes.
Acknowledgments
A sincere thanks to Modjeh Nassaj, Arya Safakish, Aryan Safakish, and Genane Loheswaran for their assistance and contributions during the lesioning experiment. A very special thanks to Dr Gil Faclier, MD; Dr Kevin Smith, MD; Dr Tina Emadi, MD; and Dr Morley-Forster, MD, for their assistance in editing the manuscript. A very sincere thanks to Diros Technology for allowing us to use their facilities to conduct the study.
Disclosure
The author reports no conflicts of interest in this work.
References
Frank JW, Brooker AS, DeMaio SE, et al. Disability resulting from occupational low back pain. Part II: What do we know about secondary prevention? A review of the scientific evidence on prevention after disability begins. Spine (Phila Pa 1976). 1996;21(24):2918–2929. | ||
Allegri M, Montella S, Salici F, et al. Mechanisms of low back pain: a guide for diagnosis and therapy. F1000Res. 2016;5:F1000 Faculty Rev-1530. | ||
Katz JN. Lumbar disc disorders and low-back pain: socioeconomic factors and consequences. J Bone Joint Surg Am. 2006;88(Suppl 2):21–24. | ||
Katz RT. Impairment and disability rating in low back pain. Clin Occup Environ Med. 2006;5(3):719–740, viii. | ||
Kitayuguchi J, Kamada M, Okada S, Kamioka H, Mutoh Y. Association between musculoskeletal pain and trips or falls in rural Japanese community-dwelling older adults: a cross-sectional study. Geriatr Gerontol Int. 2015;15(1):54–64. | ||
Karvelas DA, Rundell SD, Friedly JL, et al. Subsequent health-care utilization associated with early physical therapy for new episodes of low back pain in older adults. Spine J. 2017;17(3):380–389. | ||
Maigne JY, Aivaliklis A, Pfefer F. Results of sacroiliac joint double block and value of sacroiliac pain provocation tests in 54 patients with low back pain. Spine (Phila Pa 1976). 1996;21(16):1889–1892. | ||
Grob KR, Neuhuber WL, Kissling RO. [Innervation of the sacroiliac joint of the human]. Z Rheumatol. 1995;54(2):117–122. German. | ||
Fortin JD, Kissling RO, O’Connor BL, Vilensky JA. Sacroiliac joint innervation and pain. Am J Orthop (Belle Mead NJ). 1999;28(12):687–690. | ||
Yin W, Willard F, Carreiro J, Dreyfuss P. Sensory stimulation-guided sacroiliac joint radiofrequency neurotomy: technique based on neuroanatomy of the dorsal sacral plexus. Spine (Phila Pa 1976). 2003; 28(20):2419–2425. | ||
Nakagawa T. [Study on the distribution of nerve filaments over the iliosacral joint and its adjacent region in the Japanese]. Nihon Seikeigeka Gakkai Zasshi. 1966;40(4):419–430. Japanese. | ||
Forst SL, Wheeler MT, Fortin JD, Vilensky JA. The sacroiliac joint: anatomy, physiology and clinical significance. Pain Physician. 2006; 9(1):61–67. | ||
Szadek KM, Hoogland PV, Zuurmond WW, De Lange JJ, Perez RS. Possible nociceptive structures in the sacroiliac joint cartilage: an immunohistochemical study. Clin Anat.23(2):192–198. | ||
Damen L, Buyruk HM, Guler-Uysal F, Lotgering FK, Snijders CJ, Stam HJ. Pelvic pain during pregnancy is associated with asymmetric laxity of the sacroiliac joints. Acta Obstet Gynecol Scand. 2001; 80(11):1019–1024. | ||
Patel VB, Wasserman R, Imani F. Interventional therapies for chronic low back pain: a focused review (efficacy and outcomes). Anesth Pain Med. 2015;5(4):e29716. | ||
Townsend CA, Beauchamp RD, Evers BM, Mattox K. Sabiston Textbook of Surgery, 19th Edition. Philadelphia, PA: Elsevier Saunders; 2012. | ||
Cohen SP, Hurley RW, Buckenmaier CC 3rd, Kurihara C, Morlando B, Dragovich A. Randomized placebo-controlled study evaluating lateral branch radiofrequency denervation for sacroiliac joint pain. Anesthesiology. 2008;109(2):279–288. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.