Back to Journals » Clinical Ophthalmology » Volume 15
Comparison of Preoperative Measurements with Intraoperative Aberrometry in Predicting Need for Correction in Eyes with Low Astigmatism Undergoing Cataract Surgery
Authors Hovanesian JA
Received 7 April 2021
Accepted for publication 3 May 2021
Published 26 May 2021 Volume 2021:15 Pages 2189—2196
DOI https://doi.org/10.2147/OPTH.S314618
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
John A Hovanesian
Harvard Eye Associates, Laguna Hills, CA, USA
Correspondence: John A Hovanesian
Harvard Eye Associates, 23961 Calle Magdalena, Suite 300, Laguna Hills, CA, 92653, USA
Tel +1 949 951 2020
Email [email protected]
Purpose: To determine whether intraoperative aberrometry during cataract surgery measures higher levels of absolute astigmatism than preoperative biometry readings and which method yields a lower, final level of astigmatism if the two do not agree.
Patients and Methods: Retrospective record review of all patients who underwent uncomplicated cataract surgery from February 2015 to May 2019 with planned intraoperative aberrometry. Data analysis included preoperative keratometry, total astigmatism as measured by intraoperative aberrometry, intraocular lens model and power used, and postoperative manifest refraction ≥ 1 month after surgery. The primary outcome measure was the proportion of patients requiring astigmatism correction (≥ 0.5 D) when measured by preoperative keratometry vs intraoperative aberrometry. Secondary outcomes included postoperative residual astigmatism, where adjusted preoperative astigmatism fell below the 0.5 D threshold for treatment but the intraoperative measurement was ≥ 0.5 D or ≥ 1.0 D.
Results: A total of 451 patient records were evaluated. Intraoperative aberrometry measured statistically higher levels of mean astigmatism than keratometry (0.86 D vs 0.79 D, respectively; P < 0.0001) and significantly greater astigmatism among patients with 0.5– 1.5 D of adjusted preoperative astigmatism (P < 0.0001). Significantly more patients qualified for with-the-rule astigmatism correction when measured by intraoperative aberrometry (n=339; 75%) than by preoperative keratometry alone (n=314; 70%); P < 0.03. This difference did not hold for against-the-rule or oblique astigmatism. For patients whose preoperative biometry astigmatism differed from intraoperative biometry, final postoperative astigmatism was lower when corrected if the adjusted preoperative and intraoperative measurements had a vector difference of < 0.5 D, but there was no additional benefit in final astigmatism reduction when the vector difference was ≥ 0.5 D.
Conclusion: Using intraoperative biometry readings can produce lower postoperative astigmatism than using preoperative biometry readings, but caution should be used when interpreting intraoperative readings that disagree with preoperative measurements with a vector magnitude of > 0.5 D.
Keywords: aberrometry, astigmatism, cataract surgery, toric IOL
Plain Language Summary
Intraoperative biometry readings can help surgeons provide more accurate outcomes in astigmatism assessment and management, but when the preoperative biometric readings disagree with the intraoperative readings by more than 0.5D, caution should be used when revising a surgical strategy.
Introduction
Today’s refractive cataract surgery comes with high patient expectations to be spectacle-free after surgery.1 It is well accepted that a large percentage of patients scheduled to undergo cataract surgery have ≥1.0 D of astigmatism (and close to 22% have ≥1.5 D of astigmatism).2–4 Advances in preoperative measurements (including keratometry, corneal topography, and corneal tomography5–7) have helped cataract surgeons improve patient outcomes, but residual astigmatism can result in decreased patient satisfaction.
Anecdotal evidence suggests that the introduction of intraoperative aberrometry helped improve the accuracy of astigmatism correction with low-power toric intraocular lenses (IOLs) compared to using preoperative biometry alone. Studies by Woodcock8 and Hatch9 have supported this concept in patients requiring higher toric correction, but to this author’s knowledge no formal study has examined the accuracy of toric predictive power in patients with <1.5 D of astigmatism.
When the preoperative measurement of corneal astigmatism, adjusted for surgically induced astigmatism (SIA) and posterior corneal astigmatism, amounts to <0.5 D, many surgeons choose to leave astigmatism uncorrected. In such cases when the intraoperative reading shows more astigmatism, surgeons question which measurement to trust. This dilemma becomes more confusing when the difference between preoperative and intraoperative measurements is significant.
Measuring the optics of a living eye is, by its nature, subject to some variability. During surgery, some of this variability results from corneal hydration, dryness or irregularity of the ocular surface, intraocular pressure, and mechanical factors such as the placement of an eyelid speculum. When accepted techniques for performing intraoperative aberrometry are followed, however, these sources of variability can be controlled within reasonable limits to make the measurements trustworthy for treatment decisions. Indeed, a number of studies have demonstrated that by following accepted practices for intraoperative aberrometry, greater accuracy in the final refractive outcome is achieved compared to preoperative biometry alone.10,11
The purpose of this study was to determine whether the magnitude of astigmatism measured by intraoperative aberrometry was, on average, greater than that of preoperative optical biometry, as has been observed anecdotally by a number of experienced surgeons. This study also examined whether the direction of preoperative astigmatism (with-the-rule [WTR], against-the-rule [ATR], or oblique) influenced the difference in measured intraoperative astigmatism. Secondary analyses address the implications when preoperative and intraoperative measurements disagreed. When preoperative readings suggested no astigmatism correction was needed (adjusted cylinder <0.5 D) but intraoperative measurements suggested treatment was appropriate (cylinder ≥0.5 D), the option exists to follow the preoperative measurements and perform no astigmatic correction or to follow the intraoperative aberrometry reading and place a toric IOL or limbal relaxing incision (LRI). The final astigmatic outcome of each course of action was measured and compared.
Patients and Methods
Records of all patients who underwent uncomplicated cataract surgery by one surgeon (JAH) at Harvard Eye Associates (Laguna Hills, CA, USA) between February 2015 and May 2019, who had undergone intraoperative aberrometry, and who had postoperative manifest refraction data were acquired from the AnalyzOR database on site at Harvard Eye Associates. This single surgeon had significant previous experience using intraoperative aberrometry following established protocols of the manufacturer. The data collected included preoperative keratometry (collected with an IOLMaster 500, Carl Zeiss Meditec, Jena, Germany), total astigmatism (measured by the ORA device, Alcon Laboratories, Inc., Fort Worth, TX, USA), the IOL model and power used, and postoperative manifest refraction performed at least one month after surgery. Electronic health records on this same group of patients also were used to identify study variables that were not available in the ORA database, including whether astigmatic keratometry was performed, the axis of astigmatism correction (toric IOL or LRI placement) for cases where astigmatism correction was performed, and whether clinical examinations before or after surgery revealed any exclusion criteria. Records were combined in a single table in Excel for analysis.
Patient records were excluded if eyes had undergone either femtosecond laser cataract surgery or previous refractive surgery. Also excluded were patient records with visually significant comorbidities of the cornea, retina, or optic nerve disease that had the potential to affect visual outcomes or ability to be refracted after surgery. Finally, patient records were excluded if they had complications either during or after surgery (capsule tears, iris trauma, decentered IOL, cystoid macular edema, etc).
Preoperative/Intraoperative Keratometry Readings
Preoperatively, the Koch formula was used to calculate adjusted preoperative keratometry.12 Per that formula, to adjust for SIA, 0.2 D was added for WTR astigmatism (steep axis between 60° and 120°) and 0.2 D was subtracted for ATR astigmatism (axis between 0° and 30° or between 150° and 180°). This value of SIA had been previously validated for the surgeon (JAH) using the calculator available at www.doctor-hill.com. To further adjust for posterior corneal astigmatism, 0.5 D was subtracted from WTR and 0.5 D added to ATR.
The ORA device for intraoperative aberrometry obtains 40 consecutive measurements of refraction. The astigmatism component is reported as a single cylinder power and axis. It is the custom of the surgeon to rely upon the ORA reading for astigmatism magnitude and axis when formulating a final plan for LRI or toric IOL use. In a minority of cases, when the ORA reading was not used to guide astigmatism treatment, this was recorded in the medical record, and those eyes were excluded from evaluation in this study.
The primary outcome measure was to compare adjusted preoperative keratometry readings to intraoperative astigmatism measurements for the same patients to determine the mean magnitude of astigmatism in each patient by each method. Means were compared using a paired t-test.
The proportion of patients whose adjusted preoperative vs intraoperative astigmatism was ≥0.5 D were compared using McNemar’s test13 for paired, nominal data. A subanalysis evaluated differences in astigmatism among WTR, ATR, or oblique (31°–50° or 121°–150°).
Secondary outcome measures included final postoperative astigmatism outcomes when intraoperative readings suggested greater astigmatism (≥0.5 D or ≥1.0 D) than adjusted preoperative measurements (<0.5 D). It is common practice at this cataract practice to counsel patients preoperatively on the availability of surgical astigmatic correction with a toric IOL or LRI. The patient’s choice of a surgical option that included or did not include astigmatism correction (LRI or toric IOL) effectively randomized whether patients with ≥0.5 D of intraoperative cylinder received astigmatic correction. No patients in this analysis received both a toric IOL and LRI. Because patients with significant comorbidities were excluded from the study, it would be expected that both the group receiving and not receiving astigmatism correction would have similar characteristics.
Patient records were included for analysis if all of the following conditions were met:
- The adjusted preoperative magnitude of astigmatism was <0.5 D, indicating that astigmatism correction would not be warranted on a preoperative basis.
- The intraoperative magnitude of astigmatism was ≥0.5 D, indicating a need for astigmatic correction as measured by aberrometry.
The final one-month postoperative magnitude of refractive astigmatism was compared between patients who did vs did not have surgical astigmatism correction.
In each patient, the vector difference in astigmatism between adjusted preoperative and intraoperative measurements was also calculated. This allowed a subset analysis of those patients who had a small disagreement (a vector difference of <0.5 D) vs a larger disagreement (a vector difference of ≥0.5 D). Chi-squared testing for proportions was used to compare the “success” (achieving final refractive astigmatism ≤0.5 D) of treating vs not treating astigmatism in patient groups.
This study was performed under the supervision of WCB IRB (Santee, CA, USA) under protocol number 520190247 and was registered at clinicaltrials.gov under protocol # NCT04247152. It followed the principles of the Declaration of Helsinki. Informed consent was provided for surgery, but the data were anonymized for analysis purposes, and a HIPAA waiver was granted by the IRB exempting the study from requiring additional informed consent.
Results
The initial data query returned 688 patient records. Of these, 451 patients met the entry criteria. Table 1 summarizes patient characteristics and procedures performed. No statistically significant differences in groups were identified for any characteristics.
 |
Table 1 Patient Characteristics and Procedures Performed |
Primary Outcome
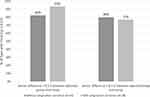
The mean magnitude of astigmatism was significantly greater when measured by intraoperative aberrometry than by adjusted preoperative biometry. Figure 1 shows the mean astigmatism by adjusted preoperative keratometry was 0.79 ± 0.42 D whereas intraoperative aberrometry showed a mean of 0.86 ± 0.48 D (P < 0.000001, paired t-test). Also, 339 eyes (75%) had a magnitude of astigmatism ≥0.5 D by intraoperative aberrometry and 314 eyes (70%) had a magnitude of astigmatism ≥0.5 D by adjusted preoperative biometry (P < 0.0001, McNemar’s test) See Figure 2.13
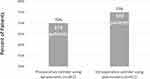 |
Figure 1 Intraoperative aberrometry measured statistically significantly higher levels of astigmatism vs preoperative keratometry. P < 0.0001 (McNemar’s test). |
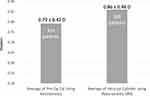 |
Figure 2 All patients combined: incidence of cylinder ≥ 0.5 D as measured by adjusted preoperative keratometry vs intraoperative aberrometry. P < 0.0001 (McNemar’s test). |
When preoperative adjusted keratometry was >1.0 D, there were no differences between the two measurement methods (Figure 3).
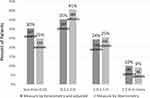 |
Figure 3 Magnitude of astigmatism is shown as measured by each method. P < 0.000001 paired t-test. |
Analysis by Axis of Astigmatism
The preoperative adjusted astigmatism included 147 patients (33%) with WTR, 213 patients (47%) with ATR, and 91 patients (20%) with oblique astigmatism. Table 2 shows the proportion of patients in each category who had cylinder ≥0.5 D with adjusted preoperative vs intraoperative aberrometry.
 |
Table 2 Distribution of Astigmatism Measurements by Axis of Astigmatism |
Compared to adjusted preoperative measurements, intraoperative aberrometry found astigmatism ≥0.5 D in significantly more patients with WTR and oblique astigmatism and significantly fewer patients with ATR astigmatism. Table 3 and Figure 4 show the comparisons.
 |
Table 3 Paired Distribution of Astigmatism Measurements by Axis of Astigmatism |
 |
Figure 4 The incidence of cylinder ≥ 0.5 D is shown in a subgroup analysis by axis of adjusted preoperative keratometry. P < 0.0001 McNemar’s test for all comparisons. |
Secondary Outcomes
Correcting astigmatism led to less final postoperative cylinder when the preoperative cylinder was <0.5 D and intraoperative cylinder was 0.5 D or more in most cases. Where the vector difference between preoperative and intraoperative measurements was <0.5 D, better results were achieved by following the guidance of intraoperative aberrometry, though the subgroup was too small to determine statistical significance. When the vector difference between preoperative and intraoperative readings was greater at ≥0.5 D, astigmatism correction had no effect on final cylinder. See Figure 5, which shows a favorable trend in final astigmatism is observed when intraoperative aberrometry guides correction in patients where the vector difference between adjusted preoperative and intraoperative cylinder is <0.5 D.
Discussion
Increasing postoperative satisfaction in patients with astigmatism requires a combination of accurate astigmatism measurement, preoperative marking,14,15 IOL selection,16,17 and IOL placement and rotation.18,19 Surgeons and their technicians generally take great care to optimize all parameters such as the ocular surface before biometry, yet this technique is limited by several factors. Ocular surface disruption can cause inaccuracy in keratometry.20 Posterior corneal astigmatism is also not measured by the keratometry function of current optical biometry systems. For these reasons, another diagnostic tool, intraoperative aberrometry, has been introduced to further refine patient outcomes.
Yesilirmak et al showed the benefits of using intraoperative aberrometry for toric IOL placement in eyes that had undergone previous refractive surgery.21 Anecdotal evidence suggests that use of intraoperative wavefront aberrometry for toric power selection could enhance the refractive outcomes and that the prediction error for the same implanted toric power was significantly lower using the intraoperative wavefront aberrometer compared with the toric IOL calculator.22 Conversely, Solomon et al found methods other than intraoperative aberrometry produced less remaining refractive cylinder.23 In both those analyses, patients were well beyond the traditional cutoff of 0.5 D for astigmatic correction at the time of surgery.
In this analysis, patients who presented with <0.5 D of astigmatism measured preoperatively were significantly more likely to have intraoperative astigmatism >0.5 D when the preoperative astigmatism was WTR or oblique in orientation. Furthermore, those who underwent astigmatic correction had lower final cylinder than untreated patients, suggesting that the intraoperative readings were more predictive of the final result. These findings suggest first that intraoperative aberrometry can enhance surgical outcomes even in cases of low astigmatism. They also suggest that even patients who would not normally be considered for astigmatism management (ie, those with <0.5 D of preoperative astigmatism) should be educated before cataract surgery about the potential options for treating astigmatism surgically, especially if their astigmatism is WTR or oblique.
Patients in this study with preoperative ATR astigmatism ≥0.5 D were significantly less likely to reach this level of astigmatism when evaluated with intraoperative aberrometry. This suggests that the Koch nomogram made adjustments for posterior corneal astigmatism that were too great, at least for this patient population.
As with preoperative astigmatism measurement, intraoperative aberrometry is not a perfect science. A number of factors can confound measurements, including ocular surface irregularities, irregular corneal hydration, low IOP, pressure from an eyelid speculum or other instruments, or others. Generally, an experienced user of intraoperative aberrometry can avoid these artifacts with caution in the prep of the eye, in the handling of the eye intraoperatively and particularly during aberrometry measurements. However, it is reasonable to expect that confounding influences can occur without the surgeon’s knowledge, and when preoperative measurements are thought to be reliable yet intraoperative measurements differ significantly, the latter should be considered with caution. In this study, when intraoperative aberrometry disagreed with adjusted preoperative biometry by a vector of magnitude of ≥ 0.5 D, there was no advantage to using intraoperative aberrometry to guide treatment of astigmatism over using preoperative measurements alone.
This study combined groups of patients whose astigmatism was treated by toric lenses and LRIs as one group. In fact, there may be differences in treatment accuracy between these two methods. To account for that, the same analysis was performed on each of the two groups. While the outcomes and trends mimicked the findings of the combined groups, the smaller number of patients in each of the individual groups reduced the statistical validity of the study. Future studies should include a larger number of patients in each group to be able to power each arm for statistical analysis.
This study is not without limitations, among them are those inherent in a retrospective record review. The retrospective nature of this study limited deeper analysis of some outcomes, eg, final toric IOL axis and final location and length of LRIs were not captured but might have influenced results. Exclusion of patients with “abnormal eyes” was based on recorded preoperative and intraoperative information, but this recorded information might not have included minor corneal irregularities or other variables that could have reduced the quality of ORA readings. In a prospective study, these variables could be captured and eyes excluded. Postoperative refractions recorded in the ORA database were performed in the typical time frame of 4 weeks after surgery, but these refractions can be influenced by a number of variables, including postop eye drop toxicity, ocular surface disease, patient compliance with postoperative treatment regimens, and the persistence of inflammation. However, these risks were mitigated to some extent by the large number of patient records.
In summary, using intraoperative biometry readings over preoperative biometry for astigmatism assessment and management provides better astigmatic outcomes in most cases, but caution should be advocated when interpreting intraoperative readings that disagree with preoperative measurements by >0.5 D.
Data Sharing Statement
The datasets used and/or analyzed for the purposes of this study are available from the corresponding author on reasonable request.
Ethics Approval and Informed Consent
This study was performed under the supervision of Aspire IRB (Santee, California) under Protocol ID “1909 ORA vs Biometry” and following the principles of the Declaration of Helsinki. Informed consent was provided for the surgery, but the data was anonymized for analysis purposes and exempt from additional informed consent.
Acknowledgments
This paper was presented as a poster at the 2020 ASCRS Virtual Symposium and at the 2019 American Academy of Ophthalmology meeting, also as a poster. Michelle Dalton, ELS, provided medical writing; this was funded by Research InSight, LLC.
Funding
This was an investigator-initiated study; limited funding was received from Alcon.
Disclosure
Dr Hovanesian reports grants from Alcon, during the conduct of the study. The author reports no other competing interests related to this work.
References
1. Saraiva J, Neatrour K, Waring GO
2. Ferrer-Blasco T, Montes-Mico R, Peixoto-de-matos SC, Gonzalez-Meijome JM, Cervino A. Prevalence of corneal astigmatism before cataract surgery. J Cataract Refract Surg. 2009;35(1):70–75. doi:10.1016/j.jcrs.2008.09.027
3. Khan MI, Muhtaseb M. Prevalence of corneal astigmatism in patients having routine cataract surgery at a teaching hospital in the United Kingdom. J Cataract Refract Surg. 2011;37(10):1751–1755. doi:10.1016/j.jcrs.2011.04.026
4. Michelitsch M, Ardjomand N, Vidic B, Wedrich A, Steinwender G. Pravalenz und Altersabhangigkeit von kornealem Astigmatismus bei Patienten vor Kataraktchirurgie [Prevalence and age-related changes of corneal astigmatism in patients before cataract surgery]. Ophthalmologe. 2017;114(3):247–251. doi:10.1007/s00347-016-0323-8
5. Kanellopoulos AJ, Asimellis G. Distribution and repeatability of corneal astigmatism measurements (Magnitude and Axis) evaluated with color light emitting diode reflection topography. Cornea. 2015;34(8):937–944. doi:10.1097/ico.0000000000000476
6. Bradley MJ, Coombs J, Olson RJ. Analysis of an approach to astigmatism correction during cataract surgery. Ophthalmologica. 2006;220(5):311–316. doi:10.1159/000094621
7. Yong Park C, Do JR, Chuck RS. Predicting postoperative astigmatism using Scheimpflug keratometry (Pentacam) and automated keratometry (IOLMaster). Curr Eye Res. 2012;37(12):1091–1098. doi:10.3109/02713683.2012.713158
8. Woodcock MG, Lehmann R, Cionni RJ, Breen M, Scott MC. Intraoperative aberrometry versus standard preoperative biometry and a toric IOL calculator for bilateral toric IOL implantation with a femtosecond laser: one-month results. J Cataract Refract Surg. 2016;42(6):817–825. doi:10.1016/j.jcrs.2016.02.048
9. Hatch KM, Woodcock EC, Talamo JH. Intraocular lens power selection and positioning with and without intraoperative aberrometry. J Refract Surg. 2015;31(4):237–242. doi:10.3928/1081597x-20150319-03
10. Cionni RJ, Dimalanta R, Breen M, Hamilton C. A large retrospective database analysis comparing outcomes of intraoperative aberrometry with conventional preoperative planning. J Cataract Refract Surg. 2018;44(10):1230–1235. doi:10.1016/j.jcrs.2018.07.016
11. Canto AP, Chhadva P, Cabot F, et al. Comparison of IOL power calculation methods and intraoperative wavefront aberrometer in eyes after refractive surgery. J Refract Surg. 2013;29(7):484–489. doi:10.3928/1081597X-20130617-07
12. Koch DD, Ali SF, Weikert MP, Shirayama M, Jenkins R, Wang L. Contribution of posterior corneal astigmatism to total corneal astigmatism. J Cataract Refract Surg. 2012;38(12):2080–2087. doi:10.1016/j.jcrs.2012.08.036
13. McNemar Q. Note on the sampling error of the difference between correlated proportions or percentages. Psychometrika. 1947;12(2):153–157. doi:10.1007/bf02295996
14. Cha D, Kang SY, Kim SH, Song JS, Kim HM. New axis-marking method for a toric intraocular lens: mapping method. J Refract Surg. 2011;27(5):375–379. doi:10.3928/1081597X-20101005-01
15. Popp N, Hirnschall N, Maedel S, Findl O. Evaluation of 4 corneal astigmatic marking methods. J Cataract Refract Surg. 2012;38(12):2094–2099. doi:10.1016/j.jcrs.2012.07.039
16. Visser N, Bauer NJ, Nuijts RM. Toric intraocular lenses: historical overview, patient selection, IOL calculation, surgical techniques, clinical outcomes, and complications. J Cataract Refract Surg. 2013;39(4):624–637. doi:10.1016/j.jcrs.2013.02.020
17. Kessel L, Andresen J, Tendal B, Erngaard D, Flesner P, Hjortdal J. Toric intraocular lenses in the correction of astigmatism during cataract surgery: a systematic review and meta-analysis. Ophthalmology. 2016;123(2):275–286. doi:10.1016/j.ophtha.2015.10.002
18. Kaur M, Shaikh F, Falera R, Titiyal JS. Optimizing outcomes with toric intraocular lenses. Indian J Ophthalmol. 2017;65(12):1301–1313. doi:10.4103/ijo.IJO_810_17
19. Miyake T, Kamiya K, Amano R, Iida Y, Tsunehiro S, Shimizu K. Long-term clinical outcomes of toric intraocular lens implantation in cataract cases with preexisting astigmatism. J Cataract Refract Surg. 2014;40(10):1654–1660. doi:10.1016/j.jcrs.2014.01.044
20. Trattler WB, Majmudar PA, Donnenfeld ED, McDonald MB, Stonecipher KG, Goldberg DF. The prospective health assessment of cataract patients’ ocular surface (PHACO) study: the effect of dry eye. poster. Clin Ophthalmol. 2017;11:1423–1430. doi:10.2147/OPTH.S120159
21. Yesilirmak N, Palioura S, Culbertson W, Yoo SH, Donaldson K. Intraoperative wavefront aberrometry for toric intraocular lens placement in eyes with a history of refractive surgery. J Refract Surg. 2016;32(1):69–70. doi:10.3928/1081597X-20151210-02
22. Krader CG Intraop wavefront aberrometry may enhance results in IOL surgery. Ophthalmology Times. Cleveland, OH: MJH Life Sciences; 2018. Available from: https://www.ophthalmologytimes.com/iols/intraop-wavefront-aberrometry-may-enhance-results-toric-iol-surgery.
23. Solomon JD, Ladas J. Toric outcomes: computer-assisted registration versus intraoperative aberrometry. J Cataract Refract Surg. 2017;43(4):498–504. doi:10.1016/j.jcrs.2017.01.012
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.