Back to Journals » Clinical Interventions in Aging » Volume 17
Comparison of Perioperative Outcomes in Patients Undergoing Short-Level Lumbar Fusion Surgery After Implementing Enhanced Recovery After Surgery: A Propensity Score Matching Analysis Focusing on Young-Old and Old-Old
Authors Cui P , Wang P, Hu X, Kong C, Lu S
Received 14 September 2022
Accepted for publication 27 November 2022
Published 5 December 2022 Volume 2022:17 Pages 1793—1801
DOI https://doi.org/10.2147/CIA.S389927
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Zhi-Ying Wu
Peng Cui,1,2,* Peng Wang,1,2,* Xinli Hu,1,2,* Chao Kong,1,2 Shibao Lu1,2
1Department of Orthopedics, Xuanwu Hospital, Capital Medical University, Beijing, People’s Republic of China; 2National Clinical Research Center for Geriatric Diseases, Beijing, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Chao Kong; Shibao Lu, Email [email protected]; [email protected]
Background: There were exponentially increased studies focused on revealing the satisfactory outcomes after implementing enhanced recovery after surgery (ERAS) in patients undergoing lumbar fusion surgery. However, little attention has been paid to the impact of chronologic age alone on perioperative outcomes.
Methods: In the present study, patients were dichotomized into two groups: young-old (65– 79 years), and old-old (80 years and older). Given the heterogeneity and age-related comorbidities in this population and the need to compare similar groups, we performed propensity score matching for gender, body mass index (BMI), operation time, American Society of Anesthesiologists (ASA) grade, Charlson Comorbidity Index (CCI), fusion levels and frail status. Perioperative outcomes were compared between two groups.
Results: In our study, we found there were significant discrepancies in length of stay (LOS) (7.17 ± 2.81 vs 8.11 ± 3.57 days, p = 0.031) and postoperative nausea and vomiting (3.7% vs 11.0%, p = 0.038); however, there were no significant differences in C-reactive protein (21.50 ± 26.52 vs 19.22 ± 22.04 mg/L, p = 0.490), overall complication rates (24.8% vs 33.0%, p = 0.179), ambulation time (2.89 ± 1.34 vs 2.55 ± 1.49 days, p = 0.078) or removal of urinary catheter time (2.47 ± 1.44 vs 2.32 ± 1.40 days, p = 0.446).
Conclusion: There were few differences in perioperative outcomes between young-old and old-old groups. Despite similar postoperative complication rates, the old-old group might experience longer LOS when complications occur. More importantly, current outcomes suggested that chronologic age alone does not appear to have the capacity to reflect the tolerance of elderly patients to surgery.
Keywords: enhanced recovery after surgery, propensity score matching, lumbar fusion surgery, elderly, postoperative outcomes
Introduction
It has been over twenty years since, enhanced recovery after surgery (ERAS), was first proposed.1 ERAS is a multimodal, multidisciplinary perioperative management strategy, with the purpose of reducing length of stay (LOS), perioperative adverse events and accelerating recovery, further shortening the hospitalization cost.2–6 Although, ERAS applied just in recent years, bright prospect is envisioned in spine surgery.2
According to the Seventh National Population Census in China, there were 264.02 million persons aged 60 and over, accounting for 18.7%, especially there were 190.64 million persons who were older than 65 years, accounting for 13.5%.7 The aging of the population and the associated comorbidities impose continued pressure on health-care resources. Especially in the context of the COVID-19 pandemic, it is of great importance to shorten LOS and accelerate bed turnover while assuring the quality of health care.8
Recently published consensus statement in lumbar spinal fusion provided explicit guidance for perioperative care.9 Implementing conventional perioperative management, studies reported satisfactory outcomes irrespective of LOS2,10,11 or hospitalization cost3,12 after implementing ERAS in spinal surgery. However, most of the studies were cross-sectional, which introduced confounding biases inevitably. Elderly patients are often recommended for conservative treatment, not least because of the higher incidence of postoperative adverse events after surgery in elderly patients. However, there have been conflicting findings regarding the influence of age on perioperative outcomes.13,14 Therefore, we used propensity score matching in this study to control for confounding factors when comparing the impact of age on perioperative outcomes after implementing ERAS.
Patients and Methods
Study Design
This was a retrospective, monocentric study. We retrospectively reviewed patients receiving short-level posterior lumbar fusion surgery between July 2020 and December 2021. Inclusion criteria were as follows: 1) diagnosis of lumbar disk herniation, lumbar spinal stenosis, or lumbar spondylolisthesis; 2) no history of spinal surgery; 3) age ≥65 years, and 4) short-level lumbar fusion surgery, defined as no more than two fusion levels. Exclusion criteria were 1) emergency surgery; 2) lack of clinical data; 3) combined surgery; and 4) other severe surgical contraindications. There were 559 patients with complete clinical data. As published previously, ERAS became routine in our department in January 2019.10,15 All patients in this study were treated according to strict adherence to the ERAS protocol and all surgeries were operated by the same experienced team. Details for short-level lumbar fusion surgery are displayed in Table 1. Then, we segregated patients into young-old (65–79 years), and old-old, (80 years and above).16
 |
Table 1 ERAS Items for Short-Level Lumbar Fusion Surgery |
Because this was a retrospective study, subject to confounding factors. In an effort to reduce the influence of selection bias when comparing between the groups, we performed 1:1 nearest-neighbor propensity score matching for gender, body mass index (BMI), operation time, American Society of Anesthesiologists (ASA) grade, Charlson Comorbidity Index (CCI),17 fusion levels and frail status, distinguished by Fried frailty phenotype18 to keep comparable physiological status at maximum extent. Match tolerance was set at 0.02. The institutional review board in Xuanwu Hospital Capital Medical University approved the study (No. 2018086), which followed the Declaration of Helsinki principles. Written informed consent was obtained from all participants.
Data Collection
All information relating to the patients was obtained from medical records. The collected clinical data included age, sex, BMI, operation time, comorbidity, fusion levels, 90-day readmission and frail status. To facilitate the statistical analysis of comorbidity, the CCI was used.17 LOS was defined as a period from postoperative day one to discharge. All patients were strictly subject to identical discharge criteria: no clinical complications requiring emergent measures; visual analog scale <3 on oral analgesics; independent ambulation or ambulation with minimal assistance; absence of fever in the previous 48 hours.19 As a routine postoperative laboratory examination item, CRP was extracted according to the result of the first laboratory test within two days of surgery.20 Urinary catheter extraction and postoperative mobilization time were also extracted. Postoperative complications included nausea and vomiting, delirium, hematoma, surgical site infection, cerebrospinal fluid leakage, urinary retention, urinary tract infection, sepsis, respiratory failure, deep venous thrombosis, and myocardial ischemia.
Statistical Analysis
Continuous variables were expressed as mean value ± standard deviation (mean ± SD) when the normal distribution was met, if not, median with interquartile range (IQR) was used. Continuous variables were analyzed using the two sample t-test or nonparametric Wilcoxon test, while statistical analysis for categorical variables was performed using the Chi-square test or the Fisher exact test. All statistical analyses were performed using SPSS software version 25.0 (SPSS, Inc., Armonk, NY, USA), and P-values <0.05 were considered statistically significant.
Results
Results of Propensity Score Matching
There were 599 patients enrolled in this study, 371 in young-old group (216 female) and 188 in old-old group (105 female), respectively. After propensity score matching, there were 109 well-balanced pairs of patients. The clinical characteristics of the 218 patients are displayed in Table 2.
 |
Table 2 Patients Characteristics Before and After Propensity Score Matching |
Perioperative Outcomes
The old-old group was more likely than the young-old group to have prolonged LOS (8.11 ± 3.57 vs 7.17 ± 2.81 days, p = 0.031). Delayed urinary catheter removal was more common in the old-old group, without a significant difference (2.47 ± 1.44 vs 2.32 ± 1.40 days, p = 0.446). Interestingly, we found that the young-old group appeared to have more severe stress responses (21.50 ± 26.52 vs 19.22 ± 22.04 mg/L, p = 0.490) and delayed mobilization (2.89 ± 1.34 vs 2.55 ± 1.49 days, p = 0.078) though no statistical difference. The detailed clinical characteristics are shown in Figure 1.
Complications
The postoperative complications are displayed in Table 3. There were no significant differences in 90-day readmission (6.4% vs 11.0%, p = 0.230). Except for nausea and vomiting (3.7% vs 11.0%, p = 0.038), all other complications were comparable between young-old and old-old, and there were no significant differences in overall postoperative complications between the groups (24.8% vs 33.0%, p = 0.179).
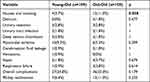 |
Table 3 Perioperative Complications for Propensity Score-Matched Patients |
Discussion
In the current study, after propensity score matching for sex, BMI, operation time, ASA, CCI, fusion levels and frail status, we found there was a significant difference in LOS between the young-old and old-old groups, further subjected to nausea and vomiting was observed in old-old. While there were no significant differences in CRP, 90-day readmission, postoperative ambulation time and removal of urinary catheter time.
ERAS is a multimodal, multidiscipline perioperative management that is superior to traditional management in reducing LOS and perioperative complications.2,5,21,22 With the continued aging population and the decline in physiological function, aging was considered as an obstacle preventing patients from surgery.23,24 Later, studies come to focus on the crucial importance of frail status and found frailty is a stronger predictor than age for perioperative outcomes,14,25,26 though there existing contradictory results.27 Therefore, in this study, in an effort to discuss the impact of chronologic age alone on perioperative outcomes after implementing ERAS, propensity score matching was utilized to offset confounding factors such as frailty status. According to the comparable physiological condition after propensity score matching, we found there were significant differences between the young-old and old-old groups in LOS and postoperative nausea and vomiting, which might be attributed to the decrease of physiological reserves and decreased tolerance to postoperative hyper-catabolism in this population.20
As an indicator to evaluate the stress response associated with surgery, CRP has been confirmed to be correlated with postoperative complications in previous studies,28–30 however, we found no significant difference in CRP between these two well-balanced groups. Besides, comparing with old-old, young-old even had severe stress response, though no significant difference, which may result from decreased organ function and activity to cytokine associated with stress response in the old-old group.20 Furthermore, according to our ERAS protocol (Table 1), patients receiving short-level lumbar fusion surgery were advocated to ambulate and have the urinary catheter removed on postoperative day one following recently published consensus statement for perioperative care in lumbar spinal fusion,9 which was not an ERAS item based on age- or sex-specific. Hence, we expected that there would be no significant difference in ambulation and urinary catheter removal time between the young-old and old-old groups. Interestingly, the old-old patients seemed to have earlier ambulation than their young-old counterparts. One possible explanation is that the old-old group might have endured longer symptom duration than the young-old group and would be more eager to ambulate.
In a retrospective cross-section study of one- to three-level lumbar fusion surgery among young-old patients, Brusko et al conducted that there was a significant reduction in LOS after implementing ERAS.11 Furthermore, in a retrospective cohort study published by our department previously, we proposed that patients older than 75 years receiving multi-segment lumbar fusion surgery can also benefit from ERAS.15 However, studies focusing on implementing ERAS among 80 years and older in spine surgery remain limited. A study of patients age 65 and older undergoing posterior lumbar fusion surgery, Hersey et al concluded that longer operation time is independently associated with increased complication rate.31 Meanwhile, in a retrospective study, Kuo et al revealed that age ≥65 years, time to ambulation and total operation time were independent predictors for extended LOS.32 What is more, in a retrospective study, Chan et al showed that elderly patients were at increased risk of developing postoperative complications and longer hospital stay.33 Retrospective studies are subject to selection and confounding biases inevitably. Hence, in order to reduce the influence of confounding factors, propensity score matching to keep similar physiological condition was used. The results showed that there were no significant differences in overall complications, except for LOS and nausea and vomiting. Postoperative nausea and vomiting was not a risk for discharge according to our discharge criteria; and the baseline characteristics of matched patients were well balanced. Therefore, we speculate that though comparable postoperative complication rates (Table 3), once occurred in the old-old, which might lead to a longer LOS (Figure 1). Therefore, more attention should be paid to preventing the occurrence of postoperative complications in the old-old. More importantly, current outcomes suggested that chronologic age alone seems not to have the capacity to reflect the tolerance of surgical interventions in elderly patients. Future studies should use an integrated and coordinated evaluation tool such as comprehensive geriatric assessment to provide personalized care for the surgical elderly individual.
There were some limitations in the current study. First, there were 599 patients enrolled in this study, after propensity score matching, only there were 109 well-balanced pairs of patients, which limited the robustness of current conclusions caused by insufficient statistical power due to a small sample size. Second, this was not a randomized controlled study and was subject to inherent limitations associated with retrospective analysis despite propensity score matching was used to offset confounding factors, there still remains bias in this study. Further, a prospective study with a large sample size should be performed to validate our findings.
Conclusions
In our study, we found there were no significant differences in CRP, postoperative ambulation time, removal of catheter time, 90-day readmission or overall complications between young-old and old-old groups after propensity score matching, while there existing significant differences in LOS and nausea and vomiting. Therefore, we speculate that though comparable postoperative complication rates, once occurred in the old-old, which might lead to a longer LOS. More importantly, current outcomes suggested that chronologic age alone seems not to have the capacity to reflect the tolerance of elderly patients to surgery.
Data Sharing Statement
All the data used to support the findings of this study were included within the article.
Ethics Approval and Consent to Participate
The institutional review board in Xuanwu Hospital Capital Medical University approved the study (No. 2018086), which followed the Declaration of Helsinki principles. A written informed consent was obtained from all participants in this study.
Acknowledgments
We thank the Department of Orthopedics, Xuanwu Hospital Capital Medical University staff and all the patients who participated in the study. In addition, special thanks to Lijuan Yang for help in retrieving the full text of some literatures.
Funding
This work was supported by the Beijing Municipal Health Commission (Jing 2019-2), Beijing Hospitals Authority’s Ascent Plan (DFL20190802) and Beijing Hospitals Authority Clinical Medicine Development of Special Funding Support (XMLX202116). The funders played no role in the design of this study, the collection, analysis and interpretation of data, or preparation of the manuscript.
Disclosure
Peng Cui, Xinli Hu and Peng Wang are co-authors. The authors declare that there are no conflicts of interest in this work.
References
1. Kehlet H. Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth. 1997;78:606–617. doi:10.1093/bja/78.5.606
2. Debono B, Corniola MV, Pietton R, et al. Benefits of enhanced recovery after surgery for fusion in degenerative spine surgery: impact on outcome, length of stay, and patient satisfaction. Neurosurg Focus. 2019;46(4):E6. doi:10.3171/2019.1.FOCUS18669
3. Staartjes VE, de Wispelaere MP, Schröder ML. Improving recovery after elective degenerative spine surgery: 5-year experience with an enhanced recovery after surgery (ERAS) protocol. Neurosurg Focus. 2019;46(4):E7. doi:10.3171/2019.1.FOCUS18646
4. D’Astorg H, Fiere V, Dupasquier M, et al. Enhanced recovery after surgery (ERAS) protocol reduces LOS without additional adverse events in spine surgery. Orthop Traumatol Surg Res. 2020;106(6):1167–1173. doi:10.1016/j.otsr.2020.01.017
5. Smith J, Probst S, Calandra C, et al. Enhanced recovery after surgery (ERAS) program for lumbar spine fusion. Perioper Med. 2019;8(4). doi:10.1186/s13741-019-0114-2
6. Michael Y, Wang M, Peng-Yuan Chang M, et al. Development of an Enhanced Recovery After Surgery (ERAS) approach for lumbar spinal fusion. J Neurosurg Spine. 2017;26(4):411–418. doi:10.3171/2016.9.SPINE16375
7. Tu WJ, Zeng X, Liu Q. Aging tsunami coming: the main finding from China’s seventh national population census. Aging Clin Exp Res. 2022;34(5):1159–1163. doi:10.1007/s40520-021-02017-4
8. Ljungqvist O, de Boer HD, Balfour A, et al. Opportunities and challenges for the next phase of enhanced recovery after surgery: a review. JAMA Surg. 2021;156(8):775–784. doi:10.1001/jamasurg.2021.0586
9. Debono B, Wainwright TW, Wang MY, et al. Consensus statement for perioperative care in lumbar spinal fusion: enhanced Recovery After Surgery (ERAS(R)) Society recommendations. Spine J. 2021;21(5):729–752.
10. Li Z, Lu S, Kong C, et al. Comparative short-term outcomes of enhanced recovery after surgery (ERAS) program and non-ERAS traditional care in elderly patients undergoing lumbar arthrodesis: a retrospective study. BMC Musculoskelet Disord. 2021;22(1):283. doi:10.1186/s12891-021-04166-z
11. Brusko GD, Kolcun JPG, Heger JA, et al. Reductions in length of stay, narcotics use, and pain following implementation of an enhanced recovery after surgery program for 1- to 3-level lumbar fusion surgery. Neurosurg Focus. 2019;46(4):E4. doi:10.3171/2019.1.FOCUS18692
12. Angus M, Jackson K, Smurthwaite G, et al. The implementation of enhanced recovery after surgery (ERAS) in complex spinal surgery. J Spine Surg. 2019;5(1):116–123. doi:10.21037/jss.2019.01.07
13. Moguilner S, Knight SP, Davis JRC, et al. The importance of age in the prediction of mortality by a frailty index: a machine learning approach in the Irish longitudinal study on ageing. Geriatrics. 2021;6(3). doi:10.3390/geriatrics6030084
14. Wolf JH, Hassab T, D’Adamo CR, et al. Frailty is a stronger predictor than age for postoperative morbidity in Crohn’s disease. Surgery. 2021;170(4):1061–1065. doi:10.1016/j.surg.2021.04.030
15. Cui P, Wang P, Kong C, et al. Patients older than 75 years undergoing polysegmental lumbar fusion surgery can also benefit from enhanced recovery after surgery program. Clin Interv Aging. 2022;17:245–252. doi:10.2147/CIA.S353511
16. Ho V, Chen C, Ho S, et al. Healthcare utilisation in the last year of life in internal medicine, young-old versus old-old. BMC Geriatr. 2020;20(1):495. doi:10.1186/s12877-020-01894-0
17. Charlson ME, Pompei P, Ales KL, et al. A new method of classifying pronnostic comorbidity in long itudinal studies: development and validation. Pergamon J. 1987;40:373–383.
18. Fried L, Tangen C, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol a Biol Sci Med Sci. 2001;56(3):M146–M156. doi:10.1093/gerona/56.3.M146
19. Li Z, Lu S, Kong C, et al. Impact of compliance with an enhanced recovery after surgery program on the outcomes among elderly patients undergoing lumbar fusion surgery. Clin Interv Aging. 2020;15:2423–2430. doi:10.2147/CIA.S286007
20. Cusack B, Buggy DJ. Anaesthesia, analgesia, and the surgical stress response. BJA Educ. 2020;20(9):321–328. doi:10.1016/j.bjae.2020.04.006
21. Soffin E, Vaishnav A, Wetmore D, et al. Design and Implementation of an Enhanced Recovery After Surgery (ERAS) program for minimally invasive lumbar decompression spine surgery: initial experience. Spine. 2019;44(9):E561–E570. doi:10.1097/BRS.0000000000002905
22. Fiasconaro M, Wilson LA, Bekeris J, et al. Enhanced recovery implementation and perioperative outcomes in posterior fusion patients. Spine. 2020;45(16):E1039–E1046. doi:10.1097/BRS.0000000000003495
23. Santarpino G, Condello I, Serraino GF, et al. Age, comorbidities, frailty: who comes first? J Card Surg. 2021;36(7):2407–2409. doi:10.1111/jocs.15543
24. Goshtasbi K, Birkenbeuel JL, Abiri A, et al. The association of frailty, age, and ASA classification with postoperative outcomes in endoscopic sinus surgery. Int Forum Allergy Rhinol. 2021;11(11):1596–1598. doi:10.1002/alr.22829
25. Niemelainen S, Huhtala H, Andersen J, et al. The Clinical Frailty Scale is a useful tool for predicting postoperative complications following elective colon cancer surgery at the age of 80 years and above: a prospective, multicentre observational study. Colorectal Dis. 2021;23(7):1824–1836. doi:10.1111/codi.15689
26. Shahrestani S, Ton A, Chen XT, et al. The influence of frailty on postoperative complications in geriatric patients receiving single-level lumbar fusion surgery. Eur Spine J. 2021;30(12):3755–3762. doi:10.1007/s00586-021-06960-8
27. Elsamadicy A, Freedman I, Koo A, et al. Modified-frailty index does not independently predict complications, hospital length of stay or 30-day readmission rates following posterior lumbar decompression and fusion for spondylolisthesis. Spine J. 2021;21(11):1812–1821. doi:10.1016/j.spinee.2021.05.011
28. Cabellos Olivares M, Labalde Martinez M, Torralba M, et al. C-reactive protein as a marker of the surgical stress reduction within an ERAS protocol (Enhanced Recovery After Surgery) in colorectal surgery: a prospective cohort study. J Surg Oncol. 2018;117(4):717–724. doi:10.1002/jso.24909
29. Kim J, Jung J, Lee J, et al. Can whole spine magnetic resonance imaging predict radiographic progression and inflammatory activity in axial spondyloarthritis? Joint Bone Spine. 2022;89(4):105352. doi:10.1016/j.jbspin.2022.105352
30. Hoeller S, Roch P, Weiser L, et al. C-reactive protein in spinal surgery: more predictive than prehistoric. Eur Spine J. 2021;30(5):1261–1269. doi:10.1007/s00586-021-06782-8
31. Hersey AE, Durand WM, Eltorai AEM, et al. Longer operative time in elderly patients undergoing posterior lumbar fusion is independently associated with increased complication rate. Global Spine J. 2019;9(2):179–184. doi:10.1177/2192568218789117
32. Kuo CC, Hess RM, Khan A, et al. Factors affecting postoperative length of stay in patients undergoing anterior lumbar interbody fusion. World Neurosurg. 2021;155:e538–e547. doi:10.1016/j.wneu.2021.08.093
33. Chan DKH, Ang JJ, Tan JKH, et al. Age is an independent risk factor for increased morbidity in elective colorectal cancer surgery despite an ERAS protocol. Langenbecks Arch Surg. 2020;405(5):673–689. doi:10.1007/s00423-020-01930-y
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

