Back to Journals » Clinical Ophthalmology » Volume 16
Comparison of Iridocorneal Angle Assessments in Open-Angle Glaucoma and Ocular Hypertension Patients: Anterior Segment Optical Coherence Tomography and Gonioscopy
Authors Craven ER, Chopra V, Goldberg JL, Marion KM, Chen X, Chang CT, Chen MY
Received 2 June 2021
Accepted for publication 3 March 2022
Published 27 April 2022 Volume 2022:16 Pages 1301—1312
DOI https://doi.org/10.2147/OPTH.S322962
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Scott Fraser
E Randy Craven,1 Vikas Chopra,2 Jeffrey L Goldberg,3 Kenneth M Marion,4 Xiaoming Chen,5 Cheng-Tao Chang,6 Michelle Y Chen6
1Johns Hopkins University School of Medicine, Baltimore, MD, USA; 2Doheny Eye Center UCLA, Pasadena, CA, USA; 3Byers Eye Institute at Stanford University, Palo Alto, CA, USA; 4Doheny Eye Institute, Los Angeles, CA, USA; 5West China Hospital Sichuan University, Sichuan, People’s Republic of China; 6Allergan, an AbbVie Company, Irvine, CA, USA
Correspondence: E Randy Craven, 600 N. Wolfe Street, Baltimore, MD, 21287, USA, Tel +1 240-482-1100, Fax +1 240-482-1105, Email [email protected]
Purpose: To quantitatively compare iridocorneal angle assessments using gonioscopy and anterior segment optical coherence tomography (AS-OCT).
Patients: US and Chinese patients with open-angle glaucoma (OAG) and/or ocular hypertension (OHT).
Methods: Analysis was pooled from 2 multicenter, noninterventional studies conducted in the US and China. Gonioscopy Shaffer grade and an AS-OCT method that approximates the angle width relative to local morphologic variations were compared by measuring the same iridocorneal angles. A third, separate, single-center, noninterventional study was conducted to verify results observed from the pooled analysis.
Results: From the pooled studies, a total of 239 eyes were measured using Shaffer grade and AS-OCT. Of these, 6 were Shaffer grade 2, 37 in Shaffer grade 3, and 196 in Shaffer grade 4. There was a trend of increasing Shaffer grade with increasing AS-OCT angle width. Open iridocorneal angles, Shaffer grade ≥ 3, had a ∼ 98% sensitivity and 88% positive predictive value for identifying AS-OCT angle width ≥ 300 μm, using the AS-OCT method. To verify these results, a total of 28 right eyes were imaged for the third study. A trend of increasing Shaffer grade with increasing AS-OCT angle width was observed, and angles with Shaffer grade ≤ 2 had AS-OCT angle width < 300 μm.
Conclusion: The AS-OCT method can determine the space in the anterior chamber and can potentially identify angles that are the appropriate size for certain glaucoma devices. Information gathered from AS-OCT can provide additional comprehensive and quantitative assessment to gonioscopy.
Keywords: gonioscopy, anterior segment optical coherence tomography, angle assessment, open-angle glaucoma
Introduction
Gonioscopy, as well as other imaging modalities (such as ultrasound biomicroscopy [UBM] and anterior segment optical coherence tomography [AS-OCT]), have been widely used to assess the anterior chamber angle (ACA) to determine the type of glaucoma and the most appropriate treatment option for a patient. The difference between the two main anatomic definitions of glaucoma, primary open-angle glaucoma (OAG) and primary angle-closure glaucoma (ACG), lies in the ACA.1–4 In recent years, more glaucoma treatment options, such as minimally invasive glaucoma surgeries (MIGS), tubes, and drug delivery implants, have become available. To benefit from certain devices and safely determine the most appropriate treatment option, the iridocorneal angle width (space) must be large enough to safely accommodate them.5 If the device contacts the corneal endothelium, it can cause corneal edema, and if it impacts the iris, it can cause anterior chamber inflammation, and potentially, visual loss. A recent study reported that corneal endothelial cell density loss may be inadvertently caused by selective laser trabeculoplasty (SLT) lasers that have a spot size of 400 µm, and in some eyes, the angle opening is less than 400 µm.6 No study has analyzed the space between the iris and the cornea to determine which device should be used in a specific patient. Although gonioscopy is the current gold standard for assessing the ACA,7 AS-OCT has also been widely used due to recent advancements and new features made for ACA assessment. This study was designed to evaluate an AS-OCT method that is different and simpler than other assessments. The findings were compared to standard gonioscopy grading.
Indirect gonioscopy is a contact method performed by placing a goniolens on the patient’s cornea while the patient is seated at the slit lamp. It allows for a 360-degree assessment of the angle width and provides dynamic visual information, such as changes during compression. During gonioscopy, areas of synechiae (angle-closure) can be identified by gently pushing on the eye. Neovascular and pseudoexfoliation signs can also be visually identified during gonioscopy.8 In regards to ACA devices, such as aqueous bypass shunts and stents or intracameral implants, it can provide clinicians with an idea of whether the angle devices may fit. There are many standard grading systems for gonioscopy, such as Scheie, Shaffer, and Spaeth. Each method is categorical and determines how open the angle might be. Shaffer grade is based on the angle between the iris and trabecular meshwork and provides a basic approach to determining the space in that angle.9 Although gonioscopy is the gold standard, there are some issues with the technique. For example, the requirement for direct contact with the eye may slightly change the angle shape due to compression artifact, which may lead to false impressions of the angle width. In addition, some patients find it uncomfortable,10 and gonioscopy is highly subjective and not quantitative.10–12 It may also underrepresent anatomic variation of the ACA when compared to other methods such as AS-OCT.13 Gonioscopy may not be able to provide the quantitative information required to accurately assess if an angle can accommodate a specific angle device.
AS-OCT is a non-contact (avoiding inadvertent compression) imaging technique that produces high resolution, cross-sectional images of the anterior chamber through optical backscattering of light (reflections).14 It can be performed with dim or bright light to see the differences in the angle. These objective, high-resolution images can accurately measure the angle width using the scleral spur or Schwalbe line as a landmark15–17 and can be analyzed qualitatively and quantitatively by automated image analysis software.14,18 Quantification of anterior chamber angle parameters have been shown to have high repeatability and reproducibility with OCT devices.19–22 A potential drawback for using AS-OCT is that it only provides a cross sectional image of a particular area and local morphological variability can affect interpretation of the condition. Differences between eye quadrants can also increase this difficulty.23–28
A more precise way of measuring the ACA, rather than using large categories or identifying it as open or closed, is needed to better determine the most appropriate treatment option. AS-OCT is a simple tool that can be implemented in the clinic to help bridge this knowledge gap. As it becomes adopted into practice, it is important to understand how measurements obtained from AS-OCT are related to and compare with gonioscopy observations and classifications. The two methods may provide complementary information. Together, they can improve the overall picture of the ACA, and this information can be used to help make treatment decisions. In this study, a simple AS-OCT method was introduced to potentially reduce measurement variability due to morphological differences, such as iris bumps and corneal curvatures. We compared the AS-OCT angle width measurements with the Shaffer grades obtained using gonioscopy to see how the two methods are correlated. The AS-OCT method has the potential to provide a more objective and quantitative ACA measurement. The purpose of this study was to evaluate the AS-OCT method for determining the space in the anterior chamber compared to gonioscopy. One use for determining the space in the anterior chamber is to identify angles that are the appropriate size for certain glaucoma devices, such as MIGS, tubes, and drug delivery implants.
Methods
This paper includes data from three studies that were conducted to evaluate the AS-OCT method in different populations. The studies were conducted in compliance with Good Clinical Practice (GCP) and in accordance with the Declaration of Helsinki. Investigators obtained approval of the study from an Institutional Review Board (IRB) (Chesapeake Research Review, Inc., Columbia, MD) or Independent Ethics Committees (IEC) (Ethics Committee of West China Hospital, Sichuan University, Sichuan, China; Ethics Committee of Beijing Tongren Hospital, Beijing, China; Ethics Committee of the Eye and ENT Hospital of Fudan University, Shanghai, China) prior to study initiation at each site. Written informed consent was obtained at the first study visit.
Analyses were conducted in two parts. In the first part, data from two multicenter, noninterventional, prospective studies, with a similar design, were pooled and presented together. Asian patients had been reported to be at higher risk of corneal contact with angle devices due to shallower iridocorneal angles;29–31 to account for this factor, both US and Chinese patients were studied. One of the two multicenter studies was conducted at three sites in China (NCT01781962) and the second at three sites in the US (NCT01540370); hereon the first part of the paper is referred to as the pooled study. To help validate the pooled study, data from a single-center, noninterventional, prospective study was analyzed independently; hereon the study is referred to as the single-center study.
For the pooled study, inclusion criteria included adult patients (≥18 years of age) who had been diagnosed with OAG or OHT in both eyes. Patients needed to be able to understand and be willing to follow study instructions as well. Patients were excluded if they had a known allergy or sensitivity to diagnostic agents used in the study, any changes in eye medication within 7 days prior to the examination day, intraocular surgery within 3 months prior to examination day, corneal or other ocular abnormalities, active or recurrent ocular disease, or wearing or anticipated wear of contact lenses during the study. In addition, patients were also excluded if there was a history of angle recession, narrow angle or angle-closure glaucoma (having a Shaffer grade ≤1), peripheral anterior synechia in the inferior angle, trabeculectomy or other types of incisional glaucoma surgery, or intraocular surgery resulting in cornea, angle, or iris trauma that altered the normal anterior segment anatomy. Inclusion and exclusion for the single-center study was the same as the pooled study, other than the inclusion of narrow angles (having a Shaffer grade ≤1) in the single-center study. To first determine if the AS-OCT method can be used to determine open angles, narrow angle and ACG patients were excluded from the pooled study. To verify the results from the pooled study and determine if the method was applicable to patients with narrow angles, the single center study was conducted and included narrow angle patients. Pseudophakia patients were allowed in all studies.
Patients who fit the eligibility criteria completed the screening visit, examination visit, and the study procedures within 5 weeks. Shaffer grade was determined using indirect gonioscopy with a mirrored Goniometric MV200 gonioscopy lens (Ocular Instruments, Inc.) and methylcellulose interface. The goniometric lens has a single mirror inclined at 62°, similar to a Goldmann one-mirror lens. Due to reports of variability in angle width between quadrants, and the fact that many anterior segment devices (including recently approved intracameral implants) reside in the inferior quadrant, only the inferior quadrant (6 o’clock angle) was measured to standardize the measurements in the pooled study. Shaffer grade (grade 0–4) is based on the angle between the iris and trabecular meshwork where the clinician approximates the angle at which the iris inserts relative to the trabecular meshwork. Grade 0 is the narrowest (smallest) angle described by the inability to identify the apex of the corneal wedge, while grade 4 is the widest angle with the ciliary body band easily visualized. The Shaffer grades 3 (20°-34°) and 4 >35°) refer to open-angles representing the angle between the iris and the meshwork to be ≥ 30° and without risk of angle-closure. Angles between 0° to 29° are classified as Shaffer grades 0, 1 (<10°) and 2 (10°-20°) and are considered either closed or have increased risk of angle-closure (Table 1). In clinical practice, it is common for a modified Shaffer grading system that combines the degrees of angle opening along with the visible angle structures to be used.9,32 At each site, gonioscopy was performed by the same investigator(s).
 |
Table 1 Description of the Shaffer Grading System |
AS-OCT images of the inferior angle were obtained using Zeiss Cirrus (Carl Zeiss Meditec, Dublin, CA) spectral domain high-definition optical coherence tomography by the same technician, when possible, at each study site. At least 3 images from each eye were captured using anterior segment 5-line raster with the scan lines bisecting the limbus at the 6 o’clock position. Both gonioscopy and AS-OCT were conducted at the same visit. The images were sent to an Image Review Committee (IRC) to evaluate the AS-OCT angle width. For this paper, an anatomic (space) interpretive method was used to determine the AS-OCT angle width (µm) to account for morphological variabilities. Unlike the other reported methods, such as AOD-SL (Angle opening distance at Schwalbe’s line), which is defined as the distance from the Schwalbe’s line to the iris surface that is perpendicular to a line drawn from scleral spur to Schwalbe’s line,16,33 this simple AS-OCT method approximates the iridocorneal angle width using the diameter of the largest circle that can fit between the point of contact at Schwalbe’s line and the iris (Figure 1A and B). Other methods, such as AOD-SL, can vary due to their dependency on the visibility of the morphology in the image and the identification of multiple landmarks in the eye. Figure 1A demonstrates how AOD-SL measurements of the same AS-OCT image can vary based on the grader’s interpretation. In addition, it can be challenging to identify the scleral spur due to morphological variability, and differences between the eye quadrants can increase this difficulty.23–26 Overall, due to the straightforward approach, our method can potentially reduce measurement variabilities due to morphological differences. For both the pooled study and the single-center study, gonioscopy and AS-OCT assessments were performed with the lights off.
All investigators who performed gonioscopy were masked to the AS-OCT evaluations and the technicians who performed the AS-OCT evaluations were masked to the results from the gonioscopy assessment. Gonioscopy was performed by the same investigator(s) at each site. Bilateral measurements were taken, and the right eye was selected as the study eye for all the analyses.
The purpose of the pooled study was to evaluate the AS-OCT method for determining the space in the anterior chamber and evaluate the relationship with gonioscopy grading. Distribution characteristics, sensitivity, positive predictive value (PPV), and negative predictive value (NPV) of Shaffer grading were evaluated using AS-OCT as the reference. The equations used to determine sensitivity, PPV, and NPV are in Table 2. An example of a 2×2 table used to determine the true positive (TP), true negative (TN), false positive (FP), and false negative (FN) values based on a Shaffer grade cut off value and angle width threshold, is shown in Table 3. In this paper, Shaffer grade 3 was used as the cut off value, as Shaffer grade ≥3 is the value that is considered an open iridocorneal angle not in danger of angle closure.9 Currently, most anterior chamber devices for glaucoma treatment, such as stents, are approved only for open angles.34–37 Sensitivity and PPV were calculated to determine the ability of the AS-OCT method to correctly identify the range of patients’ angle width based on Shaffer grades.
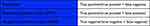 |
Table 2 Equations Used to Determine Sensitivity, PPV, and NPV |
 |
Table 3 Example of the 2×2 Table |
In the second part of the analysis, data from the single-center study were analyzed separately. The single-center study collected additional data on narrow angles and provided support to further verify the results of the pooled study. It also collected angle data from all four quadrants to investigate within eye variabilities and determine if the relationship between gonioscopy and the AS-OCT method is consistent between quadrants. Patients diagnosed with open-angle glaucoma were included, and patients with complete angle-closure were excluded due to AS-OCT imaging limitations. The iridocorneal angles were measured from images obtained from the GS-1, Nidek gonioscope (Nidek Co. LTD; Hiroishi-cho, Gamagori, Aichi, Japan) to determine Shaffer grades. The Nidek gonioscope is semi-automated, using controlled lighting and producing images that can be used for masked grading. It was chosen for the single-center study in hopes of providing more objective grading when compared to a standard mirrored gonioscopy. Images included 360-degrees of the iridocorneal angle and were assessed by a trained clinician masked to the AS-OCT results. For each eye, four Shaffer grades were provided based on four quadrants: Superior (12 o’clock), Inferior (6 o’clock), Nasal (3 o’clock), and Temporal (9 o’clock). AS-OCT images from both eyes were also taken with the Zeiss Cirrus OCT. The right eye was selected as the study eye for all the analyses. At least one 5-line raster image set was taken at each of the four quadrants (3, 6, 9, and 12 o’clock). The AS-OCT angle width was determined from the images using the method mentioned above by a masked grader.
Results
For the pooled study, a total of 304 patients enrolled in the two multicenter studies (NCT01781962, NCT01540370). Of those, 239 patients had both gonioscopy measurements and gradable AS-OCT images and were included in this analysis (Table 4). Of the 239 study eyes, 6 (2.5%), 37 (15.5%), and 196 (82.0%) patients had Shaffer grade 2, grade 3, and grade 4, respectively. The mean (SD) AS-OCT angle width for all graded study eyes was 598.3 (250.8) μm, the range was 73–1321 μm, and the median was 586.7 μm. Of note, the mean (SD) AS-OCT angle width was 647.8 (270.0) μm, and the median was 649.1 μm for all graded study eyes from the study conducted in China. Table 5 shows the range (min, max), median, and mean (SD) AS-OCT measurements within each Shaffer grade, and Figure 2 shows the distribution of AS-OCT measurements in each Shaffer grade. A trend of increasing AS-OCT measurements as Shaffer grade increases was observed. AS-OCT thresholds were selected to cover the range of the mean AS-OCT angle widths from Table 5 and for best correlation to Shaffer grade ≥3. Sensitivity values of the various AS-OCT thresholds are shown in Table 6, along with the positive and negative predictive values for each. As shown in Table 6, Shaffer grade ≥3 had high sensitivity (97.6%) with 88.0% PPV when predicting AS-OCT angle width ≥300 µm vs <300 µm. In addition, as AS-OCT angle width decreases, both TP and FN rates increase, and the FP rate decreases (Figure 2).
 |
Table 4 Patient Characteristics of the Pooled Study Population with at Least 1 Goniometric Measurement and Anterior Segment Optical Coherence Tomography |
 |
Table 5 The Range (Min, Max), Median, Mean (SD), and Number of AS-OCT Angle Width Measurements in Each Shaffer Grade from the Pooled Study |
 |
Table 6 The Sensitivity, PPV, and NPV at Different AS-OCT Angle Width Measurements (µm) Corresponding to Shaffer Grade ≥3 |
In the single-center study, there was a total of 28 patients with 21, 25, 17, and 26 measurements from the inferior, nasal, superior, and temporal quadrant, respectively. There was a total of 12, 8, and 69 measurements in Shaffer grade 2, 3, and 4, respectively. Most of the measurements, 65–88% from each quadrant, were Shaffer grade 4 and approximately 10–19% were Shaffer grade 2. Table 7 shows the distribution of Shaffer grades by quadrant and Figure 3 shows a visualization of the distribution of the AS-OCT angle width measurements in each Shaffer grade. Similar to the pooled study results, a trend of increasing AS-OCT measurements as Shaffer grade increases was observed. Any Shaffer grade <3, in any quadrant, had an AS-OCT angle width <300 µm ranging from 100.1 to 220.3 µm. The median and mean angle width was >300 µm for Shaffer grade ≥3 in all quadrants except for the nasal quadrant. The median and mean (SD) µm AS-OCT angle width for each Shaffer grade in each quadrant is provided in Table 8.
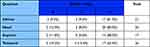 |
Table 7 Distribution (Percentage) of Shaffer Grade by Quadrant in the Single-Center Study |
 |
Table 8 The Median, and Mean (SD) AS-OCT Angle Width Measurements for Each Shaffer Grade by Each Quadrant in the Single-Center Study |
Discussion
Gonioscopy has been the standard for assessing iridocorneal angles. It provides a 360-degree view of the angle structures allowing clinicians to assess the angle opening grossly. AS-OCT provides an image of the iridocorneal angle with fine structural details at a specific location, which may be used to quantitatively assess the iridocorneal angle at the location of interest. Here, the AS-OCT method for quantitatively assessing the iridocorneal angle was described and found that it could be used to determine the space in the anterior chamber. The correlation of AS-OCT angle width measurements and what is commonly considered as an open iridocorneal angle using gonioscopy (Shaffer grade ≥3)9 indicates that the AS-OCT method has the potential to identify angles that are appropriate for certain glaucoma devices. Although previous studies have compared gonioscopy and AS-OCT to determine if each could distinguish between an open or closed angle,11,16,38–40 this paper used a quantitative approach to determine how standard gonioscopy grading scale measurements, Shaffer grade, correspond to AS-OCT angle width measurements. Overall, a trend of increasing AS-OCT angle width was observed as Shaffer grade measurements increases. To determine clinically relevant AS-OCT values, Shaffer grade 3 was used as the cut-off value for the analysis as it is the value that has been widely adopted for considering an iridocorneal angle as open.41 High sensitivity and PPV results, as well as acceptable TP and FP rates, indicated that with the AS-OCT method an angle width of ≥300 µm correlates well to an open angle. In addition, the results showed that it is complementary to gonioscopy, and the two methods can be used together to provide supplemental assessments for clinicians.
AS-OCT can provide finer detail and quantitative assessment if there is a specific area of interest, giving a better overall picture of the location when compared to gonioscopy. One limitation of the conventional AS-OCT angle quantification methods is the need to identify multiple morphological landmarks.23–28 Previous studies have shown that in about 20–25% of AS-OCT images, the scleral spur cannot be identified.24,25 In contrast, the method described in this study allows for angle approximation using the diameter of the largest circle that can fit between the point of contact at Schwalbe’s line and the iris, without the need to identify the scleral spur. This can potentially reduce measurement variability with a simple, easy approximation of the iridocorneal angle. Since most devices do not offer automatic angle measurements, this methodology overcomes one of the most common challenges for a clinician in using AS-OCT when measuring the iridocorneal angle. Placing a simple reticle overlay with a specific ACA width over the angle recess image could allow for very quick quantification of angle measurements. Quantification of the anterior chamber angle parameters has been shown to have high repeatability and reproducibility with OCT devices,19,20,22,42 and the AS-OCT method could provide a more simple, reliable, and precise way of measuring the ACA when compared to the categorical gonioscopy grades. In the future, it may be possible to use this AS-OCT method to determine the range of ACA widths that are suitable for specific anterior chamber devices. This information could better inform clinicians on the ACA when determining which patients should receive specific anterior chamber devices.
Previous work has shown that certain quadrants tend to have narrower angles than others, and the proportion of angles considered to be closed by gonioscopy differed by quadrant.38,43,44 Together gonioscopy and AS-OCT may provide insight into how variability within the eye affects angle measurements from different quadrants of the eye (inferior, superior, nasal, and temporal). To validate the pooled study results and to assess whether variability within the eye would affect the angle assessments, the single-center study was conducted. Results from the single-center study supported the pooled study findings regarding the relationship between gonioscopy and AS-OCT measurements. All measurements with Shaffer grade ≤2 had AS-OCT angle width <300 µm in all four quadrants. All quadrants followed the same trend seen in the pooled study; an increasing AS-OCT angle width was observed as Shaffer grade measurements increased. In general, results indicate that the relationship between gonioscopy and the AS-OCT method is similar in different quadrants, with the exception of the nasal quadrant where the median and mean AS-OCT angle width measurements were <300 µm in Shaffer grade 3. A limited number of patients were included in the single-center study, and additional studies that include narrow angles and investigate all quadrants should be conducted with a larger number of patients to confirm our results. Although previous studies have shown that the Chinese population has a larger percentage of narrower angles,29–31,45 the mean AS-OCT angle width from the study conducted in China was similar to the overall mean AS-OCT angle width of the US population. This is likely due to the inclusion criteria that patients were expected to have open angles. In addition, there have been growing rates of myopia incidence reported in the Chinese population from recent epidemiological studies.46,47 Therefore, our observation is consistent with larger angles observed in Chinese subjects, and our results are applicable for both American and Chinese populace.
There are several strengths to this study. One strength is that the data were pooled from studies with similar designs that were conducted at six sites in the US and China. Another is that all AS-OCT images were sent to an internal Image Review Committee (IRC) where two graders, masked to each other and to the gonioscopy results, graded the AS-OCT angle widths. Additionally, there was a wide distribution of AS-OCT angle width measurements, ranging from 73 μm to 1321 μm, showing that there was a diversity in angle size included in this study.
There are some limitations to this study, including the small sample from the single-center study and the small number of patients with Shaffer grade <3. Follow-up studies are needed to confirm our findings. Although the use of the Nidek gonioscope in the single-center study indicates that the relationship between gonioscopy and the AS-OCT method is consistent between different gonioscopy devices, the fact that two different gonioscopy devices were used could also be seen as a limitation. The Nidek is a semi-automated gonioscope, while a conventional mirrored gonioscopy was used in the pooled study. Both gonioscopy assessments utilize the same type of gonio lens. The semi-automated gonioscope has been suggested to have the potential to reduce interobserver and/or technique variability.48 However, how these two gonioscopy assessments compare to one another has not been fully determined. It should also be noted that glaucoma devices can be placed in the superior angle as well as the inferior angle, and that the presence of adequate space in the inferior angle does not indicate adequate space in the other angles. This should be borne in mind by clinicians wishing to use this method.
Conclusion
Although gonioscopy is the current standard method to assess angle width in clinical practice, AS-OCT is becoming more widely used. AS-OCT allows non-contact imaging of the angle and provides enhanced visualization of the angle for quantitative assessment. Information gathered from AS-OCT can be used to provide a comprehensive and quantitative assessment of the angle and can also be used to supplement gonioscopy assessment of the iridocorneal angle and thus help decision making regarding treatment. Overall, this study showed that this simple AS-OCT method could determine the space in the anterior chamber. Results also showed that an angle width of ≥300 µm measured with the AS-OCT method corresponds well to open iridocorneal angles (Shaffer grade ≥3), indicating that it has the potential to identify angles that are appropriate for certain glaucoma devices. This opens the possibility of using the AS-OCT angle width measurements to determine if the angle is suitable for a specific anterior chamber device. In the future, this method could provide a more simple and objective way of measuring the ACA and can complement gonioscopy assessment.
Abbreviations
ACA, anterior chamber angle; AS-OCT, anterior segment optical coherence tomography; ACG, angle-closure glaucoma; AOD-SL, Angle opening distance at Schwalbe’s line; IRC, Image Review Committee; FN, false negative; FP, false positive; OAG, open-angle glaucoma; OHT, ocular hypertension; NPV, negative predictive value; PPV, positive predictive value; SLT, selective laser trabeculoplasty; TN, true negative; TP, true positive; UBM, ultrasound biomicroscopy.
Data Sharing Statement
This clinical trial data can be requested by any qualified researchers who engage in rigorous, independent scientific research, and will be provided following review and approval of a research proposal and Statistical Analysis Plan (SAP) and execution of a Data Sharing Agreement (DSA). Data requests can be submitted at any time and the data will be accessible for 12 months, with possible extensions considered. For more information on the process, or to submit a request, visit the following link: https://www.abbvie.com/our-science/clinical-trials/clinical-trials-data-and-information-sharing/data-and-information-sharing-with-qualified-researchers.html.
Acknowledgments
Writing and editorial assistance was provided to the authors by Stephanie Kuwahara, PhD, of AbbVie Inc and Envision Scientific Solutions, Philadelphia, PA.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research was supported by Allergan (prior to its acquisition by AbbVie Inc). Employees of AbbVie participated in the research, interpretation of data, review of the manuscript, and the decision to submit for publication.
Disclosure
E. Randy Craven is a former employee of Johns Hopkins University School of Medicine, is currently employed by AbbVie Inc, and may hold AbbVie stock.
Vikas Chopra has received grant support and consulted for Allergan (an AbbVie company).
Jeffrey Goldberg has received grant and consulting fees from Allergan (an AbbVie company).
Cheng-Tao Chang is full-time employee of AbbVie Inc.
Michelle Chen is a former employee of AbbVie Inc. currently employed by Perfuse Therapeutics, Inc. and may hold AbbVie stock.
The authors report no other conflicts of interest in this work.
References
1. Weinreb RN, Aung T, Medeiros FA. The pathophysiology and treatment of glaucoma: a review. JAMA. 2014;311(18):1901–1911. doi:10.1001/jama.2014.3192
2. Smith SD, Singh K, Lin SC, et al. Evaluation of the anterior chamber angle in glaucoma: a report by the American Academy of Ophthalmology. Ophthalmology. 2013;120(10):1985–1997. doi:10.1016/j.ophtha.2013.05.034
3. Ishikawa H, Liebmann JM, Ritch R. Quantitative assessment of the anterior segment using ultrasound biomicroscopy. Curr Opin Ophthalmol. 2000;11(2):133–139. doi:10.1097/00055735-200004000-00012
4. Gupta D, Chen PP. Glaucoma. Am Fam Physician. 2016;93(8):668–674.
5. Lewis RA, Christie WC, Day DG, et al. Bimatoprost sustained-release implants for glaucoma therapy: 6-month results from a Phase I/II clinical trial. Am J Ophthalmol. 2017;175:137–147. doi:10.1016/j.ajo.2016.11.020
6. Craven ER, Christie WC, Chen MY, Gu X, Robinson MR, Wirta D. Corneal endothelial cell loss associated with selective laser trabeculoplasty.
7. Campa C, Pierro L, Bettin P, Bandello F. Anterior Chamber Angle Assessment Techniques. InTech; 2011.
8. Lin SC. Assessing the angle: which method is best? 2016. Available from: https://www.reviewofophthalmology.com/article/assessing-the-angle-which-method-is-best.
9. Alward WLM. Color Atlas of Gonioscopy. San Francisco, CA: Foundation of the American Academy of Ophthalmology; 2001.
10. Quek DT, Nongpiur ME, Perera SA, Aung T. Angle imaging: advances and challenges. Indian J Ophthalmol. 2011;59(Suppl):S69–75. doi:10.4103/0301-4738.73699
11. Rigi M, Bell NP, Lee DA, et al. Agreement between gonioscopic examination and swept source Fourier domain anterior segment optical coherence tomography imaging. J Ophthalmol. 2016;2016:1727039. doi:10.1155/2016/1727039
12. Raluca M, Mircea F, Andrei F, et al. Old and new in exploring the anterior chamber angle. Rom J Ophthalmol. 2015;59(4):208–216.
13. Xu BY, Pardeshi AA, Burkemper B, et al. Differences in anterior chamber angle assessments between gonioscopy, EyeCam, and anterior segment OCT: the Chinese American Eye Study. Transl Vis Sci Technol. 2019;8(2):5. doi:10.1167/tvst.8.2.5
14. Ang M, Baskaran M, Werkmeister RM, et al. Anterior segment optical coherence tomography. Prog Retin Eye Res. 2018;66:132–156. doi:10.1016/j.preteyeres.2018.04.002
15. Cheung CY, Zheng C, Ho CL, et al. Novel anterior-chamber angle measurements by high-definition optical coherence tomography using the Schwalbe line as the landmark. Br J Ophthalmol. 2011;95(7):955–959. doi:10.1136/bjo.2010.189217
16. Qin B, Francis BA, Li Y, et al. Anterior chamber angle measurements using Schwalbe’s line with high-resolution Fourier-domain optical coherence tomography. J Glaucoma. 2013;22(9):684–688. doi:10.1097/IJG.0b013e318264b921
17. Marion KM, Maram J, Pan X, et al. Reproducibility and agreement between 2 spectral domain optical coherence tomography devices for anterior chamber angle measurements. J Glaucoma. 2015;24(9):642–646. doi:10.1097/IJG.0000000000000303
18. Li H, Leung CK, Cheung CY, et al. Repeatability and reproducibility of anterior chamber angle measurement with anterior segment optical coherence tomography. Br J Ophthalmol. 2007;91(11):1490–1492. doi:10.1136/bjo.2007.118901
19. Pan X, Marion K, Maram J, et al. Reproducibility of anterior segment angle metrics measurements derived from Cirrus spectral domain optical coherence tomography. J Glaucoma. 2015;24(5):e47–51. doi:10.1097/IJG.0000000000000136
20. Maram J, Pan X, Sadda S, Francis B, Marion K, Chopra V. Reproducibility of angle metrics using the time-domain anterior segment optical coherence tomography: intra-observer and inter-observer variability. Curr Eye Res. 2015;40(5):496–500. doi:10.3109/02713683.2014.930155
21. Akil H, Dastiridou A, Marion K, Francis B, Chopra V. Repeatability, reproducibility, agreement characteristics of 2 SD-OCT devices for anterior chamber angle measurements. Can J Ophthalmol. 2017;52(2):166–170. doi:10.1016/j.jcjo.2016.08.019
22. Pan X, Maram J, Nittala MG, Francis BA, Chopra V, Sadda SR. Reproducibility and agreement of four anterior segment-optical coherence tomography devices for anterior chamber angle measurements. Graefes Arch Clin Exp Ophthalmol. 2020;258(7):1475–1481. doi:10.1007/s00417-020-04648-1
23. Maslin JS, Barkana Y, Dorairaj SK. Anterior segment imaging in glaucoma: an updated review. Indian J Ophthalmol. 2015;63(8):630–640. doi:10.4103/0301-4738.169787
24. Narayanaswamy A, Sakata LM, He MG, et al. Diagnostic performance of anterior chamber angle measurements for detecting eyes with narrow angles: an anterior segment OCT study. Arch Ophthalmol. 2010;128(10):1321–1327. doi:10.1001/archophthalmol.2010.231
25. Sakata LM, Lavanya R, Friedman DS, et al. Assessment of the scleral spur in anterior segment optical coherence tomography images. Arch Ophthalmol. 2008;126(2):181–185. doi:10.1001/archophthalmol.2007.46
26. Console JW, Sakata LM, Aung T, Friedman DS, He M. Quantitative analysis of anterior segment optical coherence tomography images: the Zhongshan angle assessment program. Br J Ophthalmol. 2008;92(12):1612. doi:10.1136/bjo.2007.129932
27. Marion KM, Niemeyer M, Francis B, Sadda SR, Chopra V. Effects of light variation on Schwalbe’s line-based anterior chamber angle metrics measured with cirrus spectral domain optical coherence tomography. Clin Exp Ophthalmol. 2016;44(6):455–464. doi:10.1111/ceo.12700
28. Shi Y, Marion KM, Jenkins D, Sadda S, Le PV, Chopra V. Identification and characterization of imaging technique errors and artifacts using anterior-segment OCT for irido-corneal angle evaluations in glaucoma. Ophthalmol Glaucoma. 2019;2(3):136–144. doi:10.1016/j.ogla.2019.02.006
29. Leung CK, Palmiero PM, Weinreb RN, et al. Comparisons of anterior segment biometry between Chinese and Caucasians using anterior segment optical coherence tomography. Br J Ophthalmol. 2010;94(9):1184–1189. doi:10.1136/bjo.2009.167296
30. Sihota R, Vashisht P, Sharma A, Chakraborty S, Gupta V, Pandey RM. Anterior segment optical coherence tomography characteristics in an Asian population. J Glaucoma. 2012;21(3):180–185. doi:10.1097/IJG.0b013e3182070cb1
31. Wang D, Chiu C, He M, Wu L, Kao A, Lin S. Differences in baseline dark and the dark-to-light changes in anterior chamber angle parameters in whites and ethnic Chinese. Invest Ophthalmol Vis Sci. 2011;52(13):9404–9410. doi:10.1167/iovs.11-8470
32. AbdElHakam OM, Abdelrahman R, Abdelrazek S, Eid A. Evaluation of the anterior chamber angle and filtering bleb morphology after phacotrabeculectomy by using anterior segment optical coherence tomography. J Egypt Ophthalmol Soc. 2018;111(4):137–143. doi:10.4103/ejos.ejos_22_18
33. Pan X, Maram J, Marion K, et al. Effect of angle of incidence on anterior chamber angle metrics from optical coherence tomography. J Glaucoma. 2016;25(1):e19–23. doi:10.1097/IJG.0000000000000169
34. Glaukos Corporation.Directions for use/package insert Glaukos® Corporation iStent® Trabecular Micro-Bypass System. 2016. Available from: https://www.glaukos.com/wp-content/uploads/2021/09/45-0074-Rev-6-Instructions-IFU-GTS100-RLI-Commercial-US.pdf. Accessed April 11, 2022.
35. Glaukos Corporation. Glaukos® Corporation iStent® Trabecular Micro-Bypass System. 2017 Available from: https://www.accessdata.fda.gov/cdrh_docs/pdf17/p170043c.pdf. Accessed April 11, 2022.
36. Alcon Laboratories Inc. Instructions for use: CyPass Micro-Stent. 2016. Available from:https://www.accessdata.fda.gov/cdrh_docs/pdf15/p150037d.pdf. Accessed April 11, 2022.
37. Allergan, Inc. Directions for use of the XEN Glaucoma Treatment System. 2017. Available from:https://allergan-web-cdn-prod.azureedge.net/actavis/actavis/media/allergan-pdf-documents/labeling/xen/dfu_xen_glaucoma_treatment_system_us_feb2017.pdf. Accessed April 11, 2022.
38. Sakata LM, Lavanya R, Friedman DS, et al. Comparison of gonioscopy and anterior segment ocular coherence tomography in detecting angle closure in different quadrants of the anterior chamber angle. Ophthalmology. 2008;115(5):769–774. doi:10.1016/j.ophtha.2007.06.030
39. Nolan WP, See JL, Chew PT, et al. Detection of primary angle closure using anterior segment optical coherence tomography in Asian eyes. Ophthalmology. 2007;114(1):33–39. doi:10.1016/j.ophtha.2006.05.073
40. Melese EK, Chan JD, Blieden LS, et al. Determination and validation of thresholds of anterior chamber parameters by dedicated anterior segment optical coherence tomography. Am J Ophthalmol. 2016;169:208–217. doi:10.1016/j.ajo.2016.06.032
41. Kaushik S, Jain R, Pandav SS, Gupta A. Evaluation of the anterior chamber angle in Asian Indian eyes by ultrasound biomicroscopy and gonioscopy. Indian J Ophthalmol. 2006;54(3):159–163. doi:10.4103/0301-4738.27065
42. Kim DY, Sung KR, Kang SY, et al. Characteristics and reproducibility of anterior chamber angle assessment by anterior-segment optical coherence tomography. Acta Ophthalmol. 2011;89(5):435–441. doi:10.1111/j.1755-3768.2009.01714.x
43. He M, Foster PJ, Ge J, et al. Gonioscopy in adult Chinese: the Liwan Eye Study. Invest Ophthalmol Vis Sci. 2006;47(11):4772–4779. doi:10.1167/iovs.06-0309
44. Kunimatsu S, Tomidokoro A, Mishima K, et al. Prevalence of appositional angle closure determined by ultrasonic biomicroscopy in eyes with shallow anterior chambers. Ophthalmology. 2005;112(3):407–412. doi:10.1016/j.ophtha.2004.10.026
45. Dastiridou A, Marion K, Niemeyer M, Francis B, Sadda S, Chopra V. Pilot study of the effects of ambient light level variation on spectral domain anterior segment OCT-derived angle metrics in Caucasians versus Asians. Curr Eye Res. 2018;43(7):955–959. doi:10.1080/02713683.2018.1464192
46. Wang J, Ying G-S, Fu X, et al. Prevalence of myopia and vision impairment in school students in Eastern China. BMC Ophthalmol. 2020;20(1):2. doi:10.1186/s12886-019-1281-0
47. Chen M, Wu A, Zhang L, et al. The increasing prevalence of myopia and high myopia among high school students in Fenghua city, eastern China: a 15-year population-based survey. BMC Ophthalmol. 2018;18(1):159. doi:10.1186/s12886-018-0829-8
48. Peroni A, Paviotti A, Campigotto M, et al. On clinical agreement on the visibility and extent of anatomical layers in digital gonio photographs. Transl Vis Sci Technol. 2021;10(11):1. doi:10.1167/tvst.10.11.1
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



