Back to Journals » Clinical Pharmacology: Advances and Applications » Volume 15
Comparison of Efficacy and Safety Between Dronedarone and Amiodarone Used During the Blind Period in Patients with Atrial Fibrillation After Catheter Ablation
Authors Li Y, Hu T, Lin M, Wang Q, Han W, Zhong J
Received 17 September 2023
Accepted for publication 1 December 2023
Published 8 December 2023 Volume 2023:15 Pages 113—123
DOI https://doi.org/10.2147/CPAA.S440704
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Arthur E. Frankel
Yihan Li,1 Tong Hu,1 Mingjie Lin,1,2 Qinhong Wang,1 Wenqiang Han,1 Jingquan Zhong1,2
1Department of Cardiology, Qilu Hospital of Shandong University, Jinan, Shandong Province, People’s Republic of China; 2Department of Cardiology, Qilu Hospital (Qingdao), Cheeloo College of Medicine, Shandong University, Qingdao, Shandong Province, People’s Republic of China
Correspondence: Jingquan Zhong, Department of Cardiology, Qilu Hospital of Shandong University, Jinan, Shandong Province, People’s Republic of China, Tel: +008618560086597, Email [email protected]
Background: Dronedarone is an effective drug for maintaining the sinus rhythm in patients with atrial fibrillation (AF). The efficacy and safety of dronedarone versus amiodarone in patients with AF after catheter ablation (CA) needs more evidence. We retrospectively compared the efficacy and safety of dronedarone and amiodarone in our hospital.
Methods: Patients who underwent CA from January 2021 to January 2022 and used dronedarone (n=229) or amiodarone (n=202) during the blind period were enrolled. The recurrence of AF in post-and during the blanking period was compared between the groups; the rehospitalization for re-ablation and adverse drug events (ADE) were also calculated.
Results: During an average follow-up period of 14.28 months, the long-term recurrence rate of AF did not differ significantly between the amiodarone group and dronedarone group (22.71% vs 21.29%, hazard ratio [HR], 1.033, 95% confidence interval [CI], 0.661– 1.614; p=0.888). The recurrence rate in the blanking period also showed no statistically significant differences between the amiodarone group and dronedarone group (9.90% vs 14.41%, HR, 0.851; 95% CI, 0.463– 1.564; p=0.604). The re-hospitalization rates for re-ablation between two groups did not differ between the amiodarone group and dronedarone group (4.65% vs 13.46%; p =0.144). The incidence of ADE was higher in the dronedarone groups than that in the amiodarone group (16.59% vs 5.45%, p < 0.001). The main adverse drug events in the dronedarone and amiodarone groups were gastrointestinal (6.99%) and bradycardia (2.48%), respectively.
Conclusion: Compared to the amiodarone group, the dronedarone group had a similar blank-period and long-term recurrence rate of AF and a higher incidence of ADE.
Keywords: atrial fibrillation, catheter ablation, amiodarone, dronedarone
Introduction
Atrial fibrillation (AF) is the most common cardiac arrhythmia and is associated with a higher incidence of stroke, heart failure and mortality.1 Guidelines recommend catheter ablation (CA) for symptomatic paroxysmal atrial fibrillation who does not respond to antiarrhythmic drugs (AADs).2 Within 3 months after of CA, patients often have recurrent AF due to pulmonary vein reconnection following resolution of inflammation.3 Therefore, the first three months after CA are referred to as the blanking period, also called the blind period.2 Oral antiarrhythmic medication is usually recommended during the blanking period to improve the surgical success rate and diminish AF recurrence. In China, amiodarone is the most commonly used drug for ventricular and supraventricular arrhythmias.4 However, its side effects, particularly extracardiac side effects, limit its widespread use.5 Dronedarone, which acts similarly to amiodarone, but has fewer side effects, has been used to maintain sinus rhythm after atrial fibrillation conversion.6 Dronedarone has attracted considerable attention since its emergence, and its efficacy and safety have been demonstrated in several large clinical trials including DAFNE,6 EURIDIS/ADONIS,7 ERATO8 and ATHENA.9 Currently, there are few comparative studies of dronedarone and amiodarone during the blanking period after CA. This study aimed to compare the effectiveness and safety endpoints of dronedarone and amiodarone in a real-world cohort of patients after AF ablation.
Data Sources and Methods
Study Population
Patients who underwent CA at the Arrhythmia Diagnosis and Treatment Center of Shandong University Qilu Hospital between January 2020 and December 2021 and who received oral dronedarone and amiodarone therapy after ablation were included in this retrospective study. The main inclusion criteria were as follows: 1) nonvalvular AF, 2) initial catheter radiofrequency ablation, and 3) routine postoperative follow-up. The main exclusion criteria were: 1) heart failure with New York Heart Association (NYHA) Class IV or a recent decompensation requiring hospitalization or referral to a specialized heart failure clinic; 2) age≤18 or ≥80 years; 3) blood pressure<90/60mmHg; 4) bradycardia <55 bpm or second-/third-degree atrioventricular block or sick sinus syndrome; 5) hyperthyroidism or hypothyroidism; 6) severe hepatic/renal impairment (alanine aminotransferase >120U/L or eGFR<60 mL⋅min−1⋅(1.73 m2)−1); and 7) pregnancy or breastfeeding women.
This study was approved by the Institutional Review Board of Qilu Hospital. This study was conducted in accordance with the Declaration of Helsinki, and written informed consent was obtained from all the participants. All methods were performed in accordance with the relevant guidelines and regulations. The ethical approval number was KYLL-202306-082.
Study Design
Demographic and clinical data were collected from medical records by trained clinicians who were blinded to the study aims. The types of antiarrhythmic drugs used during the blind period after CA mainly depend on the individual’s situation, doctors’ recommendations, and patients’ personal wishes. In the amiodarone group, patients were administered 200 mg every time, three times a day in the first week, twice a day in the second week, and once a day for the remaining 10 weeks. In the dronedarone group, 400 mg was prescribed twice a day after the procedure. Patient symptoms, routine electrocardiograms, and 24-hour Holter monitoring were collected by trained clinicians at one month, three months, six months and every six months after the procedure.
Catheter Ablation Strategy
Catheter ablation was aimed at pulmonary vein isolation. Left atrial thrombi were excluded by transesophageal echocardiography 1 to 2 days before ablation. If patients had thrombosis in the left atrial appendage, oral anticoagulants should be taken first to dissolve it. Heparin or low-molecular-weight heparin was used when bridging was needed. All patients received intravenous heparin to maintain an activated clotting time of 300–400 s as recommended. A single or double transseptal puncture was performed to gain entrance to the left atrium. Circumferential pulmonary vein isolation was performed with an open, irrigated-tip, radiofrequency catheter guided by an electroanatomic mapping system. A left atrial roof line was optional in patients with persistent atrial fibrillation (PAF). Pulmonary vein entrance block and conduction block across the roof line were confirmed to achieve the endpoint of procedure.
Measurement of Outcomes
The primary outcome of our study was long-term recurrence of AF. The long-term recurrence of AF was defined as any atrial tachyarrhythmias lasting 30 seconds or longer after the post-90-day blanking period. Corresponding to it, we defined the recurrence of AF within 3 months after CA as the blanking-period AF recurrence. The secondary outcomes were the blanking-period AF recurrence, rehospitalization for re-ablation, and adverse drug events (ADE), including bleeding, hepatic dysfunction or renal dysfunction, skin sensibility, gastrointestinal adverse reactions, bradyarrhythmia (<55bpm), ischemic stroke, and hyperthyroidism.
Statistical Analysis
The prevalence was calculated by dividing the total number of cases by the total number of participants. Continuous variables are expressed as mean and standard deviation (SD) in cases of normal distribution or medians (25th and 75th percentiles) in cases of non-normal distribution. Categorical variables were expressed as numbers (%). We compared the baseline characteristics of the different groups. Categorical variables were analyzed using the chi-square test. The Student’s t-test was used to compare the differences among different groups in the case of a normal distribution. In the case of a non-normal distribution, the Mann–Whitney U-test was used. Univariate and multivariate Cox regression analyses were performed to evaluate dronedarone effectiveness. In multivariate analysis, the adjusted covariates included traditional risk factors for AF recurrence. The variance inflation factor (VIF) value of CHA2DS2-VAS score was 15.165 with a tolerance of 0.066, and the VIF value of HAS-BLED score was 14.533 with a tolerance of 0.069; to avoid collinearity (VIF≥10) in the adjusted model, we did not include the HAS-BLED score as a covariate in the adjusted model. Chi-square analysis was also used to compare the incidence of ADE between the two groups. Statistical significance was set at p < 0.05.
The analyses were performed by PASS version 15, SPSS version 27.0 and R software version 4.2.3.
Subgroup Analyses
Comparisons between dronedarone and amiodarone were supplemented by subgroup analyses according to sex, age bracket, type of atrial fibrillation, BMI bracket, history of hypertension, history of coronary heart disease (CHD), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), and left atrial (LA) size. For subgroup analyses, we used multivariable Cox proportional hazard regression models.
Results
Baseline Characteristics
A total of 431 patients were included in this study. Based on the type of antiarrhythmic drug taken during the blanking period after ablation, patients were divided into amiodarone (n=202) and dronedarone (n=229) groups. The average follow-up time was 14.28 months [median 14 months, interquartile range (IQR) 10–19 months]:14.56 months (median 14 months, IQR 10–18.5 months) in the dronedarone group and 13.95 months (median 14 months, IQR 10–19 months) in the amiodarone group. Baseline patient data and concomitant medication were shown in Table 1. Patients in the amiodarone group had higher LDL-C levels and a higher proportion of smoking and drinking history than those in the dronedarone group did. The dronedarone group included more patients with paroxysmal AF. No significant differences were observed in baseline characteristics between the two treatment groups (p> 0.05). And concomitant medication had no significant difference between the two groups. 420 (97.4%) patients were treated with new oral anticoagulants (NOAC) during the blind period totally. Among them, 199 (98.5%) patients were in amiodarone group and 221 (96.5%) patients were in dronedarone group (p=0.187). The remaining patients were anticoagulated with warfarin.
 |
Table 1 Baseline Characteristics of Participants According to Group |
Primary Outcomes
In our study, the long-term AF recurrence rate was 22.04% (n=95) totally. The long-term AF recurrence rate in the dronedarone group and amiodarone group were 22.71% (n=52) and 21.29% (n=43) respectively. The long-term recurrence rate was not significantly different between groups [hazard ratio (HR),0.962; 95% confidence interval (CI),0.642–1.444; p=0.853] (Table 2 and Figure 1). There were no statistically significant differences in the long-term recurrence rate of atrial fibrillation between the groups when stratified by sex, age, type of AF, etc. (HR,1.033; 95% CI,0.661–1.614; p=0.888) (Table 2). Figure 2 shows that in the adjusted model, high HDL-C level was a protective factor for the long-term recurrence of AF. Age, sex, BMI, type of AF, LDL-C, and left atrial size did not appear to be predictors of long-term recurrence of AF (Figure 2).
 |
Table 2 The Recurrence Rate of Atrial Fibrillation in the Dronedarone Group and Amiodarone Group |
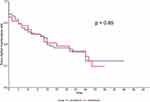 |
Figure 1 Kaplan–Meier survival curve of sinus rhythm maintenance rate by different groups. |
In subgroup analyses, the clinical benefits of dronedarone compared with those of amiodarone were consistent across the subgroups examined. (Figure 3)
Secondary Outcomes
In our study, the blanking-period AF recurrence rate was 12.30% (n=53). In dronedarone group, the blanking period recurrence rate of AF was 14.41% (n=33), while in amiodarone group, the blanking period recurrence rate of AF was 9.90% (n=20). The blanking period recurrence rate of AF in these two groups was not significantly different (HR,0.851; 95% CI,0.463–1.564; p=0.604) (Table 2 and Figure 3). The re-hospitalization rates for re-ablation in the dronedarone and amiodarone groups were 13.46% (n=7) and 4.65% (n=2), respectively (p=0.144). Figure 4 showed that the incidence of ADE increased significantly in the population treated with dronedarone (p <0.001). Adverse drug reactions occurred in 49 patients (P=11.37%), including 11 patients (P=5.45%) in the amiodarone group and 38 patients (P=16.59%) in the dronedarone group. Dronedarone was associated with a higher risk of adverse gastrointestinal reactions than amiodarone (p=0.002). Dronedarone was associated with a higher risk of skin allergies than amiodarone, with only a marginal and non-significant association (p=0.059). The incidence of other ADE did not differ significantly between the dronedarone and amiodarone groups. (Figure 4) The average QTc interval of the dronedarone group was 468.21ms, while the average QTc interval of the amiodarone group was 486.29ms (p=0.521).
 |
Figure 4 Adverse drug events occurred in dronedarone group and amiodarone group. Abbreviation: p, p-value. |
Discussion
With the emergence of various antiarrhythmic drugs, their safety and effectiveness have received widespread attention. Dronedarone is currently used to treat patients with AF. However, few studies have compared the application of dronedarone and amiodarone after CA of AF. We reported several important findings in the current study: (1) compared with amiodarone, dronedarone demonstrated similar effectiveness in preventing AF recurrence in both the long-term and blanking periods; (2) the safety of dronedarone was worse, especially in terms of gastrointestinal adverse reactions; and (3) in subgroup analyses, the benefits of dronedarone were consistent with those of amiodarone.
Dronedarone is a new antiarrhythmic drug with an amiodarone-like benzofuran structure,10 minus the iodine moieties, but with a methyl sulfonamide group.11 Dronedarone and amiodarone are largely metabolized by the hepatic cytochrome P-4503A4 isoform (CYP3A4).5,11 They are both uncoupler and inhibitor of the mitochondrial respiratory chain and of β-oxidation.10 Amiodarone has the greatest potential for preventing AF recurrence of atrial fibrillation. Some clinical trials have shown that dronedarone can reduce the recurrence of AF and CV burden of disease.6–9 Dronedarone was associated with a significant reduction in AF recurrence in the EURIDIS/ADONIS trial.12 A meta-analysis of the efficacy and safety of AADs, including dronedarone and amiodarone, has been performed.13 According to this report, dronedarone demonstrated results comparable to those of amiodarone in terms of proarrhythmic events.13 In a short-term study, dronedarone was less effective than amiodarone at decreasing AF recurrence.14 The present study suggested that dronedarone and amiodarone had almost identical effects on preventing AF recurrence of atrial fibrillation after the blanking period. Our study suggested that the effectiveness of either drug in maintaining sinus rhythm was modest. Based on the follow-up, the rehospitalization rates for re-ablation between these two groups were not significantly different. A study discussing the factors leading to recurrence of AF after CA showed that patients with AF recurrence were more likely to smoke.15 Many previous studies showed that increased alcohol consumption is associated with an increased risk of AF recurrence after CA.16–18 A multicenter prospective observational study demonstrated that alcohol reduction of ≥1% from baseline to 1-year follow-up was associated with lower risk of AF/AT recurrence, compared with alcohol reduction of <1%.18 Baseline data displayed the amiodarone group had significantly more patients with smoking and drinking habits, which might increase the recurrence rate of AF. Multivariate Cox regression analysis was used to reduce smoking and alcohol consumption on the final results. In addition, high HDL-C was found to be a protective factor for long-term recurrence of AF in our trail. Previous few studies held that HDL-C were not independently associated with AF recurrence.19,20 Some trails proved low HDL-C were associated with an increased risk of AF,21,22 but others observed no significant association of AF with HDL-C.23,24 So further discussion is needed on the relationship between HDL-C and long-term recurrence of AF.
The incidence of early AF recurrence during the 3-month blanking period following pulmonary vein isolation(PVI) ranges from 9% to 65%.25–28 Early recurrence of AF was not included in the evaluation of the eventual success rate of the procedures.29 Early recurrence is a consequence of ablation-induced proarrhythmic factors.2 Procedure-induced pathophysiological changes include necrosis, ischemia, edema, inflammation, autonomic nervous imbalance, and tissue repair including scar formation.29,30 However, delayed cure may also be the cause of the antiarrhythmic effect that develops during the blind period. The administration of AADs during the blind period has been proposed to prevent early recurrence and improve the success rate of radiofrequency ablation. Some trials demonstrated that AADs (Vaughan-Williams class I + II + III) decreased the incidence of early recurrence within the period of administration,31,32 whereas others observed that AADs (not specified) during a 2-month blanking period were ineffective.33 After initial ablation, repeat hospitalizations occur in 29%-43% at 1 year.1,34 Our study showed that amiodarone and dronedarone performed comparable in maintained the sinus rhythm during the blanking period. Distinctively, the rehospitalization rates for re-ablation were not statistically different between the two groups. Further studies are needed to clarify the effects of different AADs on the early recurrence and rehospitalization rates.
The ADE analysis suggested that amiodarone had an improved safety profile. The reduced incidence of ADE in the amiodarone group compared with the dronedarone group was mainly driven by fewer gastrointestinal adverse reactions (0.99% vs 6.99%) and skin allergies (0% vs 1.75%). Recently, real-world safety studies on dronedarone have yielded abundant results.35 In a multicenter double-blind study, treatment with dronedarone was associated with increased early mortality related to worsening of heart failure in patients with severe heart failure and left ventricular systolic dysfunction.36,37 A meta-analysis suggested that dronedarone was safer than amiodarone in terms of serious adverse events.13 Based on previous studies, GI side effects were the main reason for intolerance to dronedarone.14,38 Intolerance to amiodarone was mostly attributed to the thyroid.39 To prevent GI side effects, we recommend that patients consumed dronedarone during meals. Patients with GI side effects were administered proton pump inhibitor. However, in our study, the thyroid toxicity of amiodarone was not evident, which might be related to its short-term use. Subclinical hyperthyroidism should be monitored. In a comparative study, the incidence of stroke in the amiodarone group was significantly higher than that in the dronedarone group, and the risk of interstitial liver disease was 10 times higher than that in the dronedarone group.40 Amiodarone and its main metabolites can enhance the anticoagulant effects of warfarin and increase the risk of severe bleeding.41,42 A new study found that the combination of amiodarone and NOAC was associated with significantly higher major bleeding.43 Dronedarone does not contain iodine and does not interact with warfarin drugs.44 It is lack of strong evidence that the combination of dronedarone and NOAC can increase major bleeding events.45,46 In a post hoc analysis of the ATHENA study, dronedarone could significantly reduce the risk of stroke when compared with the placebo (HR 0.66, 95% CI 0.46–0.96).47 In this study, we found that the incidences of bleeding and stroke were not significantly different between the amiodarone and dronedarone groups. Dronedarone and amiodarone exhibit Class III effects, prolonging the QTc interval. A prolonged QTc interval is a manifestation of drug-tissue binding and is not an indication of adverse drug reactions. In a short-term, randomized, double-blind study, dronedarone caused less bradycardia and QTc interval prolongation than amiodarone.14 In this study, we found that dronedarone and amiodarone had similar effects on prolonging the QTc interval.
Subgroup analysis showed that compared with amiodarone, dronedarone was not significantly different among populations with different ages, BMI, sex, types of atrial fibrillation, left atrial volume, and history of coronary heart disease. In the current study, patients in the amiodarone group received a lower dose of amiodarone within three months. The low dose was significantly different from the conventional dose used in other studies. We inferred that amiodarone used at conventional doses would have a lower AF recurrence rate of atrial fibrillation and higher safety.
Dronedarone did not have any advantages in our experiment, but previous experiments and pharmacology have shown that dronedarone has unique advantages.5,13,39,40,48 In clinical work, many patients had better efficacy and fewer adverse events when using dronedarone. Doctors have always pursued personalized medication. In a word, the comparison of amiodarone and dronedarone requires more RCT and meta-analysis. Our research hopes to add more evidence to the use of these two drugs.
Limitations
As with all AF outcome studies, monitoring arrhythmia recurrence is subject to practical limitations. Patient symptoms and electrocardiograms may not capture all AF recurrence. Second, this study was retrospective and nonrandom, and participants without complete information or lost to follow-up were excluded; therefore, bias may exist in this study. Third, the basic condition of patients might change during the follow-up period, such as BMI, LVEF, LDL-C, etc. In addition, the short duration of this study probably led to underestimation of adverse events. Further research should include an update of this analysis using additional data. A longer timeframe may also provide sufficient outcomes to support further sub-analyses. Our data were obtained from a single center in eastern China; therefore, their generalizability to the global population is uncertain.
Conclusions
In this single-center study, dronedarone was as effective as amiodarone in preventing AF recurrence after CA, both in the long-term and blanking period. However, dronedarone had a poor safety profile, specifically with regard to gastrointestinal adverse reactions. Based on this study, we believe that dronedarone can effectively control AF recurrence after CA. The choice of antiarrhythmic drug depends on the ultimate aim of the therapy, which should be considered in the case of the patient’s clinical presentation and treatment tailored to the individual.
Ethics Approval and Informed Consent
This study was approved by the Institutional Review Board of Qilu Hospital. This study was conducted in accordance with the Declaration of Helsinki, and written informed consent was obtained from all the participants. All methods were performed in accordance with the relevant guidelines and regulations.
Acknowledgment
Yihan Li takes responsibility for all aspects of the reliability and freedom from bias of the data presented and their discussed interpretation.
Funding
This work is supported by the National Science Foundation of China 82270331 and Qingdao Key Health Discipline Development Fund QDZDZK-2022008.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Lin JL, Wu TJ, Chen CP, et al. Observational study of dronedarone in Taiwanese patients with atrial fibrillation. J Formos Med Assoc. 2020;119(1 Pt 1):59–68. doi:10.1016/j.jfma.2019.03.009
2. Calkins H, Hindricks G, Cappato R, et al. 2017 HRS/EHRA/ECAS/APHRS/SOLAECE expert consensus statement on catheter and surgical ablation of atrial fibrillation. Europace. 2018;20(1):e1–e160. doi:10.1093/europace/eux274
3. Shah S, Barakat AF, Saliba WI, et al. Recurrent Atrial Fibrillation After Initial Long-Term Ablation Success: electrophysiological Findings and Outcomes of Repeat Ablation Procedures. Circ Arrhythm Electrophysiol. 2018;11(4):e005785. doi:10.1161/CIRCEP.117.005785
4. Epstein AE, Olshansky B, Naccarelli GV, Kennedy JI, Murphy EJ, Goldschlager N. Practical Management Guide for Clinicians Who Treat Patients with Amiodarone. Am J Med. 2016;129(5):468–475. doi:10.1016/j.amjmed.2015.08.039
5. Vamos M, Hohnloser SH. Amiodarone and dronedarone: an update. Trends Cardiovasc Med. 2016;26(7):597–602. doi:10.1016/j.tcm.2016.03.014
6. Touboul P, Brugada J, Capucci A, Crijns HJ, Edvardsson N, Hohnloser SH. Dronedarone for prevention of atrial fibrillation: a dose-ranging study. Eur Heart J. 2003;24(16):1481–1487. doi:10.1016/S0195-668X(03)00321-X
7. Singh BN, Connolly SJ, Crijns HJ, et al. Dronedarone for maintenance of sinus rhythm in atrial fibrillation or flutter. N Engl J Med. 2007;357(10):987–999. doi:10.1056/NEJMoa054686
8. Davy JM, Herold M, Hoglund C, et al. Dronedarone for the control of ventricular rate in permanent atrial fibrillation: the Efficacy and safety of dRonedArone for the cOntrol of ventricular rate during atrial fibrillation (ERATO) study. Am Heart J. 2008;156(3):
9. Hohnloser SH, Crijns HJ, van Eickels M, et al. Effect of dronedarone on cardiovascular events in atrial fibrillation. N Engl J Med. 2009;360(7):668–678. doi:10.1056/NEJMoa0803778
10. Felser A, Blum K, Lindinger PW, Bouitbir J, Krähenbühl S. Mechanisms of hepatocellular toxicity associated with dronedarone--a comparison to amiodarone. Toxicol Sci. 2013;131(2):480–490. doi:10.1093/toxsci/kfs298
11. Zimetbaum PJ. Dronedarone for atrial fibrillation--an odyssey. N Engl J Med. 2009;360(18):1811–1813. doi:10.1056/NEJMp0902248
12. Page RL, Connolly SJ, Crijns HJ, et al. Rhythm- and rate-controlling effects of dronedarone in patients with atrial fibrillation (from the ATHENA trial). Am J Cardiol. 2011;107(7):1019–1022. doi:10.1016/j.amjcard.2010.11.028
13. Freemantle N, Lafuente-Lafuente C, Mitchell S, Eckert L, Reynolds M. Mixed treatment comparison of dronedarone, amiodarone, sotalol, flecainide, and propafenone, for the management of atrial fibrillation. Europace. 2011;13(3):329–345. doi:10.1093/europace/euq450
14. Le Heuzey JY, De Ferrari GM, Radzik D, Santini M, Zhu J, Davy JM. A short-term, randomized, double-blind, parallel-group study to evaluate the efficacy and safety of dronedarone versus amiodarone in patients with persistent atrial fibrillation: the DIONYSOS study. J Cardiovasc Electrophysiol. 2010;21(6):597–605. doi:10.1111/j.1540-8167.2010.01764.x
15. Buiatti A, Kaess B, Reents T, et al. Catheter Ablation for “Lone” Atrial Fibrillation: Efficacy and Predictors of Recurrence. J Cardiovasc Electrophysiol. 2016;27:536–541.
16. Grindal AW, Sparrow RT, McIntyre WF, Conen D, Healey JS, Wong JA. Alcohol Consumption and Atrial Arrhythmia Recurrence After Atrial Fibrillation Ablation: a Systematic Review and Meta-analysis. Can J Cardiol. 2023;39(3):266–273. doi:10.1016/j.cjca.2022.12.010
17. Brilliant J, Yadav R, Akhtar T, Calkins H, Trayanova N, Spragg D. Clinical and Structural Factors Affecting Ablation Outcomes in Atrial Fibrillation Patients - A Review. Curr Cardiol Rev. 2023;19(5):83–96. doi:10.2174/1573403X19666230331103153
18. Takahashi Y, Nitta J, Kobori A, et al. Alcohol Consumption Reduction and Clinical Outcomes of Catheter Ablation for Atrial Fibrillation. Circ Arrhythm Electrophysiol. 2021;14(6):e009770. doi:10.1161/CIRCEP.121.009770
19. Shang Y, Chen N, Wang Q, et al. Blood lipid levels and recurrence of atrial fibrillation after radiofrequency catheter ablation: a prospective study. J Interv Card Electrophysiol. 2020;57(2):221–231. doi:10.1007/s10840-019-00543-w
20. Li ZZ, Liu T, Huang Q, et al. Association Between Pre-Radiofrequency Catheter Ablation Serum Lipid Levels and Recurrence of Atrial Fibrillation in 412 Patients in Beijing, China: a Single-Center Study. Med Sci Monit. 2023;29:e938288. doi:10.12659/MSM.938288
21. Ding M, Wennberg A, Gigante B, Walldius G, Hammar N, Modig K. Lipid levels in midlife and risk of atrial fibrillation over 3 decades-Experience from the Swedish AMORIS cohort: a cohort study. PLoS Med. 2022;19:e1004044. doi:10.1371/journal.pmed.1004044
22. Harrison SL, Lane DA, Banach M, et al. Lipid levels, atrial fibrillation and the impact of age: results from the LIPIDOGRAM2015 study. Atherosclerosis. 2020;312:16–22. doi:10.1016/j.atherosclerosis.2020.08.026
23. Yang S, Pudasaini R, Zhi H, Wang L. The Relationship between Blood Lipids and Risk of Atrial Fibrillation: univariable and Multivariable Mendelian Randomization Analysis. Nutrients. 2021;14(1):181. doi:10.3390/nu14010181
24. Li X, Gao L, Wang Z, et al. Lipid profile and incidence of atrial fibrillation: a prospective cohort study in China. Clin Cardiol. 2018;41(3):314–320. doi:10.1002/clc.22864
25. Pieragnoli P, Paoletti Perini A, Ricciardi G, et al. Recurrences in the Blanking Period and 12-Month Success Rate by Continuous Cardiac Monitoring After Cryoablation of Paroxysmal and Non-Paroxysmal Atrial Fibrillation. J Cardiovasc Electrophysiol. 2017;28(6):625–633. doi:10.1111/jce.13190
26. Mugnai G, de Asmundis C, Hünük B, et al. Second-generation cryoballoon ablation for paroxysmal atrial fibrillation: predictive role of atrial arrhythmias occurring in the blanking period on the incidence of late recurrences. Heart Rhythm. 2016;13(4):845–851. doi:10.1016/j.hrthm.2015.12.034
27. Choi JI, Pak HN, Park JS, et al. Clinical significance of early recurrences of atrial tachycardia after atrial fibrillation ablation. J Cardiovasc Electrophysiol. 2010;21(12):1331–1337. doi:10.1111/j.1540-8167.2010.01831.x
28. Willems S, Khairy P, Andrade JG, et al. Redefining the Blanking Period After Catheter Ablation for Paroxysmal Atrial Fibrillation: insights From the ADVICE (Adenosine Following Pulmonary Vein Isolation to Target Dormant Conduction Elimination) Trial. Circ Arrhythm Electrophysiol. 2016;9(8). doi:10.1161/CIRCEP.115.003909
29. Gottlieb LA, Dekker L, Coronel R. The Blinding Period Following Ablation Therapy for Atrial Fibrillation: proarrhythmic and Antiarrhythmic Pathophysiological Mechanisms. JACC Clin Electrophysiol. 2021;7(3):416–430. doi:10.1016/j.jacep.2021.01.011
30. Vaishnav AS, Levine E, Coleman KM, et al. Early recurrence of atrial fibrillation after pulmonary vein isolation: a comparative analysis between cryogenic and contact force radiofrequency ablation. J Interv Card Electrophysiol. 2020;57(1):67–75. doi:10.1007/s10840-019-00639-3
31. Roux JF, Zado E, Callans DJ, et al. Antiarrhythmics After Ablation of Atrial Fibrillation (5A Study). Circulation. 2009;120(12):1036–1040. doi:10.1161/CIRCULATIONAHA.108.839639
32. Kaitani K, Inoue K, Kobori A, et al. Efficacy of Antiarrhythmic Drugs Short-Term Use After Catheter Ablation for Atrial Fibrillation (EAST-AF) trial. Eur Heart J. 2016;37(7):610–618. doi:10.1093/eurheartj/ehv501
33. Lodziński P, Kiliszek M, Koźluk E, et al. Does a blanking period after pulmonary vein isolation impact long-term results? Results after 55 months of follow-up. Cardiol J. 2014;21(4):384–391. doi:10.5603/CJ.a2013.0144
34. Piccini JP, Sinner MF, Greiner MA, et al. Outcomes of Medicare beneficiaries undergoing catheter ablation for atrial fibrillation. Circulation. 2012;126(18):2200–2207. doi:10.1161/CIRCULATIONAHA.112.109330
35. Valembois L, Audureau E, Takeda A, Jarzebowski W, Belmin J, Lafuente-Lafuente C. Antiarrhythmics for maintaining sinus rhythm after cardioversion of atrial fibrillation. Cochrane Database Syst Rev. 2019;9(9):CD005049. doi:10.1002/14651858.CD005049.pub5
36. Opie LH, Schwartz PJ. Dronedarone in high-risk permanent atrial fibrillation. N Engl J Med. 2012;366(12):1159.
37. Køber L, Torp-Pedersen C, McMurray JJ, et al. Increased mortality after dronedarone therapy for severe heart failure. N Engl J Med. 2008;358(25):2678–2687. doi:10.1056/NEJMoa0800456
38. Guerra F, Hohnloser SH, Kowey PR, et al. Efficacy and safety of dronedarone in patients previously treated with other antiarrhythmic agents. Clin Cardiol. 2014;37(12):717–724. doi:10.1002/clc.22342
39. Prystowsky EN. Atrial fibrillation: dronedarone and amiodarone-The safety versus efficacy debate. Nat Rev Cardiol. 2010;7(1):5–6. doi:10.1038/nrcardio.2009.221
40. Gao S, Dai W, Zhang L, Juhaeri J, Wang Y, Caubel P. Risk of Cardiovascular Events, Stroke, Congestive Heart Failure, Interstitial Lung Disease, and Acute Liver Injury: dronedarone versus Amiodarone and Other Antiarrhythmics. J Atr Fibrillation. 2013;6(4):890. doi:10.4022/jafib.890
41. Sr HD, Nandkeolyar S, Lan H, et al. Amiodarone: a Comprehensive Guide for Clinicians. Am J Cardiovasc Drugs. 2020;20(6):549–558. doi:10.1161/CIRCULATIONAHA.109.875252
42. Wells PS, Holbrook AM, Crowther NR, Hirsh J. Interactions of warfarin with drugs and food. Ann Intern Med. 1994;121(9):676–683. doi:10.7326/0003-4819-121-9-199411010-00009
43. Grymonprez M, Carnoy L, Capiau A, et al. Impact of P-glycoprotein and CYP3A4-interacting drugs on clinical outcomes in patients with atrial fibrillation using non-vitamin K antagonist oral anticoagulants: a nationwide cohort study. Eur Heart J Cardiovasc Pharmacother;2023. pvad070. doi:10.1093/ehjcvp/pvad070
44. Shirolkar SC, Fiuzat M, Becker RC. Dronedarone and vitamin K antagonists: a review of drug-drug interactions. Am Heart J. 2010;160(4):577–582. doi:10.1016/j.ahj.2010.07.008
45. Friberg L. Safety of apixaban in combination with dronedarone in patients with atrial fibrillation. Int J Cardiol. 2018;264:85–90. doi:10.1016/j.ijcard.2018.02.055
46. Mendell J, Zahir H, Matsushima N, et al. Drug-drug interaction studies of cardiovascular drugs involving P-glycoprotein, an efflux transporter, on the pharmacokinetics of edoxaban, an oral factor Xa inhibitor. Am J Cardiovasc Drugs. 2013;13(5):331–342. doi:10.1007/s40256-013-0029-0
47. Connolly SJ, Crijns HJ, Torp-Pedersen C, et al. Analysis of stroke in ATHENA: a placebo-controlled, double-blind, parallel-arm trial to assess the efficacy of dronedarone 400 mg Bid for the prevention of cardiovascular hospitalization or death from any cause in patients with atrial fibrillation/atrial flutter. Circulation. 2009;120(13):1174–1180.
48. Piccini JP, Hasselblad V, Peterson ED, Washam JB, Califf RM, Kong DF. Comparative efficacy of dronedarone and amiodarone for the maintenance of sinus rhythm in patients with atrial fibrillation. J Am Coll Cardiol. 2009;54(12):1089–1095. doi:10.1016/j.jacc.2009.04.085
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


