Back to Journals » Patient Preference and Adherence » Volume 18
Comparison of Efficacy and Adherence of Patient-Preferred (1 Unit Daily) and ADA/EASD Guideline-Recommended (2 Units Every 3 Days) Basal Insulin Titration Algorithms: Multicenter, Randomized, Clinical Study
Authors Li L, Zhang X , Zhang T, Zeng L, Lin M, Li Y, Li W
Received 27 October 2023
Accepted for publication 12 March 2024
Published 18 March 2024 Volume 2024:18 Pages 687—694
DOI https://doi.org/10.2147/PPA.S446855
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jongwha Chang
Ling Li,1 Xiaodan Zhang,1 Tong Zhang,2 Liankun Zeng,3 Mingrun Lin,4 Yanli Li,4 Wangen Li1
1Department of Endocrinology, The Second Affiliated Hospital, Guangzhou Medical University, Guangzhou, People’s Republic of China; 2Department of Endocrinology, The Third Affiliated Hospital, Southern Medical University, Guangzhou, People’s Republic of China; 3Department of Endocrinology, The Fourth Affiliated Hospital, Guangzhou Medical University, Guangzhou, People’s Republic of China; 4Department of Endocrinology, The Fifth Affiliated Hospital, Guangzhou Medical University, Guangzhou, People’s Republic of China
Correspondence: Wangen Li; Yanli Li, Email [email protected]; [email protected]
Aim: Insulin titration often faces inertia, hindering glycemic control. A patient-centered approach empowers patients to overcome this inertia. This study aims to compare the effectiveness of patient-preferred and guideline-recommended self-titration algorithms in achieving glycemic targets and improving adherence.
Methods: Outpatients with type 2 diabetes (T2D) who did not respond to oral antihyperglycemic drugs (OAD) were assessed. They were randomly assigned to patient-preferred and guideline-recommended groups. In the patient-preferred group, individuals selected an algorithm to self-adjust their insulin glargine dosage by 2 units every 3 days if the mean fasting blood glucose (FBG) over the past 3 consecutive days was ≥ 7.0 mmol/L, or by 1 unit daily if the FBG on the same day was ≥ 7.0 mmol/L. In the guideline-recommended group, insulin glargine was titrated by 2 units every 3 days if the mean FBG over the past 3 consecutive days was ≥ 7.0 mmol/L. The FBG target was set below < 7.0 mmol/L.
Results: Thirty-nine participants in the patient-preferred group and 42 in the guideline-recommended group completed the study. The cumulative rates of achieving the FBG target in the patient-preferred group compared to the guideline-recommended group were 69.2% vs 54.8% (χ²=1.792, p=0.181) in week 1, 89.7% vs 73.8% (χ²=3.403, p = 0.065) in week 2, 94.9% vs 76.2% (χ²=17.638, p=0.000) in week 3, and 100.0% vs 88.1% (χ²=4.405, p=0.036) in week 4. Adherence rates were significantly higher in the patient-preferred group (97.4%, 37/38) compared to the guideline-recommended group (66.7%, 28/42) (χ²=12.688, p=0.000). Insulin glargine dosage at FBG target achievement was 21.2± 4.3 U in the patient-preferred group and 18.8± 6.7 U in the guideline-recommended group (t=1.888, p=0.063). Hypoglycemia was reported in 1 patient in the guideline-recommended group, with no instances in the patient-preferred group.
Conclusion: The patient-preferred self-titration algorithm demonstrates a higher rate of reaching glucose targets and improved adherence.
Trial Registration Number: ChiCTR2100050805.
Keywords: type 2 diabetes, glargine, self-titration, adherence, preference
Introduction
Type 2 diabetes (T2D) is a progressive condition, necessitating insulin therapy to achieve glucose targets for many patients, despite the array of available antidiabetic treatments.1
Basal insulin, when added to metformin and other oral agents, serves as a convenient initial regimen.1 Once instituted, titration becomes pivotal for attaining desired glucose levels.2
The evolution of insulin titration can be categorized into two phases. Prior to the 1980s, physicians predominantly handled insulin titration for most patients. However, initiating insulin often required frequent contact with healthcare providers, which proved challenging due to resource constraints.3 Notably, reports such as UKPDS 33 and 34 indicated insulin dose adjustments only every three months.4,5
The 1990s ushered in the era of self-titration of insulin through self-monitoring of blood glucose (SMBG), enhancing the maintenance of glycemic control.6,7 The introduction of long-acting insulins, safer than NPH insulin, prompted numerous randomized controlled trials involving glargine and detemir, which demonstrated non-inferiority or superiority of patient-titrated insulin algorithms compared to standard care for glycemic control in T2D.8–12 The 2018 ADA Standards of Medical Care in Diabetes recommended insulin self-titration, suggesting 2–4 units once or twice weekly.13
Trials such as ATLAS, AT.LANTUS, and ATAS employed insulin self-titration algorithms entailing increments of 2 or 4 units of glargine every three days.8–10 Subsequently, starting in 2019, both ADA, EASD consensus, and AACE recommended titrating basal insulin by 2 units every three days.14,15
Interestingly, our prior survey revealed that patient-preferred insulin titration algorithms diverge from the ADA, EASD, and AACE recommended methods.16 Only 9.1% of patients favored titrating by 2 units every three days, while 90.9% preferred 1 unit daily. This discrepancy implies that the ADA and EASD endorsed self-titration approaches are incongruent with their emphasis on patient-centered care, which involves involving patients in medical decisions to overcome barriers and improve therapy adherence.17
Now that patient-preferred algorithm is different from that of ADA/EASD-recommended, a head-to-head comparison of the two algorithms is urgently needed. Our present study aims to objectively compare these divergent approaches which will provide evidence for guideline recommendation.
Methods
Participants
This multicenter, randomized, controlled prospective study adhered to the principles of the Declaration of Helsinki. Approval was granted by the institutional ethics committees of the Third Affiliated Hospital of Southern Medical University, as well as the academic ethics review boards of the Second, Fourth, and Fifth Affiliated Hospitals of Guangzhou Medical University. From January 2021 to June 2023, written informed consent was obtained from all participants before their engagement in the study.
Inclusion/Exclusion Criteria
Inclusion criteria encompassed outpatients with T2D who exhibited failure with oral antihyperglycemic drugs (OAD) (HbA1c ≥7.0% and fasting blood glucose [FBG] ≥7.0 mmol/L). The age range for inclusion was 18 to 75 years. Exclusion criteria included noncompliance with daily FBG measurement, alanine aminotransferase and aspartate aminotransferase levels exceeding three times the upper normal limit, serum creatinine levels ≥130 μmol/L, pregnancy, or utilization of medications known to disrupt glucose control.
Randomization
Utilizing SPSS V.19.0, randomization codes were generated by computer software. Patients were randomly allocated in a 1:1 ratio to either of the two algorithms across the four medical centers.
Insulin Initiation and Titration
Education concerning FBG monitoring and insulin administration was provided in accordance with the local practices of each hospital. All patients were instructed to commence insulin glargine (Lantus®; Aventis Pharma, Strasbourg, France) at an initial dose of 0.2 U/kg and to administer it consistently in the evening (between 21:00 and 22:00 h).
Patients were equipped with insulin titration algorithms. Those assigned to the guideline-recommended group self-titrated their basal insulin by 2 units every three days if the mean FBG over the preceding 3 consecutive days was ≥7.0 mmol/L. Conversely, subjects designated to the patient-preferred group were granted the option to select one of two insulin titration algorithms: first, self-titration of basal insulin by 2 units every three days if the mean FBG over the previous 3 consecutive days was ≥7.0 mmol/L; second, self-titration of basal insulin by 1 unit daily if the FBG on the same day was ≥7.0 mmol/L. The target FBG was set below <7.0 mmol/L.
Outcome
The primary outcome of this study was to assess the divergence in the rate at which both groups achieved FBG levels <7.0 mmol/L. A patient was deemed to have attained the efficacy target when their FBG levels were consistently below <7.0 mmol/L for three consecutive days. The initial day of this three-day span was logged as the date of meeting the glucose target, thereby marking the conclusion of the patient’s participation in the study.
The secondary outcome included evaluating the adherence of the two groups. Safety assessment involved scrutinizing the percentage of patients encountering hypoglycemic incidents during the study period. Hypoglycemic episodes were defined as instances characterized by hypoglycemia-related symptoms accompanied by a documented blood glucose level below <3.9 mmol/L. For severe hypoglycemia, the definition encompassed incidents in which hypoglycemia symptoms necessitated external assistance from another individual.
Statistical Analyses
Significance was ascribed to a difference exceeding one week in the time required for the two groups to reach their respective blood glucose targets. Assuming a notable difference in FBG, a significance level (α) of 0.05%, and an 80% statistical power, a total of 76 patients per group were determined to be needed, considering a 20% dropout rate. The intended recruitment was set at 100 patients overall.
Pearson’s χ²-test or Student’s t-test was employed to assess the significance of disparities between the patient-preferred and guideline-recommended groups. Findings were presented as mean ± standard deviation (SD). Statistical computations were performed using IBM Corporation’s SPSS Statistical Software 19.0. The chosen threshold for statistical significance was α=0.05.
Results
Figure 1 illustrates the study’s progression. Between January 2021 and June 2023, a total of 121 patients with OAD treatment failure were subjected to screening. Among these, 100 expressed willingness to commence and self-adjust insulin therapy, leading to their inclusion in the study. These participants were then randomly and equally allocated to either the patient-preferred or guideline-recommended groups.
 |
Figure 1 Patient disposition. Abbreviation: SMBG, self-monitoring of blood glucose. |
Of the 39 patients who successfully completed the patient-preferred regimen, 35 selected the algorithm involving daily titration of 1 unit, while the remaining 4 opted for the algorithm involving titration of 2 units every 3 days.
Baseline demographic and clinical attributes of participants were comparably distributed across the treatment groups, as detailed in Table 1.
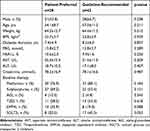 |
Table 1 Baseline Characteristics of Participants |
Difference of Rate of Reaching Glucose Target
The cumulative rates of reaching the FBG target in the patient-preferred group compared to the guideline-recommended group were as follows: in week 1, 69.2% vs 54.8% (χ²=1.792, p=0.181); in week 2, 89.7% vs 73.8% (χ²=3.403, p = 0.065); in week 3, 94.9% vs 76.2% (χ²=17.638, p=0.000); and in week 4, 100.0% vs 88.1% (χ²=4.405, p=0.036) (Figure 2).
 |
Figure 2 Accumulated rate of reaching FBG target. *p<0.05. Abbreviation: FBG, fasting blood glucose. |
The actual mean FBG of each week in the patient-preferred group compared to the guideline-recommended group were as follows: in week 1, 10.8±1.7 vs 11.1±1.9 (t=1.644, p=0.104); in week 2, 9.3±1.0 vs 9.5±0.9 (t=0.816, p = 0.417); in week 3, 7.4±0.5 vs 7.9±0.7(t=3.470, p=0.001); and in week 4, 6.6±0.3 vs 6.9±0.5 (t=2.791, p=0.007) (Figure 3).
 |
Figure 3 The actual mean FBG of each week. **p<0.01; ***p<0.001. Abbreviation: FBG, fasting blood glucose. |
Adherence
One patient in the patient-preferred group (using the titration of 2 units every 3 days) and 14 patients in the guideline-recommended group did not strictly adhere to the designated algorithm. Adherence rates were 97.4% in the patient-preferred group and 66.7% in the guideline-recommended group (χ²=12.688, p=0.000).
Insulin Dose
The mean insulin glargine dose upon reaching the FBG target was 21.2±4.3 U in the patient-preferred group and 18.8±6.7 U in the guideline-recommended group (t=1.888, p=0.063).
Safety
Hypoglycemia was reported in only 1 patient within the guideline-recommended group, while no instances of hypoglycemia were observed in the patient-preferred group.
Discussion
In the present study, patients who self-titrated using the patient-preferred algorithm achieved a significantly higher rate of reaching the FBG target compared to those following the guideline-recommended algorithm. This attributed to several reasons. First, patients using self-preferred algorithm titrated insulin dose in time. Second, guideline-recommended algorithm is a little complex and easily confused. Increasing 2 unit every 3 days needs to calculate mean FBG. Sometimes patients were not sure whether it is 2 unit every 3 days or 3 units every 2 days even it was written on the patients record. This alignment was reinforced by the robust 97.4% adherence observed in the patient-preferred group.
The method for adjusting insulin glargine involves raising the dose by 2 units every 3 days until the FBG reaches the desired level. This approach was initially suggested by Yki-Järvinen and later employed in the AT.LANTUS controlled trial.7,8 This method was also adopted in the consensus guidelines of ADA, EASD, and AACE.14,15 Subsequently, other diabetes experts’ agreements, such as those from Southeast Europe and India, also endorsed this approach.18,19
Although the authors of the AT.LANTUS trial stated that the patient-led titration method, increasing by 2 units every 3 days, is simple and had a high adherence rate over 22 weeks, and can easily be translated into clinical practice in both primary and secondary health care settings, our current findings reveal that the real-world clinical application of this method has only a 66.7% adherence rate. It is well known that randomized clinical trials have many measures ensuring patient adherence including regular visits, telephone contacts, free glucose test, and so on. Further, subject insulin dose adjustment was reviewed by the investigator at clinical visits or over the telephone. In real-world setting it is different. Our previous survey indicated that patients dislike this method due to its inconvenience. Conversely, patients favored the self-titration approach, where insulin glargine is increased by 1 unit daily, as first introduced in the INSIGHT study.20 The primary reason for patients’ preference was its simplicity.16 A straightforward titration approach offers several advantages, including fewer clinic visits for adjusting insulin doses, allowing timely dose escalation, and enabling patients to confidently manage their insulin regimen.21 This empowers patients in diabetes management and offers greater therapy flexibility.21 These benefits can potentially enhance adherence compared to more complicated methods, as complex titration methods are a major obstacle to patients’ acceptance.22,23
The guideline-recommend algorithm is not so much patient-centered as disease-centered or even physician-centered. According to the position of the ADA/EASD on patient-centered approach, physicians and patients act as partners, mutually exchanging information and deliberating on options in order to reach a consensus on the therapeutic course of action.17 The therapeutic regimen should be as simple as possible to optimize adherence.17 Importantly, engaging patients in medical decisions also enhance adherence to therapy.17 The ADA/EASD guideline-recommended algorithm may lead to poor adherence due to neglecting patient preferences.
T2D has a growing prevalence and confers significant cost burden to the health care system. Medication non-adherence places a significant cost burden on healthcare systems.24 Curtis et al reported that compared with nonadherence, adherence to glucose-lowering agents among patients with T2D was associated with a significant reduction in acute care costs and resource utilization.25 Egede et al also found that the patient-preferred algorithm may potentially help reduce the cost burden of this condition.26 Our patient-preferred algorithm had a 97.4% adherence rate and a higher rate of reaching FBG target in short term. It will helpful for reducing complication and reducing cost burden in long term.
Implementing patient-inclusion on decision-making need a little more time to explain the difference between two algorithms and let patients select their preferred one.
Our study has several limitations. First, it only involved a short-term observation focused on FBG, without considering HbA1c levels. However, it’s important to note that basal insulin adjustments should primarily be based on FBG levels.1,15,27 It’s widely recognized that FBG plays a significant role in influencing HbA1c levels. Second, there were relatively higher rate of lost to follow up in both arms (22% and 16%, respectively).
Conclusion
This study demonstrated that the patient-preferred self-titration approach, mainly increasing by 1 unit daily, exhibited better adherence, led to appropriate insulin dose adjustments, and proved to be both effective and safe in reducing FBG levels. Future guidelines should recommend patient-preferred basal insulin self-titration algorithm.
Data Sharing Statement
The raw data supporting the conclusions of this article will be made available by Wangen Li, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by the academic ethics review boards of the Second Affiliated Hospital of Guangzhou Medical University. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by Guangzhou Science and Technology Project (grants number: 202201020550 to Yanli Li).
Disclosure
The authors report no conflicts of interest in this work.
References
1. American Diabetes Association. 9. Pharmacologic approaches to glycemic treatment: standards of medical care in diabetes-2020. Diabetes Care. 2020;43:S98–S110. doi:10.2337/dc20-S009
2. Garber AJ. The importance of titrating starting insulin regimens in patients with type 2 diabetes. Diabetes Obes Metab. 2009;11(s5):10–13. doi:10.1111/j.1463-1326.2009.01138.x
3. American Diabetes Association. Standards of medical care for patients with diabetes mellitus. Diabetes Care. 1989;12(5):365–368. doi:10.2337/diacare.12.5.365
4. UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998;352:837–853.
5. UK Prospective Diabetes Study (UKPDS) Group. Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). Lancet. 1998;352(9131):854–865. doi:10.1016/S0140-6736(98)07037-8
6. Rubin RR, Peyrot M, Saudek CD. Differential effect of diabetes education on self-regulation and life-style behaviors. Diabetes Care. 1991;14:335–338. doi:10.2337/diacare.14.4.335
7. Yki-Järvinen H, Ryysy L, Nikkilä K, Tulokas T, Vanamo R, Heikkilä M. Comparison of bedtime insulin regimens in patients with type 2 diabetes mellitus. A randomized, controlled trial. Ann Intern Med. 1999;130:389–396. doi:10.7326/0003-4819-130-5-199903020-00002
8. Davies M, Lavalle-González F, Storms F, Gomis R; LANTUS Study Group. Initiation of insulin glargine therapy in type 2 diabetes subjects suboptimally controlled on oral antidiabetic agents: results from the AT.LANTUS trial. Diabetes Obes Metab. 2008;10:387–399. doi:10.1111/j.1463-1326.2008.00873.x
9. Garg SK, Admane K, Freemantle N, et al. Patient-led versus physician-led titration of insulin glargine in patients with uncontrolled type 2 diabetes: a randomized multinational ATLAS study. Endocr Pract. 2015;21:143–157. doi:10.4158/EP14079
10. Bonadonna RC, Giaccari A, Buzzetti R, Perseghin G, Cucinotta D, Avogaro A. Comparable efficacy with similarly low risk of hypoglycaemia in patient- vs physician-managed basal insulin initiation and titration in insulin-naïve type 2 diabetic subjects: the Italian Titration Approach Study. Diabetes Metab Res Rev. 2020;36:e3304. doi:10.1002/dmrr.3304
11. Russell-Jones D, Dauchy A, Delgado E, Dimitriadis G, Frandsen HA, Popescu L. Take control: a randomized trial evaluating the efficacy and safety of self- versus physician-managed titration of insulin glargine 300 U/mL in patients with uncontrolled type 2 diabetes. Diabetes Obes Metab. 2019;21:1615–1624. doi:10.1111/dom.13697
12. Meneghini L, Koenen C, Weng W, Selam J-L. The usage of a simplified self-titration dosing guideline (303 Algorithm) for insulin detemir in patients with type 2 diabetes – results of the randomized, controlled PREDICTIVE™ 303 study. Diabetes Obes Metab. 2007;9(6):902–913. doi:10.1111/j.1463-1326.2007.00804.x
13. American Diabetes Association. 8. Pharmacologic approaches to glycemic treatment. Diabetes Care. 2017;40(Supplement_1):S64–S74. doi:10.2337/dc17-S011
14. Davies MJ, D’Alessio DA, Fradkin J, et al. Management of hyperglycemia in type 2 diabetes, 2018. A Consensus Report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2018;41:2669–2701. doi:10.2337/dci18-0033
15. Garber AJ, Abrahamson MJ, Barzilay JI, et al. Consensus statement by the American Association of clinical endocrinologists and American college of endocrinology on the comprehensive type 2 diabetes management algorithm--2016 executive summary. Endocr Pract. 2016;22:84–113. doi:10.4158/EP151126.CS
16. Zhang T, Zhao Y, Du T, Zhang X, Li X, Liu R. Lack of coordination between partners: investigation of Physician-Preferred and Patient-Preferred (4P) basal insulin titration algorithms in the real world. Patient Prefer Adherence. 2018;12:1253–1259. doi:10.2147/PPA
17. Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of hyperglycemia in type 2 diabetes: a patient-centered approach: position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2012;35:1364–1379. doi:10.2337/dc12-0413
18. Hancu N, Janez A, Lalic N, et al. Expert opinion: a call for basal insulin titration in patients with type 2 diabetes in daily practice: Southeast European perspective. Diabetes Ther. 2021;12:1575–1589. doi:10.1007/s13300-021-01037-7
19. Jain SM, Seshadri K, Unnikrishnan AG, et al. Best practices and tools for titrating basal insulins: expert opinion from an Indian panel via the modified Delphi consensus method. Diabetes Ther. 2020;11:621–632. doi:10.1007/s13300-020-00770-9
20. Gerstein HC, Yale JF, Harris SB, Issa M, Stewart JA, Dempsey E. A randomized trial of adding insulin glargine vs. avoidance of insulin in people with Type 2 diabetes on either no oral glucose-lowering agents or submaximal doses of metformin and/or sulphonylureas. The Canadian INSIGHT (Implementing New Strategies with Insulin Glargine for Hyperglycaemia Treatment) Study. Diabet Med. 2006;23:736–742. doi:10.1111/j.1464-5491.2006.01881.x
21. Khunti K, Davies MJ, Kalra S. Self-titration of insulin in the management of people with type 2 diabetes: a practical solution to improve management in primary care. Diabetes Obes Metab. 2013;15:690–700. doi:10.1111/dom.12053
22. Peyrot M, Barnett AH, Meneghini LF, Schumm-Draeger PM. Insulin adherence behaviours and barriers in the multinational Global Attitudes of Patients and Physicians in Insulin Therapy study. Diabet Med. 2012;29:682–689. doi:10.1111/j.1464-5491.2012.03605.x
23. Dailey G, Aurand L, Stewart J, Ameer B, Zhou R. Comparison of three algorithms for initiation and titration of insulin glargine in insulin-naive patients with type 2 diabetes mellitus. J Diabetes. 2014;6:176–183. doi:10.1111/1753-0407.12080
24. Cutler RL, Fernandez-Llimos F, Frommer M, Benrimoj C, Garcia-Cardenas V. Economic impact of medication non-adherence by disease groups: a systematic review. BMJ Open. 2018;8(1):e016982. doi:10.1136/bmjopen-2017-016982
25. Curtis SE, Boye KS, Lage MJ, Garcia-Perez LE. Medication adherence and improved outcomes among patients with type 2 diabetes. Am J Manag Care. 2017;23:e208–e14.
26. Egede LE, Gebregziabher M, Dismuke CE, et al. Medication nonadherence in diabetes: longitudinal effects on costs and potential cost savings from improvement. Diabetes Care. 2012;35:2533–2539. doi:10.2337/dc12-0572
27. Arnolds S, Heise T, Flacke F, Sieber J. Common standards of basal insulin titration in type 2 diabetes. J Diabetes Sci Technol. 2013;7:771–788. doi:10.1177/193229681300700323
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
