Back to Journals » Clinical Ophthalmology » Volume 18
Comparison of Distance-Based Uncorrected Visual Acuity Based on the Optical Profile of Same Platform IOLs
Authors Suzuki H , Nishiyama M
Received 16 November 2023
Accepted for publication 1 March 2024
Published 6 March 2024 Volume 2024:18 Pages 671—678
DOI https://doi.org/10.2147/OPTH.S448216
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Hisaharu Suzuki,* Miho Nishiyama*
Ophthalmology, Zengyo Suzuki Eye Clinic, Fujisawa City, Kanagawa, Japan
*These authors contributed equally to this work
Correspondence: Hisaharu Suzuki, Zengyo Suzuki Eye Clinic, 1-22-11 Zengyo, Fujisawa City, Kanagawa, 251-0871, Japan, Tel +81-466-0055, Fax +81-466-0056, Email [email protected]
Purpose: To compare and evaluate uncorrected visual acuity (UCVA) from far to near distance for four different optical designs of intraocular lenses (IOLs), developed on the same IOL platform.
Patients and Methods: In a cohort of 121 patients, who underwent uncomplicated cataract surgery in Zengyo Suzuki Eye Clinic, Japan, between June 2018 and November 2023, and who received a single-piece TECNIS OptiBlue™ platform series IOL, the following four groups were established based on the IOL implant type: ZCB00V (TE), ZXR00V (SF), DFR00V (SG), and DIB00V (EH). UCVA at 5 m, 1 m, 70 cm, 50 cm, 40 cm, and 30 cm, as well as contrast sensitivity (with and without glare), was compared at one month post-operation.
Results: Regarding diffractive IOLs, patients in the SG group demonstrated significantly improved visual acuity at 5 m, 50 cm, 40 cm, and 30 cm, while those in SF group performed significantly better at 1 m. Among non-diffractive IOLs, patients in the EH group demonstrated significantly improved visual acuity scores at 1 m, 70 cm, 40 cm, and 30 cm, compared to individuals in the TE group, with comparable results between the two groups at 5 m and 50 cm. Patients in the SF and EH groups achieved similar results for visual acuity and contrast sensitivity, while those in the SG group exhibited a distinctive decrease in contrast sensitivity (with glare) relative to the other three groups.
Conclusion: DFR00V seemingly provides excellent UCVA from near to far distances, aiming for spectacle independence, although at the potential cost of decreased contrast sensitivity compared to the other three IOL types. Furthermore, although ZXR00V and DIB00V differ lens structures, they may nonetheless provide similar visual quality and spectacle independence in daily life.
Plain Language Summary: The study focused on the TECNIS platform, specifically the OptiBlue lens, which is available primarily in Japan. Uncorrected visual acuity (UCVA) from far to near distance was compared and evaluated among four optical designs of intraocular lenses (IOLs), developed on the same IOL platform.
Keywords: postoperative visual outcome, cataract surgery, contrast sensitivity, non-diffractive lenses, continuous focus
Introduction
In recent years, cataract surgery has evolved towards smaller incisions, primarily due to the introduction of phacoemulsification by Kelman, which has imparted refractive correction abilities to the overall procedure.1 Consequently, the selection of intraocular lenses (IOLs) has become a critical consideration. The IOLs can be broadly categorized into monofocal and multifocal types, and the various IOL optical designs developed over time have had a significant impact on postoperative visual outcomes and spectacle dependence. Furthermore, each IOL differs not only in optical design but also in other proprietary aspects of their overall design, making it challenging to assess differences based solely on optical design.
Therefore, in this study, we aimed to compare IOLs with different optical designs but the same platform, to evaluate the variations in visual outcomes. We focused on the TECNIS platform, specifically the OptiBlue™ lens (Johnson & Johnson Surgical Vision, Irvine, CA), which is primarily available in Japan. This platform is known to reduce glare by blocking specified purple wavelengths associated with retinal toxicity.2,3 Within this platform, we compared four different IOLs with distinct optical structures.
The ZCB00V (Johnson & Johnson Surgical Vision) is a monofocal lens introduced in 2013. The platform for this IOL consists of four key features. First, it utilizes a unique hydrophobic acrylic material that minimizes glistening, resulting in improved visual performance. Second, its front-surface aspheric design minimizes overall spherical aberration in the eye, resulting in sharp visual acuity. Third, it incorporates a ProTEC 360° sharp-edge design to reduce lens epithelial cell migration and control posterior capsule opacification. Fourth, it features a violet light-filtering tint, allowing for normal blue light transmission, which enhances low-light sensitivity, improves nighttime vision, and purportedly augments melanopsin sensitivity.3
Using the TECNIS platform, the ZXR00V (Johnson & Johnson Surgical Vision)—a multifocal IOL with extended depth of focus (EDOF)—was introduced in 2017 and the DFR00V (Johnson & Johnson Surgical Vision) was released in 2021. This IOL has a unique proprietary design that incorporates both diffractive EDOF and bifocal technology on the posterior optic to provide a far to near range of vision; this lens is referred to as continuous focus. In addition, the DIB00V (Johnson & Johnson Surgical Vision), a high-order non-aspheric monofocal IOL, was launched in 2021. By comparing uncorrected visual acuity (UCVA) and contrast sensitivity in patients who underwent cataract surgery, we investigated the postoperative visual outcomes based on the type of IOL implant received.
Materials and Methods
Patient Characteristics
The present study was a non-randomized and retrospective observational study. The study was approved by Zengyo Suzuki Eye clinic ethics committee (21,000,029) and written informed consent for data collection and participation in the study was collected from all patients.
According to the tenets of the Declaration of Helsinki and Ethical Guidelines for Medical and Biological Research Involving Human Subjects in Japan.
The study included a cohort of 121 eyes of 121 patients who underwent cataract surgery at Zengyo Suzuki Eye Clinic, Kanagawa, Japan, using the TECNIS OptiBlue platform for IOL insertion, between June 2018 and November 2023. The same surgeon (H.S.) operated on all patients using the Centurion Vision System (Alcon Vision LLC, Ft. Worth, Texas). Patients were classified into four groups, based on the IOL design received: (1) ZCB00V (TE group), (2) ZXR00V (SF group), (3) DFR00V (SG group), and (4) DIB00V (EH group). The number of eyes for each was 33, 26, 27, and 35 for TE, SF, SG, and EH, respectively. Race was Japanese. Axial length measurements were obtained using an optical biometer (OA-2000; Tomey, Nagoya, Japan), and SRK/T and Barrett Universal II formulas were used for IOL power calculation in all cases. The target refraction was emmetropia in all cases. The surgical procedure was conducted using the Centurion platform for phacoemulsification. A 2.4 mm clear corneal incision was made at the “11 o’clock” position superiorly. Continuous curvilinear capsulorhexis (CCC) was performed with a 5.5 mm diameter, ensuring complete coverage in all cases. The wound position was confirmed by postoperative slit-lamp microscopy. The CCC was approximately 5.5 mm diameter according to the ratio to the IOL.
Exclusion criteria included cases with nuclear hardness of grade 4 or higher, corneal astigmatism of –1.0D or more, and intraoperative complications such as zonular dehiscence, retinal disorders, or concomitant severe glaucoma. Corneal topography was performed by OA-2000 to exclude corneal diseases that would exceed the settings. To confirm the exclusion criteria, visual field testing (Humphrey Field Analyzer 3; ZEISS Japan) was performed if necessary after imaging diagnosis with OCT (DRI OCT Triton Pro; TOPCON Healthcare). All cases with central visual field defects were excluded.
Evaluation Methods
A postoperative period of 1 month was selected, when postoperative inflammation had settled, corneal power had stabilized due to induced astigmatism, and the IOL position was fixed, as the observation point for comparison. The position of the intraocular lens was confirmed to be in the center of the pupil by slit-lamp microscopy at 1 month postoperatively. We evaluated UCVA at 1 month post-operation using the Space-Saving Chart (Nidek, Aichi, Japan) at distances of 5 m, 1 m, 70 cm, 50 cm, 40 cm, and 30 cm. Contrast sensitivity was measured using the CSV-1000 (IKON SOLUTIONS CO., LTD, Tokyo, Japan) only in patients with preoperative visual acuity score of 0.15 or higher, as measured in logarithm of minimum angle of resolution (logMAR). Measurements for contrast sensitivity were obtained at spatial frequencies of 3c/d~18c/d under mesopic condition with glare and without glare. Based on the criteria above, the comparisons were drawn in 26, 22, 23, and 30 cases for the TE, SF, SG, and EH groups, respectively.
Statistical Analysis
Statistical analysis was performed using an unpaired Student’s t-test when comparing two groups and one-way analysis of variance (ANOVA) with post hoc tests used for comparisons of UCVA and contrast sensitivity among the four groups. After significant differences were observed in the non-repeated ANOVA test among the four groups, the Student-Newman-Keuls (SNK) test was used to test for comparisons between two groups. Differences with P-values < 0.05 were considered statistically significant. All statistical analyses were conducted using MS Excel (Microsoft Corp., Redmond, WA, USA). Data are expressed as mean ± standard deviation (SD).
Results
Table 1 shows the preoperative characteristics and postoperative SE and best corrected distance visual acuity (BCDVA). There were differences in axial length among the four groups, but no significant differences in age and average K. There were also no significant differences in postoperative SE and BCDVA among the four groups.
 |
Table 1 Preoperative Patient Characteristics and Postoperative SE and BCDVA |
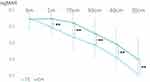
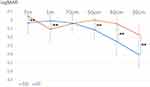
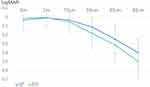
When comparing 1-month postoperative UCVA at various distances, no significant difference was observed between the TE and EH groups at 5 m. However, at 1 m, 70 cm, 50 cm, 40 cm, and 30 cm, patients in the EH group presented with significantly better UCVA (P < 0.01; Figure 1) compared with that of patients in the TE group. No significant difference was observed between the SG and SF groups at 70 cm, but at 5 m, patients in SG group exhibited significantly improved UCVA scores (P < 0.01) relative to those in SF group. The difference was even more pronounced at 50 cm, 40 cm, and 30 cm (P < 0.01). However, there was an exception at 1 m, where patients in the SF group presented with overall more improved UCVA scores in comparison to individuals in the SG group (P < 0.01; Figure 2). Both the SF and EH groups presented with highly comparable UCVA scores for all distances (Figure 3). Notably, patients in the SG group performed significantly better in the associated vision-screening tests relative to the other groups at distances between 30 cm and 5 m, except for 1 m, based on the obtained UCVA scores (Figure 4).
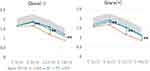
Regarding contrast sensitivity, no marked differences in performance were observed between patients in the TE vs EH, and SF vs EH group comparisons. However, patients in the SG group presented with a significant decrease in contrast sensitivity between the 6c/d and 18c/d regions, regardless of glare presence, in comparison to the other three groups (Figure 5).
Discussion
In this retrospective study, we compared the UCVA score and contrast sensitivity at various distances for four IOLs based on the same material and platform. Our results offer valuable insights regarding selection of IOL in a clinical setting, as each patient’s lifestyle and preferences vary. ZXR00V is a multifocal lens that extends depth of focus with its unique Echelette diffraction. Its structure is set higher and larger in height than the diffraction grooves used in bifocal IOLs. This reduces the energy loss of transmitted light. In addition, it corrects chromatic aberration using ChromAlignTM technology.4 This lens was shown to confer satisfactory vision at far to intermediate distances, with clinically non-inferior contrast sensitivity, compared to monofocal IOLs. DFR00V is a continuous focus multifocal IOL that combines the diffractive technology of ZLB00 and ZXR00V, thereby offering clear vision over a broad range (from far to near distances), along with color aberration correction with high contrast, similar to ZXR00V. DIB00V is a monofocal lens with a non-diffractive high-order aspheric design. Its unique optical design gradually increases power at the central portion without steps or zones, which creates a smooth depth of focus curve. Externally, it has no major structural features such as diffraction rings and is indistinguishable from a ZCB00V.
Taking these features into consideration, our data comparisons returned several key findings. Firstly, in the comparison between EH and TE groups, we observed that patients in the former group presented with significantly improved vision from 1 m to 30 cm compared to individuals in the TE group, based on UCVA scores. Similar studies comparing patients who received high-order non-spherical IOLs with those who received standard monofocal lenses, at 6 months post-cataract operation, have shown that the first group of patients exhibited significantly enhanced intermediate vision and equivalent contrast sensitivity, glare, and incidence of adverse events, relative to patients with monofocal IOLs.5,6 In our study, we also observed improvements in near vision, which could more likely be attributed to the difference in the number of cases examined (n = 68 in our work compared with n = 139 in the previous reports). Therefore, a larger cohort size needs to be considered for future studies.
Regarding the comparison between the SF and EH groups, all patients demonstrated highly similar performances for far, intermediate, and near visual acuity. The tests for contrast sensitivity also yielded comparable results between the two groups. Previous reports examining 174 cases of ZXR00V and ICB00 have highlighted that both groups maintained similar vision in far to intermediate distances, with the SF group demonstrating significantly better performance in near vision; occurrence of halos, dysphotopsia, and adverse effects were comparable between the two groups.7,8 Unlike ZXR00V, DIB00V does not use diffractive structures, which presumably results in fewer halos. However, in our study, all patients in the SF, EH, and TE groups presented with highly similar contrast sensitivity. The lack of any distinct differences may be attributed to the small number of cases examined in our work. Furthermore, previous research has reported comparable vision of patients with ZXR00V, DIB00V and standard monofocal IOLs up to intermediate distances.9 As such, the differentiation between the efficiency of ZXR00V and DIB00V in clinical practice is expected to be challenging.
Finally, in the SG and SF group comparison, patients in the SF group demonstrated significantly improved vision at 1 m, while those in the SG group achieved better performance in near vision tests. The characteristics of the continuous focus DFR00V IOL—which combines the features of a bifocal lens distributing light energy to the near field—may partially account for the observed differences between patients in the SG and SF groups. ZXR00V is known to provide continuous vision up to –1.5D without steps in logMAR, and our current observations also suggest differences in intermediate vision. Moreover, in terms of contrast sensitivity, patients in the SF group outperformed those in the SG group by a distinct margin in the high-frequency region, which indicates that the DFR00V could potentially lead to a decrease in patients’ quality of life during nighttime activities. By comparison, the continuous focus lens ensures optimal UCVA from near to far distances and aims for spectacle independence.10–12 However, it is suggested that the contrast sensitivity may decrease relative to those of the other three IOL types.
This study had some limitations, including a relatively short follow-up time and lack of information on pupil size. Pupil size may also affect depth of focus and should be considered for each IOL. Therefore, it is necessary to investigate the relationship between each IOL and factors such as pupil size in future studies with a long follow-up.
Conclusion
DFR00V is an intraocular lens that provides excellent UCVA from far to near distances and could be used to aim for spectacle independence; however, it is suggested that the contrast sensitivity may be lower with use of DFR00V than the other three types of IOLs. ZXR00V and DIB00V have different lens structures, but their need for spectacles and quality of vision in daily life remains similar. Therefore, it is important to assess the characteristics of these IOLs according to individual patient needs before making a choice. The present study offers additional insights towards a more comprehensive understanding of each IOL’s optical characteristics, to aid the selection of appropriate IOL based on each patient’s lifestyle and preferences.
Data Sharing Statement
Data from this study are restricted to this paper for reasons of privacy.
Ethics Approval and Informed Consent
This study was approved by the Ethics Committee of Zengyo Suzuki Eye Clinic (Ethics Review Committee Number: 21000029), as a retrospective observational investigation, and performed according to the tenets of the Declaration of Helsinki and Ethical Guidelines for Medical and Biological Research Involving Human Subjects in Japan. Written informed consent was obtained from all participants included in this study. This study was approved on January 26, 2022. Approval number: 0003.
Acknowledgments
We would like to thank Editage for English language editing.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
No funding was required for this study.
Disclosure
The authors have no conflicts of interest to report for this work.
References
1. Kelman CD. Phaco-emulsification and aspiration: a new technique of cataract removal. A preliminary report. Am J Ophthalmol. 2018;191:30–40. doi:10.1016/j.ajo.2018.04.014
2. Mainster MA. Violet and blue light blocking intraocular lenses: photoprotection versus photoreception. Br J Ophthalmol. 2006;90(6):784–792. doi:10.1136/bjo.2005.086553
3. Mainster MA. Intraocular lenses should block UV radiation and violet but not blue light. Arch Ophthalmol. 2005;123(4):550–555. doi:10.1001/archopht.123.4.550
4. van der Mooren M, Alarcon A, Jenkins Sanchez MD, Chang DH. Effect of Violet Light-Filtering and Manufacturing Improvements in an Extended Depth-of-Focus Intraocular Lens on Visual Performance. Clin Ophthalmol. 2023;1:701–709. doi:10.2147/OPTH.S396823
5. Auffarth GU, Gerl M, Tsai L, et al. Clinical evaluation of a new monofocal IOL with enhanced intermediate function in patients with cataract. J Cataract Refract Surg. 2021;47(2):184–191. doi:10.1097/j.jcrs.0000000000000399
6. Mencucci R, Cennamo M, Venturi D, Vignapiano R, Favuzza E. Visual outcome, optical quality, and patient satisfaction with a new monofocal IOL, enhanced for intermediate vision: preliminary results. J Cataract Refract Surg. 2020;46(3):378–387. doi:10.1097/j.jcrs.0000000000000061
7. Jeon YJ, Yoon Y, Kim TI, Koh K. Comparison between an intraocular lens with extended depth of focus (Tecnis Symfony ZXR00) and a new monofocal intraocular lens with enhanced intermediate vision (Tecnis Eyhance ICB00). Asia Pac J Ophthalmol. 2021;10(6):542–547.
8. Chang DH, Janakiraman DP, Smith PJ, et al. Visual outcomes and safety of an extended depth-of-focus intraocular lens: results of a pivotal clinical trial. J Cataract Refract Surg. 2022;48(3):288–297. doi:10.1097/j.jcrs.0000000000000747
9. Corbelli E, Iuliano L, Bandello F, Fasce F. Comparative analysis of visual outcome with 3 intraocular lenses: monofocal, enhanced monofocal, and extended depth of focus. J Cataract Refract Surg. 2022;48(1):67–74. doi:10.1097/j.jcrs.0000000000000706
10. Chang DH, Hu JG, Lehmann RP, Thompson VM, Tsai LH, Thomas EK. Clinical performance of a hybrid presbyopia-correcting intraocular lens in patients undergoing cataract surgery in a multicenter trial. J Cataract Refract Surg. 2023;49(8):840–847. doi:10.1097/j.jcrs.0000000000001205
11. Ribeiro FJ, Ferreira TB, Silva D, Matos AC, Gaspar S. Visual outcomes and patient satisfaction after implantation of a presbyopia-correcting intraocular lens that combines extended depth-of-focus and multifocal profiles. J Cataract Refract Surg. 2021;47(11):1448–1453. doi:10.1097/j.jcrs.0000000000000659
12. Gabrić N, Gabrić I, Gabrić K, Biščević A, Piñero DP, Bohač M. Clinical outcomes with a new continuous range of vision presbyopia-correcting intraocular lens. J Refract Surg. 2021;37(4):256–262. doi:10.3928/1081597X-20210209-01
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.