Back to Journals » Journal of Inflammation Research » Volume 15
Comparison of Clinical Features, Immune-Inflammatory Markers, and Outcomes Between Patients with Acute In-Hospital and Out-of-Hospital Ischemic Stroke
Authors Chen PY, Chen GC, Hsiao CL, Hsu PJ, Yang FY, Liu CY, Adam Tsou, Chang WL, Liu HH, Lin SK
Received 11 October 2021
Accepted for publication 15 January 2022
Published 9 February 2022 Volume 2022:15 Pages 881—895
DOI https://doi.org/10.2147/JIR.S342830
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ning Quan
Pei-Ya Chen,1,2 Guei-Chiuan Chen,1,2 Cheng-Lun Hsiao,1 Po-Jen Hsu,1 Fu-Yi Yang,1 Chih-Yang Liu,1 Adam Tsou,1 Wan-Ling Chang,1 Hsiu-Hsun Liu,1 Shinn-Kuang Lin1,2
1Stroke Center and Department of Neurology, Taipei Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation, New Taipei City, Taiwan; 2School of Medicine, Tzu Chi University, Hualien, Taiwan
Correspondence: Shinn-Kuang Lin, Tel +886-2-66289779 ext 3129, Fax +886-2-66289009, Email [email protected]; [email protected]
Purpose: We investigated the differences of clinical features, four immune-inflammatory markers, namely neutrophil counts, platelet-to-lymphocyte ratio, neutrophil-to-lymphocyte ratio (NLR), and systemic immune-inflammation index (SII), as well as outcomes between patients with in-hospital ischemic stroke (IHIS) and out-of-hospital ischemic stroke (OHIS).
Patients and Methods: We retrospectively enrolled 72 patients with IHIS and 3330 patients with OHIS.
Results: IHIS accounted for 2% of all patients with ischemic stroke and occurred more often in cardiology and orthopedic surgery wards. Infection, cardiac disease, and pulmonary disorder were the most common causes of hospitalization. Compared with those with OHIS, patients with IHIS had higher levels of immune-inflammatory markers, initial National Institute of Health Stroke Scale (NIHSS) scores, longer hospital stays, higher rates of heart disease, large-artery atherosclerosis or cardioembolism, received more intravenous thrombolysis (IVT) or endovascular thrombectomies (EVTs), more complications, unfavorable outcomes, and mortality. Every immune-inflammatory marker exhibited positive correlations with initial NIHSS scores and discharge modified Rankin Scale scores among patients with OHIS. NLR and SII were higher among patients with a fatal outcome in both groups. Among patients receiving IVT, most of treatment time intervals were shorter for those with IHIS than those with OHIS. Significant factors for mortality were NLR > 5.5, atrial fibrillation, and complications, with a C-statistic of 0.897 in those with IHIS; in those with OHIS, these factors were an initial NIHSS score of > 10, NLR > 6.0, atrial fibrillation, prior stroke, cancer history, and complications with a C-statistic of 0.902. The results were similar after replacing the NLR with SII.
Conclusion: Patients with IHIS had more complicated clinical features, higher levels of immune-inflammatory markers, and higher rates of mortality than patients with OHIS. The most significant predictor for mortality among those with OHIS was NIHSS score > 10, and the predictors among patients with IHIS were NLR > 5.5 and SII > 2120.
Keywords: immune-inflammatory markers, in-hospital ischemic stroke, intrahospital delay, neutrophil-to-lymphocyte ratio, out-of-hospital ischemic stroke, systemic immune-inflammation index
Introduction
In-hospital ischemic stroke (IHIS), defined as an acute ischemic stroke, occurs during hospitalization among patients originally admitted because of another diagnosis or procedure.1 IHIS accounts for 2.2% to 10.8% of all acute ischemic strokes.2 Compared with patients with out-of-hospital ischemic stroke (OHIS), patients with IHIS typically have more comorbidities and may be admitted because of active problems from those comorbidities. IHIS has been associated with more severe clinical syndromes, poorer functional outcomes, and higher rates of in-hospital mortality.3,4 Akbik et al analyzed 67,493 patients with IHIS between 2008 and 2018 and revealed that the proportion of patients with IHIS receiving reperfusion therapy increased from 9% to 19% for intravenous thrombolysis (IVT) and from 3% to 6% for endovascular thrombectomy (EVT).2 They also reported that patients with IHIS exhibited longer median times from stroke recognition to cranial imaging and from stroke recognition to IVT as compared with those with OHIS. Intrahospital delays, including poor recognition of stroke symptoms, inadequate awareness of therapeutic windows, lack of an efficient in-hospital code stroke team, insufficient interdisciplinary execution, and multiple comorbidity-related ineligibility for reperfusion therapy, hinder the timing and results of treatment for patients with IHIS.
Immune–inflammatory processes play a vital role in the development and progression of atherosclerosis. Innate and adaptive immune responses are involved in all the stages of acute stroke, namely initial artery occlusion, brain parenchymal damage, subsequent tissue repair, and infectious complications.5 Inflammation is also involved in the pathophysiology of coronary disease - the most common cause of cardiogenic death - and atrial fibrillation, the most common cardiac arrhythmia.6 The innate immunity, governed by neutrophils, monocytes, macrophages, natural killer cells, and complement systems, provides the first line of rapid defense against pathogens. Adaptive immunity, governed mainly by lymphocytes, is the second line of defense against nonself pathogens.7 Neutrophils migrate to the intraparenchymal perivascular areas within 6 to 24 hours after cerebral ischemia, producing various cytokines and participating in the early destruction of the blood–brain barrier. Lymphocytes accumulate in the brain 3–6 days after cerebral ischemia, and serve as a regulatory and neuroprotective function.8 Adaptive immunity also exerts an immunosuppressive effect that promotes intercurrent infections.5 Platelets participate in immune-inflammatory responses by releasing mediators to boost inflammation after stroke, which results in the release of neutrophils and lymphocytes into the vessel wall.9 Several immune-inflammatory markers, such as the neutrophil counts (NC), platelet-to-lymphocyte ratio (PLR), neutrophil-to-lymphocyte ratio (NLR), and systemic immune-inflammation index (SII), have been reported to be associated with poor outcomes among patients with acute stroke, cardiovascular disease, and various types of cancer.7,10–14 However, alterations in immune-inflammatory markers have rarely been described in patients with IHIS. In this study, we investigated the differences of clinical features, four immune-inflammatory markers (NC, PLR, NLR, and SII), and the outcomes between patients with IHIS and those with OHIS.
Materials and Methods
Study Population and Data Collection
For continuous quality control of stroke care, we prospective registered patients who were admitted to the ward for stroke. We retrospectively reviewed the records of all registered inpatients who presented with acute ischemic stroke during the period from January 2011 to April 2021. The diagnosis of acute ischemic stroke was confirmed by clinical presentation and proof of either an ischemic lesion or absence of a corresponding intracranial lesion other than infarction by using brain computed tomography (CT) or magnetic resonance imaging. Patients were divided into two groups: including patients with IHIS and those with OHIS. IHIS was defined as a stroke occurring during the period of hospitalization or at the emergency department (ED). OHIS was defined as a stroke that occurred before patients arrived at the ED. The following information was collected: age, sex, and clinical features, including initial presentation, initial National Institutes of Health Stroke Scale (NIHSS) score, risk factors of stroke, and length of stay (LOS) in hospital. Laboratory data including a full blood count with white blood cell differentials and platelet, glucose, and creatinine levels were obtained on arrival at the ED for patients with OHIS or during acute attack of stroke at the ward for patients with IHIS. Fasting lipid profiles including cholesterol, LDL-cholesterol and triglyceride were obtained within 24 hours of admission (for patients with OHIS) or stroke symptom onset (for patients with IHIS). Four immune-inflammatory markers, namely NC, PLR, NLR, and SII were obtained for analysis. The PLR was calculated as the ratio of platelet-to-lymphocyte count and the NLR was calculated as the ratio of NC to lymphocyte count. The SII was calculated as the platelet count multiplied by the NLR. Fasting cholesterol and triglyceride levels were recorded the morning after admission to the ward (for patients with OHIS) or during hospitalization (for patients with IHIS).
We also collected the structural time intervals related to the diagnosis and treatment of acute stroke, namely onset-to-first-aid time (first aid was performed by the emergency physician for patients with OHIS and the physician in charge for patients with IHIS), onset-to-CT time, onset-to-CT angiography (CTA; onset-to-CTA) time, onset-to-neurology liaison time (onset-to-liaison time), liaison-to-neurological evaluation (NE; liaison-to-NE) time, onset-to-NE time, onset-to-IVT time (time from symptom onset to the loading bolus in IVT), and onset-to-EVT time (time from symptom onset to the groin puncture in EVT). Liaison-to-IVT and liaison-to-EVT times were also collected for patients received IVT or EVT treatment.
Statement of Ethics
The study was conducted in accordance with the Declaration of Helsinki. Ethical approval for this study was provided by the Institutional Review Board of Taipei Tzu Chi Hospital, New Taipei City (approval no. 10-XD-128). Informed written consent was waived because this study involved retrospective data analysis. All data collected and analyzed were derived from clinical records without any intervention or influence on clinical treatment. To fully protect patient privacy and rights, only clinical observation data were used for publication, and personal information was disclosed to any other third party without the patient’s consent.
Stroke Severity, Classification, and Clinical Features
Initial stroke severity was assessed when patients with OHIS presented to the ED or for patients with IHIS after symptom onset by a neurologist according to the NIHSS. We classified the etiology of ischemic stroke according to the Trial of ORG 10172 in Acute Stroke Treatment (TOAST) categories, namely large-artery atherosclerosis, small-vessel occlusion, cardioembolism, other determined etiology, and undetermined etiology.15 Urinary tract infection, pneumonia, gastrointestinal bleeding, and seizure were registered as stroke complications. Functional outcomes were evaluated using the NIHSS and modified Rankin Scale (mRS) at discharge. An mRS score of >2 was considered to indicate an unfavorable outcome.
Neurological Liaisons and Acute Stroke Treatment
During the study period, the criteria of IVT and EVT were modified annually according to novel global evidence and revised guidelines by the Taiwan Stroke Society; however, the treatment of acute ischemic stroke was identical for patients with IHIS and those with OHIS during this period. In the neurological department, the responsibility of a 24-hour neurological liaison service is assigned to 8 to 10 consultant neurologists on a regular schedule. Among patients with IHIS, regular or emergent neurological liaisons are requested by physicians from the corresponding department in case a stroke is suspected during hospitalization. The time from consultation to a patient visit by a neurologist (liaison-to-NE time) for an emergent consultation (together with an emergent phone call directly to the on-duty neurologist) is recommended to be ≦2 hours (120 minutes), and is recommended to be ≦24 hours (1440 minutes) for a regular consultation. A well-organized code stroke protocol for IVT and EVT therapies has been implemented in the index hospital for patients with OHIS. The same protocol, except for an absence of emergent stroke call among the first-line responders and a check list of time intervals for conducting IVT or EVT, has been applied to patients with IHIS. Neurologists arrive at the ED immediately after the emergency physician activates a code stroke, which typically occurs before available brain CT imaging, when a patient is eligible for evaluation for IVT or EVT. For emergency consultations other than activation of a code stroke from the ED, neurologists still need to arrive at the ED within 30 min of a consultation.
Statistical Analysis
Continuous variables are presented as the median (first to third quartile). The chi-square test or Fisher’s exact test were used for categorical comparisons. Group comparisons of continuous variables were performed using the Mann-Whitney U-test. Correlations of continuous variables of immune-inflammatory markers with initial NIHSS and discharge mRS scores were analyzed using Pearson correlation coefficient and linear regression tests. Continuous variables of age, NIHSS score, and immune-inflammatory markers were converted into dichotomous variables with the optimal cutoff value determined according to the Youden index through a receiver operating characteristic (ROC) curve for prediction of mortality. The variables were subsequently added to a multiple or stepwise logistic regression model to identify the significant factors associated with a fatal outcome. Additionally, we analyzed the predictive performance of the significant variables through the C-statistic for fatal outcome in patients with IHIS and those with OHIS. A P value of <0.05 was considered to indicate a significant result. All statistical analyses were performed using SPSS (version 24; SPSS Inc, Chicago, IL, USA). The scatter plots diagrams were constructed and the ROC curves were compared using MedCalc version 18 (MedCalc Software, Mariakerke, Belgium).
Results
During the study period, 72 patients with IHIS and 3330 patients with OHIS were enrolled. IHIS accounted for 2% of all patients with acute ischemic stroke. The distribution of disease characteristics of 72 patients with IHIS is summarized in Table 1. The median age of onset was 75.3 years, and the median day of stroke onset was on day three of hospitalization. Thirteen patients (18.1%) had an unclear symptom onset time, and 56 patients (77.8%) had a stroke located in the anterior circulation of brain. Unclear symptom onset times were observed more often among patients with posterior circulation stroke (6/16 = 37.5%) than those with anterior circulation stroke (7/56 = 12.5%) (P = 0.032). More than two-thirds (68%) of patients were admitted to the internal medical ward. Cardiology and orthopedic surgery were the two wards where the most instances of IHIS occurred. Procedure-related stroke (defined as a stroke occurring on the same day after invasive procedures, such as surgery or cardiac catheterization) was observed in 11 patients (15.3%). The four most common primary causes of hospitalization were infection, coronary or cardiac disease, pulmonary disorder, and bone disorder. Large-artery atherosclerosis and cardioembolism constituted 78% of stroke etiology classified by TOAST criteria.
 |
Table 1 Distribution of Disease Characteristics of 72 Patients with in-Hospital Ischemic Stroke |
We compared the clinical features and outcomes between patients with IHIS and those with OHIS (Table 2). Compared with the OHIS group, the IHIS group had a greater proportion of women, a higher rate of heart disease, and a lower rate of smoking. All four immune-inflammatory markers, namely NC, PLR, NLR, and SII, were higher among patients with IHIS than among those with OHIS. The rate of IVT therapy was higher among patients with IHIS (11%) than among patients with OHIS (6%), but it did not reach statistical significance. The rate of EVT therapy (6%) was significantly higher among patients with IHIS than that among patients with OHIS (2%). The overall rate of all patients who received IVT or EVT was higher among patients with IHIS (12/72 = 17%) than among those with OHIS (224/3330 = 7%; P = 0.004). All the treatments of IVT and EVT in patients with IHIS were conducted among patients with anterior circulation stroke. Compared with patients with OHIS, those with IHIS were classified more often as having large-artery atherosclerosis or cardioembolism, had more complications during hospitalization, longer hospital LOSs, higher initial and discharge NIHSS scores, and higher discharge mRS score (P <0.001). Unfavorable outcomes (89%) and mortality (17%) occurred more often among patients with IHIS than among patients with OHIS (51% and 5%, respectively). Complications occurred in 481 of all 3402 patients (14%). Patients with complications had much higher median initial NIHSS scores (16 [8–13]) than those without complications (4 [2–8]; P <0.001).
 |
Table 2 Comparison of Clinical Features Between Patients with IHIS and OHIS |
Given the majority of patients with IHIS had unfavorable outcomes, no differences of immune-inflammatory markers were observed between patients with IHIS with favorable and unfavorable outcomes (Table 3). However, patients with unfavorable outcome had significantly higher immune-inflammatory markers than those with favorable outcomes among patients who had OHIS. Additionally, results of both Pearson correlation coefficient (Figure 1) and linear regression analyses (Table 4) revealed that all four immune-inflammatory markers exhibited positive correlations with initial NIHSS scores and discharge mRS scores among patients with OHIS. Multiple linear regression analyses of immune-inflammatory markers with initial stroke severity (initial NIHSS score) and comorbidities (hypertension, diabetes mellitus, atrial fibrillation, dyslipidemia, prior stroke, and cancer history) after converting dichotomous variables to continuous variables adjusted by age and sex revealed that initial NIHSS score exhibited the most significant positive correlation with all four immune-inflammatory markers (P < 0.001). A cancer history exhibited the second significant correlation with NLR (coefficient = 0.063; P < 0.001) and SII (coefficient = 0.042; P = 0.018).
 |
Table 3 Correlation of Immune-Inflammatory Markers with Unfavorable Outcomes in Patients with IHIS and OHIS |
 |
Table 4 Linear Correlation of Immune-Inflammatory Markers with Initial Stroke Severity and Short-Term Outcome |
A clear onset time of stroke was noted in 82% of patients with IHIS and only 49% of patients with OHIS (P <0.001). The structural time intervals and treatments between 59 patients with IHIS and 1619 patients with OHIS who had a clear onset time are compared in Table 5. The median onset-to-first-aid time (by the emergency physicians) was 273 min among patients with OHIS. Among those with IHIS, first aid was generally provided by nurses or physician in charge of the corresponding department who detected the stroke symptoms. However, confirming the onset-to-first-aid time is difficult because of the absence of a formal registration system. Compared with those with OHIS, patients with IHIS exhibited a shorter onset-to-CT time. No difference of onset-to-CTA time was observed between these two groups. The rate of onset-to-CT time within 6 hours was higher among those with IHIS (42/59 = 71%) than among patients with OHIS (902/1619 = 56%; P = 0.023). To provide early identification of patients eligible for IVT or EVT therapy, we compared the efficiency of the neurological liaisons among 944 patients with onset-to-CT times within 6 hours (comprising 42 patients with IHIS and 902 patients with OHIS). No differences of treatment rates for IVT and EVT were noted between those with IHIS and those with OHIS. No differences of median onset-to-liaison and onset-to-NE times were observed. However, the median liaison-to-NE time was much shorter in OHIS (P <0.001). A total of eight patients with IHIS received IVT treatment; three of them had cardiac catheterization-related stroke in the cardiology ward, two had urinary tract stones in the urology ward, two had nonspecific symptoms during an observation period at the ED, and one had asthma at the pulmonology ward. Four patients with IHIS received EVT treatment: two patients at the cardiology ward (because of heart failure in one and atrial fibrillation in the other), one patient at the oral surgery ward (after oral surgery), and one patient at the nephrology ward (because of urinary tract infection). A further subgroup analysis of time intervals among 236 patients receiving IVT or EVT treatment revealed that patients with IHIS had shorter median onset-to-CT, onset-to-liaison, onset-to-NE, and onset-to-IVT times, and patients with OHIS had shorter median liaison-to-NE and liaison-to-EVT times. The median liaison-to-NE time among patients with OHIS was only 4 min, which was related to an activation of code stroke at the ED. No difference of median onset-to-EVT time was observed between the two groups. Eighteen patients eligible for thrombolytic therapy did not receive IVT treatment. Reasons hindering IVT treatment included recent major surgery in 8 patients, acute critical illness in 8 patients, and active gastrointestinal bleeding in 2 patients. Twenty patients eligible for thrombectomy therapy did not receive EVT treatment. Reasons hindering EVT treatment were: not available EVT treatment in 11, intrahospital time delay in 3, and acute critical illness in 6. Those 14 patients without acute critical illness might have the opportunity to receive thrombectomy therapy if EVT treatment were available during the whole study period in case that timely CTA disclosed large artery occlusion.
 |
Table 5 Comparison of Time Intervals and Treatment Between Patients with IHIS and OHIS Who Had Clear Onset Time |
The univariate analyses of clinical features and fatal outcomes among patients with IHIS and OHIS are displayed in Table 6. Patients who had IHIS with fatal outcomes were older and had higher levels of NLR and SII, higher rates of heart disease, atrial fibrillation, and complications, but lower level of LDL-cholesterol than survivors did. Patients who had OHIS with fatal outcome were older, and had higher initial NIHSS scores, higher NC, NLR, SII, glucose, creatinine levels, higher rates of heart disease, atrial fibrillation, dyslipidemia, cancer history, uremia, complications, and IVT or EVT therapy, but lower levels of hemoglobin, LDL-cholesterol, and triglyceride than those who survived. Of the four immune-inflammatory markers, NLR and SII differed most significantly and were thus selected for further multivariable analysis. Given both heart disease and atrial fibrillation represent cardiac disorder, and differences in atrial fibrillation were more significant among both patients groups, we selected atrial fibrillation for further multivariable analysis. Through ROC curve analysis with Youden index, we identified the optimal cutoff points for age, NLR, SII, and NIHSS scores to predict mortality. The cutoff values were ≧78 years and ≧80 years of age, an NLR of >5.5 and >6.0, and an SII >2120 and >1051 for those with IHIS and OHIS, respectively. The cutoff value of NIHSS scores for mortality was >10 among patients with OHIS. Variables with a P value of <0.1 in Table 6 were included in further multivariable analysis. The results of stepwise logistic regression analysis among patients with IHIS and multiple logistic regression analysis among patients with OHIS for mortality are presented in Table 7. An NLR of >5.5, atrial fibrillation, and complications were significant predictors of mortality among patients with IHIS. The C-statistic of these three significant factors (Model 1) for prediction of mortality was 0.897 (0.804–0.989; Figure 2A). When the NLR of >5.5 was replaced by the SII of >2120, an age of ≧78 years became an additional significant factor, and the C-statistic of these four factors for prediction of mortality was 0.926 (0.838–0.975; Figure 2B). However, no significant difference was noted between the results of the C-statistic comprising either an NLR of >5.5 or an SII of >2120 (P = 0.606). The area under the curve (AUC) and sensitivity/specificity for prediction of mortality when using NLR >5.5 was 0.777 (91.7%/63.8%), and that when using SII >2120 was 0.707 (50.0%/91.4%), respectively. Among patients with OHIS, an initial NIHSS score of >10, complications, an NLR >6.0, atrial fibrillation, and cancer history were significant positive predictors, and prior stroke was a negative predictor of mortality. Together (Model 2), these factors resulted in a predictive probability for mortality of 0.903 (0.885–0.922) according to the C-statistic (Figure 2C). When replacing NLR >6.0 with SII >1051, male sex became an additional significant factor and the C-statistic of these seven factors for prediction of mortality was 0.902 (0.885–0.920; Figure 2D), which was almost the same as the model comprising an NLR >6.0 (P = 0.769). The AUC of NIHSS >10 for prediction of mortality was 0.829 with a sensitivity of 86.6% and a specificity of 79.2%.
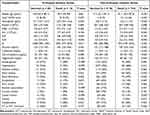 |
Table 6 Univariate Analyses of Clinical Features and Fatal Outcome in Patients with In-Hospital Ischemic Stroke and Out-of-Hospital Ischemic Stroke |
 |
Table 7 Multivariable Analyses and C-Statistic of Clinical Features and Fatal Outcome Among Patients with in-Hospital Ischemic Stroke and Out-of-Hospital Ischemic Stroke |
Discussion
IHIS accounted for approximately 2% of all ischemic strokes in the present study. Cardiology was the most frequent department where IHIS occurred, which is consistent with previous reports.16,17 Patients admitted to the cardiology ward are at greater risk of developing acute ischemic stroke because cardiovascular disorders, including coronary artery disease, dysrhythmias, and valvular heart disease, are common causes of ischemic stroke. Coronary artery disease and cerebrovascular disease have risk factors similar to those of atherosclerosis, such as aging, hypertension, diabetes mellitus, and dyslipidemia. Atrial fibrillation, however, is the most common cause of cardioembolism according to the TOAST classification, because of the potential embolic source from the heart and the effect of reduced cerebral hemodynamics from impaired cardiac function.18 Patients admitted to the orthopedic surgery ward with bone fractures are likewise at risk of developing ischemic stroke. Bone fracture and ischemic stroke also have many common risk factors,19 and stroke and bone fracture are both risk factors and complications of each other. The risk of stroke doubles after a hip fracture and remains elevated for up to 10 years.20 Limb weakness from a stroke might not be perceived because of the pain caused by the bone fracture if the paresis occurs on the fractured limb with constrained movements.21 Procedure-related or perioperative stroke was observed in approximately 15% of patients with IHIS in the present study, but it was reported in up to 60% of patients in Kassardjian’s study.16 Patients with IHIS with a stroke in the posterior circulation of the brain had higher rates of unclear onset times. General weakness of limbs and reduced mental status caused by acute illness or infection may mask the stroke symptoms, particularly among those with posterior circulation without the typical symptoms noted in the Cincinnati Prehospital Stroke Scale (arm weakness, speech disturbance, or facial droop).22
All four immune-inflammatory markers were positively and linearly correlated with patients’ initial NIHSS and the discharge mRS scores and were higher among patients with OHIS with unfavorable outcomes. Patients with IHIS had considerably higher levels of all four immune-inflammatory markers than patients with OHIS had. Such higher levels of immune-inflammatory markers resulted from the primary disorder, such as coronary artery disease, infectious disease, bone fracture, or other metabolic problem, during admission, superimposed by a subsequent ischemic stroke during hospitalization. Infectious disease, coronary or cardiac disease, pulmonary disorder, and bone fracture were four most common primary disorders for hospitalization in the present study. Lu et al determined that cardiovascular and oncological diseases were the most frequently reported reasons for admission among patients with IHIS.17 Thus, a strong association exists between increased immune-inflammation response and infectious disease. Both cardiovascular and oncological diseases have been associated with excessive activation of the immune-inflammation system with higher levels of immune-inflammatory markers.23,24 Moreover, the immune system plays a central role in developing not only in chronic airway diseases but also various interstitial lung diseases and the growth of pulmonary neoplasms.25 Vester et al reported that poor regulation of the immune system after bone trauma in older patients was likely associated with the increased complication rate and susceptibility to infections.26
Reports have demonstrated that the immune-inflammatory markers increase linearly with the initial NIHSS and the discharge mRS scores.7,14 We obtained the same results among patients with OHIS. Large-artery atherosclerosis and cardioembolism, which usually cause higher stroke severity with higher NIHSS scores, account for more than three-quarters of IHIS cases. Furthermore, patients with greater disease severity and multiple comorbidities typically have many complications. Pneumonia and urinary tract infection are the two most common in-hospital complications. Such infections further increase the immune-inflammatory response, leading greater disease severity. Additionally, stroke-induced immunosuppression related to excessively activated adaptive immunity in large-artery atherosclerosis or cardioembolic strokes also increases the patient’s susceptibility to post-stroke infections.5,27,28 This vicious cycle leads to a poor clinical outcome. A large prospective study conducted by Smeeth et al indicated that risk of stroke increases in the days following an acute upper respiratory or urinary tract infection.29 Sebastian et al analyzed 152,356 acute ischemic strokes cases and determined that every infection type was associated with an increased likelihood of acute ischemic stroke, and the strongest association was for urinary tract infection within the 7-day window.30 A comprehensive review by Elkind et al suggested that after certain severe acute infections, such as influenza or sepsis (or possibly COVID-19), the risk of stroke increases transiently (a cerebrovascular vulnerable window), and stroke may occur.31
In the present study, nearly 90% of patients with IHIS had an unfavorable outcome. Patients with IHIS had higher degree of stroke severity and more complications during hospitalization. This result could explain why no difference in immune-inflammatory markers were noted between favorable and unfavorable outcomes among patients with IHIS. However, higher levels of immune-inflammatory markers were observed among patients with fatal outcomes than among those without fatal outcomes in patients with IHIS and OHIS. Both Model 1 (C-statistic = 0.897) for IHIS and Model 2 (C-statistic = 0.903) for OHIS provide excellent predictions for mortality. Common significant predictors of mortality in both groups of patients were atrial fibrillation, complications, and higher level of NLR or SII. The initial NIHSS score, a major predictor of unfavorable outcome and mortality among patients with OHIS, was nonsignificant among those with IHIS, possibly because of the small number of patients and a large proportion of patients with IHIS having higher initial NIHSS scores than those with OHIS. In such situations, an NLR of >5.5 or an SII of >2102 became the most dominant predictor among the significant factors of mortality. Among patients with OHIS, an NIHSS score of >10 was the optimal predictor of mortality. Although all four immune-inflammatory markers had similar correlations with the clinical features and outcomes during univariate analyses, the NLR and SII were equally superior independent predictors of mortality compared with the other two markers.
Among patients with OHIS, the treatment time can be separated into a prehospital delay (onset-to-ED time) and an intrahospital delay (ED-to-CT time; ED-to-IVT time, and ED-to-EVT time) because of the precise registration time during the patient’s arrival at the ED. For patients with IHIS, the onset-to-CT time is a crucial interval for the primary diagnosis of stroke. Most studies have demonstrated a longer onset-to-CT time in patients with IHIS, particularly during the early era of thrombolytic therapy.32 Recent studies by Lu et al and Caparros et al have revealed that time intervals regarding intrahospital delay were shorter among patients with IHIS than among those with OHIS receiving IVT or EVT therapy.17,33 The present study also reveals shorter time intervals among patients with IHIS. A clear onset time was noted for approximately four in five patients with IHIS and half of patients with OHIS. This might suggest that IHIS patients had a greater likelihood of receiving IVT or EVT treatment than did patients with OHIS. Although the rates of patients who received IVT or EVT were similar among patients with an onset-to-CT time ≦6 hours between those with IHIS and those with OHIS (29% vs.25%), patients with IHIS received IVT or EVT treatment at a higher rate (17% vs 7%) than other patients in the study. These results could be attributed to a higher rate of patients with IHIS having an onset-to-CT time ≤6 hours and having shorter median onset-to-CT and onset-to-IVT times. Besides, the number of IHIS could be underestimated because not all patients with IHIS, particular for patients with minor stroke symptoms, were transferred to the stroke unit. Neurological evaluations confirming a diagnosis of stroke is the most vital step in early treatment. The median onset-to-liaison time and onset-to-NE time were shorter among patients with IHIS patients receiving IVT or EVT treatment than among patients with OHIS. The rapid arrival of neurologists to the ED for patients with OHIS or to the bedside of patients with IHIS after an emergent neurological liaison helps improve the execution rate of thrombolytic therapy. A prolonged onset-to-liaison time among patients with OHIS is most often due to a delay in the onset-to-ED time; among patients with IHIS, however, a prolonged time is mostly caused by a delayed neurological liaison from the physicians in charge, who may not have been exactly aware of the therapeutic windows or the severity of a stroke, particularly when symptoms develop outside of the working time.
An interdisciplinary team that follows appropriate specialized protocol for patients with IHIS, including a special contact window for emergent liaison, rapid transportation of patients for cranial imaging study, and a clear pathway for medicine delivery to the bed side, has been reported to effectively shorten the intrahospital delay.16,34 Furthermore, widespread educational programs for all hospital staff to more effectively recognize stroke symptoms, rapidly convey the bedside information from caregivers to physicians in charge, and understand the concept of therapeutic time windows, are vital for increasing the reperfusion rate for eligible patients. Stroke incidence is lower in the ward than in the ED. Frequent educational programs are required to ensure effective stroke treatment, particularly in units in which stroke occurs most frequently, namely the cardiovascular, infectious and orthopedic surgery wards.
This study has several limitations. First, the number of patients with IHIS was too small and was underestimated. The number of fatal outcome in IHIS was only 12 and the results of multivariable analyses of fatal outcome among patients with IHIS might not be stable. Small sample size might cause a wide range of confidence intervals but does not mean that the results are not correct. Given a sparse effect may cause a wide range of confidence intervals under a certain level, probability of monotone likelihood is a further limitation.35 Patients with a minor IHIS might not be transferred to the neurological ward after liaison, and were thus not recorded in the stroke registry. Patients with severe illness due to the primary disease who were admitted to the intensive care unit and experienced a nonfatal stroke were also not transferred and registered because of unstable vital signs and complicated comorbidities. Therefore, the rates of IVT and EVT among patients with IHIS may have been overestimated. Second, 18% of patients with IHIS patients and 51% of patients with OHIS patients had unclear symptom onset times, which might have led to a biased statistical analysis. However, based on experience, a clear symptom onset time is generally difficult to confirm. Third, the inclusion criteria of IVT therapy were updated annually, and the 24-hours EVT therapy had been implemented for less than 2 years in the index hospital. The number of patients receiving EVT treatment, however, remained insufficient. Nevertheless, we applied the same criteria of IVT and EVT for patients with IHIS and OHIS, and the number of patients receiving EVT treatment is currently increasing. Finally, our data were limited to the discharge outcome. We could not determine an intermediate outcome at 3 month nor conduct a long-term follow-up.
Conclusion
Cardiology and orthopedic surgery were the two most common departments where IHIS occurred. Compared with patients with OHIS, patients with IHIS had higher levels of all immune-inflammatory markers as well as higher rates of large-artery atherosclerosis or cardioembolism, receiving IVT or EVT treatment, unfavorable outcome and mortality. All time intervals were shorter among patients with IHIS receiving reperfusion therapy, except for liaison-to-NE time. The most significant predictor for mortality among those with OHIS was NIHSS score >10. An NLR >5.5 or a SII >2102 was the most significant predictor of mortality among patients with IHIS. Physicians need to be more vigilant toward these high levels of immune-inflammatory markers with careful clinical evaluation and management. Further protocols for IHIS are warranted to improve the quality of care for patients with IHIS.
Acknowledgments
This study was funded by Taipei Tzu Chi Hospital (TCRD-TPE-109-RT-7). The founder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Cumbler E. In-hospital ischemic stroke. Neurohospitalist. 2015;5(3):173–181. doi:10.1177/1941874415588319
2. Akbik F, Xu H, Xian Y, et al. Trends in reperfusion therapy for in-hospital ischemic stroke in the endovascular therapy era. JAMA Neurol. 2020;77(12):1486–1495. doi:10.1001/jamaneurol.2020.3362
3. Moradiya Y, Levine SR. Comparison of short-term outcomes of thrombolysis for in-hospital stroke and out-of-hospital stroke in United States. Stroke. 2013;44(7):1903–1908. doi:10.1161/STROKEAHA.113.000945
4. Bekelis K, Missios S, Coy S, MacKenzie TA. Comparison of outcomes of patients with inpatient or outpatient onset ischemic stroke. J Neurointerv Surg. 2016;8(12):1221–1225. doi:10.1136/neurintsurg-2015-012145
5. Iadecola C, Anrather J. The immunology of stroke: from mechanisms to translation. Nat Med. 2011;17(7):796–808. doi:10.1038/nm.2399
6. Fernández-Ruiz I. Immune system and cardiovascular disease. Nat Rev Cardiol. 2016;13:503. doi:10.1038/nrcardio.2016.127
7. Chu YW, Chen PY, Lin SK. Correlation between immune-inflammatory markers and clinical features in patients with acute ischemic stroke. Acta Neurol Taiwan. 2020;29(4):103–113.
8. Clark RK, Lee EV, White RF, Jonak ZL, Feuerstein GZ, Barone FC. Reperfusion following focal stroke hastens inflammation and resolution of ischemic injured tissue. Brain Res Bull. 1994;35:387–392. doi:10.1016/0361-9230(94)90119-8
9. Ali RA, Wuescher LM, Worth RG. Platelets: essential components of the immune system. Curr Trends Immunol. 2015;16:65–78.
10. Bhat T, Teli S, Rijal J, et al. Neutrophil to lymphocyte ratio and cardiovascular diseases: a review. Expert Rev Cardiovasc Ther. 2013;11(1):55–59. doi:10.1586/erc.12.159
11. Fang YN, Tong MS, Sung PH, et al. Higher neutrophil counts and neutrophil-to-lymphocyte ratio predict prognostic outcomes in patients after non-atrial fibrillation-caused ischemic stroke. Biomed J. 2017;40:154–162. doi:10.1016/j.bj.2017.03.002
12. Lim HH, Jeong IH, An GD, et al. Early prediction of severity in acute ischemic stroke and transient ischemic attack using platelet parameters and neutrophil-to-lymphocyte ratio. J Clin Lab Anal. 2019;33:e22714. doi:10.1002/jcla.22714
13. Hirahara T, Arigami T, Yanagita S, et al. Combined neutrophil-lymphocyte ratio and platelet-lymphocyte ratio predicts chemotherapy response and prognosis in patients with advanced gastric cancer. BMC Cancer. 2019;19:672. doi:10.1186/s12885-019-5903-y
14. Lin SK, Chen PY, Chen GC, et al. Association of a high neutrophil-to-lymphocyte ratio with hyperdense artery sign and unfavorable short-term outcomes in patients with acute ischemic stroke. J Inflamm Res. 2021;14:313–324. doi:10.2147/JIR.S293825
15. Adams HP
16. Kassardjian CD, Willems JD, Skrabka K, et al. In-patient code stroke: a quality improvement strategy to overcome knowledge-to-action gaps in response time. Stroke. 2017;48:2176–2180. doi:10.1161/STROKEAHA.117.017622
17. Lu MY, Chen CH, Yeh SJ, et al. Comparison between in-hospital stroke and community-onset stroke treated with endovascular thrombectomy. PLoS One. 2019;14(4):e0214883. doi:10.1371/journal.pone.0214883
18. Su YC, Lim SN, Yang FY, Lin SK. Evaluation of cerebral blood flow in acute ischemic stroke patients with atrial fibrillation: a sonographic study. J Formos Med Assoc. 2017;116:287–294. doi:10.1016/j.jfma.2016.05.009
19. Wei M, Lyu H, Huo K, et al. Impact of bone fracture on ischemic stroke recovery. Int J Mol Sci. 2018;19:1533. doi:10.3390/ijms19051533
20. Kang JH, Chung SD, Xirasagar S, et al. Increased risk of stroke in the year after a hip fracture: a population-based follow-up study. Stroke. 2011;42:336–341. doi:10.1161/STROKEAHA.110.595538
21. Chen GC, Hung JL, Chen PY, Su YC, Tzeng IS, Lin SK. Coexistence of acute ischemic stroke and acute bone fracture during hospitalization. Int J Gerontol. 2021;15:67–72. doi:10.6890/IJGE.202101_15(1).0014
22. Kothari RU, Pancioli A, Liu T, Brott T, Broderick J. Cincinnati Prehospital Stroke Scale: reproducibility and validity. Ann Emerg Med. 1999;33:373–378. doi:10.1016/s0196-0644(99)70299-4
23. Lazzerini PE, Hamilton RM, Boutjdir M. Editorial: cardioimmunology: inflammation and immunity in cardiovascular disease. Front Cardiovasc Med. 2019;6:181. doi:10.3389/fcvm.2019.00181
24. Greten FR, Grivennikov SI. Inflammation and cancer: triggers, mechanisms, and consequences. Immunity. 2019;51:27–41. doi:10.1016/j.immuni.2019.06.025
25. Lommatzsch M, van Eeden SF. Immune modulation in chronic respiratory diseases: the path to precision medicine. Respiration. 2020;99:548–549. doi:10.1159/000509648
26. Vester H, Huber-Lang MS, Kida Q, et al. The immune response after fracture trauma is different in old compared to young patients. Immun Ageing. 2014;11:20. doi:10.1186/s12979-014-0020-x
27. Urra X, Cervera A, Villamor N, Planas AM, Chamorro A. Harms and benefits of lymphocyte subpopulations in patients with acute stroke. Neuroscience. 2009;158:1174–1183. doi:10.1016/j.neuroscience.2008.06.014
28. Faura J, Bustamante A, Miró-Mur F, Montaner J. Stroke-induced immunosuppression: implications for the prevention and prediction of post-stroke infections. J Neuroinflamm. 2021;18:127. doi:10.1186/s12974-021-02177-0
29. Smeeth L, Thomas SL, Hall AJ, Hubbard R, Farrington P, Vallance P. Risk of myocardial infarction and stroke after acute infection or vaccination. N Engl J Med. 2004;351:2611–2618. doi:10.1056/NEJMoa041747
30. Sebastian S, Stein LK, Dhamoon MS. Infection as a stroke trigger. Stroke. 2019;50:2216–2218. doi:10.1161/STROKEAHA.119.025872
31. Elkind MSV, Boehme AK, Smith CJ, Meisel A, Buckwalter MS. Infection as a stroke risk factor and determinant of outcome after stroke. Stroke. 2020;51:3156–3168. doi:10.1161/STROKEAHA.120.030429
32. Yu AXY, Hill MD. In-hospital acute strokes—opportunities to optimize care and improve outcomes. JAMA Neurol. 2020;77(12):1482–1483. doi:10.1001/jamaneurol.2020.3368
33. Caparros F, Ferrigno M, Decourcelle A, et al. In hospital ischaemic stroke treated with intravenous thrombolysis or mechanical thrombectomy. J Neurol. 2017;264(8):1804–1810. doi:10.1007/s00415-017-8570-4
34. Manners J, Khandker N, Barron A, et al. An interdisciplinary approach to inhospital stroke improves stroke detection and treatment time. J Neurointerv Surg. 2019;11:1080–1084. doi:10.1136/neurintsurg-2019-014890
35. Tzeng IS. To handle the inflation of odds ratios in a retrospective study with a profile penalized log-likelihood approach. J Clin Lab Anal. 2021;35(7):e23849. doi:10.1002/jcla.23849
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


