Back to Journals » Journal of Pain Research » Volume 13
Comparison of Analgesic Effect Between Erector Spinae Plane Block and Transversus Abdominis Plane Block After Elective Cesarean Section: A Prospective Randomized Single-Blind Controlled Study
Authors Boules ML , Goda AS , Abdelhady MA , Abu El-Nour Abd El-Azeem SA, Hamed MA
Received 10 March 2020
Accepted for publication 1 May 2020
Published 19 May 2020 Volume 2020:13 Pages 1073—1080
DOI https://doi.org/10.2147/JPR.S253343
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Michael Schatman
Maged Labib Boules, Abeer Shaban Goda, Mahdy Ahmed Abdelhady, Shimaa Adel Abu El-Nour Abd El-Azeem, Mohamed Ahmed Hamed
Department of Anesthesiology, Faculty of Medicine, Fayoum University, Cairo, Egypt
Correspondence: Mohamed Ahmed Hamed
Department of Anesthesiology, Faculty of Medicine, Fayoum University, Fayoum 63511, Egypt
Tel +2011 18 560 065
Email [email protected]
Background: This study compared the analgesic efficacy of a bilateral erector spinae plane (ESP) block with that of a bilateral transversus abdominis plane (TAP) block after elective cesarean delivery.
Methods: Sixty mothers scheduled for elective cesarean delivery under spinal anesthesia were randomly allocated to receive either ESP block or TAP block. The ESP group received ESP block at the level of the ninth thoracic transverse process with 20 mL of 0.25% bupivacaine at the end of surgery. The TAP group received an ultrasound-guided TAP block with 20 mL of 0.25% bupivacaine on completion of delivery. The primary outcome was the duration of analgesia achieved by each block. Secondary outcome measures were the postoperative pain severity, total tramadol consumption, patient satisfaction.
Results: The median (interquartile range) duration of block was longer in the ESP group than in the TAP group (12 hours [10, 14] vs 8 hours [8, 8], p< 0.0001). In the first 24 hours, the mean visual analog pain score at rest was lower by 0.32 units in the ESP group. The median tramadol consumption in the first 24 hours was significantly higher in the TAP group than in the ESP group (125 mg [100, 150] vs 100 mg [75, 100, p=0.003]).
Conclusion: Compared with the TAP block, the ESP block provides more effective pain relief, has a longer duration of analgesic action, prolongs time to first analgesic requirement, is associated with less tramadol consumption, and can be used in multimodal analgesia and opioid-sparing regimens after cesarean section.
Keywords: erector spinae plane block, transversus abdominis plane block, cesarean, analgesia, tramadol
Introduction
Postoperative pain relief after elective cesarean delivery is challenging because it needs to provide maternal satisfaction while having no adverse effects on the baby.1
Spinal anesthesia is the most well-known technique used in cesarean delivery operations because it provides effective and rapid anesthesia and is technically easy to perform. Further advantages are that there is no risk of failed intubation or aspiration of gastric contents and no requirement for use of depressant drugs. However, despite these benefits, spinal anesthesia does not provide adequate postoperative pain relief.2
Various techniques are used for postoperative pain relief after cesarean delivery under spinal anesthesia, including intrathecal and/or systemic opioids, abdominal nerve blocks, and truncal blocks such as the transversus abdominis plane (TAP) block with parenteral analgesics and bilateral erector spinae plane (ESP) block.3,4
TAP block has gained popularity as an effective analgesia technique in mothers undergoing cesarean delivery and works by blocking the anterior rami of the spinal nerves of the abdominal anterior wall after spreading of the local anaesthetic agent in the neurofascial plane between the internal oblique and transversus abdominis muscle, thereby relieving the pain of cesarean section.5
Recent publications have demonstrated that the ESP block serves as a practical component of a multimodal regimen for pain relief after various types of operations, including cesarean delivery, by blocking both the dorsal and ventral branches of the thoracic and abdominal spinal nerves; therefore, it provides both somatic and visceral analgesia.4,6
We hypothesized that bilateral ESP block would provide more effective and prolonged pain relief than TAP block after elective cesarean delivery and could be used as part of a multimodal opioid-sparing analgesia technique. The aim of this study was to compare the analgesic efficacy of bilateral ESP block with that of bilateral TAP block after elective cesarean delivery under spinal anesthesia. The primary study outcome was the duration of analgesia provided by these two types of block.
Methods
This prospective, randomized, single-blind, single-center clinical trial was approved by the ethical review board of Fayoum University Hospital and performed in compliance with the Declaration of Helsinki after registration on ClinicalTrials.gov (NCT04016688; principal investigator, Mohamed Ahmed Hamed; date of registration, July 8, 2019, with no plan to share individual participant data). Written informed consent was obtained from all study participants. Prospective participants were scheduled for elective cesarean delivery under spinal anesthesia between July 15, 2019, and December 31, 2019. The enrolment date of patients was 15 July 2019. The design of the study adheres to the applicable CONSORT guidelines (Figure 1).
 |
Figure 1 Consort flow diagram of the study population. |
Sixty women aged 18–40 years with American Society of Anesthesiologists physical status ІІ who were scheduled for elective cesarean delivery via a Pfannenstiel incision under intrathecal anesthesia were included in the trial. The exclusion criteria were as follows: local infection; major hepatic, renal, or cardiovascular disease; a bleeding disorder; known anaphylaxis to any drug used in the trial; and a contraindication to regional anesthesia.
The women were randomly allocated in equal numbers to an ESP group or a TAP group using computer-generated random numbers placed in separate opaque envelopes that were opened by the study investigator just before performing the block. All blocks were done by the same anesthesiologist. The functional data collectors were blinded to randomization until completion of the trial.
As per routine hospital practice, the pre-anesthetic assessment was performed, 1 mg of granisetron and 50 mg of ranitidine were administered intravenously (IV) as premedications one hour before the operation, and 10 mL/kg of Ringer’s lactate solution was infused for 15 minutes as a preload. All the study participants received a standard spinal anesthetic consisting of 10–12 mg of 0.5% hyperbaric bupivacaine. The mother was then moved immediately to the supine position with a 15° left tilt and fitted with a nasal oxygen catheter. After confirmation of a sufficient level of anesthesia, cesarean delivery was performed with continuous hemodynamic monitoring of blood pressure and heart rate. If the systolic blood pressure decreased to 20% below the baseline or less than 90 mmHg, 5 mg of ephedrine were injected IV. Moreover, if the heart rate reduced to 50 bpm or less, 0.5 mg of atropine was injected IV. Upon delivery, 10 U of oxytocin were injected by IV infusion.
At the end of delivery, women allocated to the ESP group underwent bilateral ESP block. The woman was turned into the lateral position to receive the block. After sterilization of the skin at the level of the ninth thoracic transverse process, a linear ultrasound probe (Philips, Saronno, Italy) was placed vertically 3 cm lateral to the spinous process to visualize the trapezius and erector spinae muscles.
A 22-G short-bevel needle (Spinocan, B. Braun, Melsungen AG, Germany) was inserted in the cranial-caudal direction using the in-plane method until it made contact with the transverse process. The needle tip was confirmed to be correctly positioned by injection of 1 mL of saline and visualization of linear fluid spreading between the erector spinae muscle and the transverse process. After aspiration to exclude vascular puncture, 20 mL of 0.25% bupivacaine were injected. The same intervention was performed on the other side of the back.
Women in the TAP group underwent a bilateral TAP block in the supine position. According to the routine technique used in our institute, a linear probe (Phillips) was placed transversely on the anterolateral abdominal wall in the midaxillary line between the costal margin and iliac crest to identify the three layers of muscles, i.e., external oblique, internal oblique, and transversus abdominis. A 22-G short-bevel needle (Spinocan) was introduced using the in-plane technique to reach the TAP between the internal oblique and transversus abdominis muscles. After aspiration to exclude vascular puncture, 20 mL of 0.25% bupivacaine were injected. The procedure was repeated on the contralateral side.
All women were instructed to report any symptoms of local anesthetic toxicity, such as circumoral or tongue numbness, visual or auditory disturbance, dizziness, or tinnitus.
The spinal level was assessed and recorded before either type of block was administered. At the end of delivery, the women were transferred to the postoperative anesthesia care unit for routine monitoring and then to the obstetric department when they had a modified Aldrete score ≥9. In the obstetric department, they received an IV infusion of paracetamol 1 g at 8-hour intervals and IV ketorolac 30 mg at 12-hour intervals for postoperative analgesia, according to the obstetric department’s protocol. The women also received postoperative analgesia with intravenous tramadol through patient-controlled analgesia (PCA) (concentration of 4mg/mL) with a 20 mg dose, 10 minutes lockout interval, and 1 hour limit of 50 mg, without a background dose.
Postoperative pain was assessed by the visual analog scale (VAS) pain score (range, 0–10; 0, no pain; 10, worst pain) at rest and after cough. Mean arterial blood pressure and heart rate were measured on arrival in the postoperative anesthesia care unit (time 0) and at 4, 8, 12, and 24 hours postoperatively.
The duration of block (defined as the interval between performing the block and the time of the first request for analgesia) and total tramadol consumption were recorded in the 24 hours after surgery and retrieved from the electronic memory in the patient-controlled analgesia device.
Patient satisfaction was assessed on a four-point scale (1, excellent; 2, good; 3, fair; 4, poor). Any adverse effects or complications were recorded.
The primary study outcome was the duration of analgesia achieved by each type of block. The secondary outcomes were the postoperative pain severity assessed by the VAS pain score at rest and after cough at 0, 4, 8, 12, and 24 hours, total tramadol consumption, patient satisfaction, and any adverse effects or complications.
Statistical Analysis
The required sample size was calculated using the G power program 3.1.9.4. Based on previous studies on the duration of both blocks,14,15,26 the minimal sample size in each group is 27 patients to get power level of 0.80, an alpha level of 0.05 (two-tailed) and effect size of 0.78 for the duration (mean ± SD in TAP block group and ESP group is 8 ± 4 and 12 ± 6, respectively). The calculated sample size was increased by 10% to reach 30 in each group to allow for dropouts.
The collected data were organized, tabulated, and statistically analyzed using SPSS software statistical computer package version 18 (IBM Corp., Armonk, NY, USA). Numerical variables, such as age and body weight, were normally distributed and are summarized as the mean ± standard deviation. An independent t-test was used to compare the mean values in the two groups. Other variables were not normally distributed and are presented as the median and interquartile range (IQR); the Mann–Whitney U-test was used as a test of significance. Linear mixed models were used to account for repeated measures of VAS scores. A fixed-effect model was used for group and a random-effects model was used to adjust for repeated measures over time. The time-to-event variables were evaluated using the Kaplan-Meier method, and the Log rank test was used to compare the groups. Qualitative data are presented as the number and percentage, and the chi-squared test was used to determine significance. A two-sided p-value of <0.05 was considered statistically significant.
Results
Of 112 women evaluated for eligibility, 15 did not meet the inclusion criteria, 6 declined to participate, 18 met an exclusion criterion, and 13 underwent emergency cesarean delivery. Data for 30 women in each group were analyzed (Figure 1). There was no significant between-group difference in age, body weight, spinal level, or parity (Table 1).
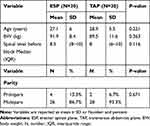 |
Table 1 The Parturients Characteristics |
There was a significant difference in median (IQR) duration of analgesia between the ESP group and the TAP group (12 hours [10, 14] vs 8 hours [8, 8]; p<0.0001) as shown in Table 2 and Figure 2.
 |
Table 2 Comparison of the Duration of the Block of the Two Groups |
 |
Figure 2 The time for first analgesic request. |
Table 3 shows that the VAS pain score was significantly lower in the ESP group than in the TAP group at 8 and 12 hours (p<0.0001). However, there was no statistically significant between-group difference in the VAS score at other times (p>0.05).
 |
Table 3 Comparison of the VAS Score at Rest and with Cough Between the Groups |
After adjustment of the VAS pain scores at rest for repeated measures, these scores were 0.32 units lower on average in the ESP group than in the TAP group (estimate −0.32, 95% CI −0.12 to −0.52, t= −3.234, p=0.002) during the first 24 postoperative hours and 0.48 units lower in the ESP group (estimate −0.48, 95% CI −0.17 to −0.78, t= −3.148, p=0.003) in the first 8 postoperative hours. The VAS pain scores after cough were on average 0.49 units lower in the ESP group than in the TAP group (estimate=−0.49, 95% CI −0.09 to −0.88, t= −2.421, p=0.016) during the first 24 postoperative hours and 0.61 units lower on average in the ESP group (estimate −0.61, 95% CI −0.36 to −0.86, t= −5.014, p<0.0001) during the first postoperative 8 hours (Figure 3). The median (IQR) total tramadol consumption in the first 24 hours was significantly higher in the TAP group than in the ESP group (125 mg [100, 150] vs 100 mg [75, 100], p=0.003; Table 2).
 |
Figure 3 VAS score at rest and with cough. |
There was no significant difference in maternal satisfaction between the groups (Table 4).
 |
Table 4 Patient Satisfaction |
No adverse effects or complications were observed in either group.
Discussion
In this study, we found that the duration of analgesia and time to first request for analgesia was longer in women undergoing cesarean delivery when they received an ESP block than when they received a TAP block. VAS pain scores both at rest and after cough were lower in our ESP group than in our TAP group during the first 8 and 12 postoperative hours and were higher in the TAP group during the first 24 postoperative hours. The total tramadol consumption during the first 24 hours was lower in the ESP group.
Pain following cesarean delivery has both visceral and somatic components, and our present findings can be attributed to differences in the mechanism and site of action between the two types of block. The ESP block delivers widespread, potent analgesia unilaterally. This effect is achieved by injecting a local anesthetic into the plane between the erector spinae muscle and the transverse process; the anesthetic then diffuses into the paravertebral space via the spaces between nearby vertebrae and blocks both the dorsal and ventral rami of the spinal nerves.7,8 In contrast, a TAP block is achieved by injecting a local anesthetic into the plane between the internal oblique and transversus abdominis muscles. The spinal roots supplying the thoracolumbar nerves pass through this plane and innervate the anterolateral abdominal wall;9 therefore, a TAP block can only cover somatic pain.10
Over the past two decades, multimodal opioid-sparing analgesia has become a successful alternative to traditional opioid-based analgesia.11 Peripheral nerve blocks and truncal blocks are some of the successful components of multimodal protocols.12 The ESP block has been used successfully in various types of surgery and provides a variable duration of postoperative analgesia. Yamak et al13 documented prolonged analgesia in a patient undergoing lower abdominal cesarean section after bilateral ESP block using a single injection and reported numeric rating scale scores of 1–3 in the first 24 hours.
Tulgar et al14 reported that the analgesic effect of an ESP block lasted for 17, 16, and 13 hours in three patients undergoing different types of abdominal surgery. Furthermore, Hamed et al15 found that the analgesic effect of an ESP block lasted for 12 hours in women undergoing abdominal hysterectomy.
TAP block was reported to be a successful component of a multimodal analgesia protocol for management of post-cesarean pain and to provide better analgesia, decrease opioid consumption, and reduce the incidence of opioid-induced side effects when compared with a sham block.16 Other studies have compared the analgesic efficacy of a TAP block with that of neuroaxial morphine and reported better analgesia with intrathecal morphine but at the expense of side effects.17,18
Meta-analyses by Mishriky et al19 and Champaneria et al20 concluded that a TAP block could be considered when intrathecal morphine is contraindicated or has adverse effects. TAP block can provide effective analgesia in the first 12 hours after transverse incision surgery. A meta-analysis by Abdallah et al10 found that the duration of analgesia achieved by a posterior TAP block after lower abdominal transverse incision surgery was longer than that achieved by a lateral TAP block. They speculated that the posterior TAP block had a better effect because of retrograde spread of the local anesthetic to the paravertebral space.
In this study, there was no significant difference in patient satisfaction between the TAP and ESP groups, possibly because pain management, despite being an important component, is not the only variable affecting satisfaction in women undergoing cesarean delivery.
Bilateral ESP block has no specifically documented adverse reactions. However, pneumothorax was the first reported complication of ESP block21 and motor weakness in the lower extremities was reported after bilateral ESP block in a woman undergoing cesarean section.22 TAP block is considered to have a low incidence of complications. However, a few complications have been reported secondary to TAP block, including intrahepatic injection in a patient with hepatomegaly,23 intraperitoneal misplacement of the TAP catheter without abdominal organ damage, and an anaphylactic reaction after injection of ropivacaine.24 Short-term femoral nerve palsy is a potential complication because of the proximity of the TAP to the femoral nerve.25 In our study, no adverse effects were noted with either type of block but the above-mentioned complications should be kept in mind when performing a TAP block.
This study had some limitations, stemming mainly from the difficulty in documenting the success rate and distribution of either type of block due to the residual block from spinal anesthesia, which extends into the early postoperative period. Furthermore, limited data were available regarding the effectiveness of the ESP block for postoperative analgesia after cesarean delivery, which restricted our ability to compare the present data with those in other reports.
Given that a TAP block via a posterior approach arguably has a better analgesic effect than one via a lateral approach, we recommend that future studies compare the analgesic efficacy of an ESP block with that of a posterior TAP block after cesarean delivery and that these trials be performed in patients under general anesthesia for better assessment of both distribution and success rate.
Conclusions
The ESP block has a longer duration of analgesia, delays the time to first requirement for analgesia, and reduces tramadol consumption when compared with the TAP block and can be used in multimodal analgesia and opioid-sparing regimens after cesarean section.
Registration
This study is registered on ClinicalTrials.gov (NCT04016688; principal investigator: Mohamed Ahmed Hamed; date of registration: July 8, 2019).
Funding
The authors have no sources of funding to declare for this manuscript.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Jadon A, Jain P, Chakraborty S, et al. Role of ultrasound-guided transversus abdominis plane block as a component of multimodal analgesic regimen for lower segment caesarean section: a randomized, double-blind clinical study. BMC Anesthesiol. 2018;18:53.
2. Karatepe U, Ozer A. Evaluation of postoperative analgesic efficacy of transversus abdominis plane block in patients who underwent caesarian section under spinal anesthesia. Biomed Res. 2018;29(10):2101–2105. doi:10.4066/biomedicalresearch.29-17-3880
3. Baeriswyl M, Kirkham KR, Kern C, Albrecht E. The analgesic efficacy of ultrasound-guided transversus abdominis plane block in adult patients: a meta-analysis. Anesth Analg. 2015;121:1640–1654. doi:10.1213/ANE.0000000000000967
4. Santonastaso DP, de Chiara A, Addis A, Mastronardi C, Pini R, Agnoletti V. Ultrasound-guided erector spinae plane block for postoperative pain control after caesarean section. J Clin Anesth. 2019;58:45–46. doi:10.1016/j.jclinane.2019.05.009
5. Canakci E, Gultekin A, Cebeci Z, Hanedan B, Kilinc A. The analgesic efficacy of transverse abdominis plane block versus epidural block after caesarean delivery: which one is effective? TAP block? Epidural block? Pain Res Manage. 2018;1–7. doi:10.1155/2018/3562701
6. Chin KJ, Adhikary S, Sarwani N, Forero M. The analgesic efficacy of pre-operative bilateral Erector Spinae Plane (ESP) blocks in patients having ventral hernia repair. Anaesthesia. 2017;72:452–460. doi:10.1111/anae.13814
7. Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ. The erector spinae plane block: a novel analgesic technique in thoracic neuropathic pain. Reg Anesth Pain Med. 2016;41:621–627. doi:10.1097/AAP.0000000000000451
8. Ueshima H, Otake H. Similarities between the retrolaminar and erector spinae plane blocks. Reg Anesth Pain Med. 2017;42:123–124. doi:10.1097/AAP.0000000000000526
9. Tsai HC, Yoshida T, Chuang TY, et al. Transversus abdominis plane block: an updated review of anatomy and techniques. Biomed Res Int. 2017;2017:8284363. doi:10.1155/2017/8284363
10. Abdallah FW, Laffey JG, Halpern SH, Brull R. Duration of analgesic effectiveness after the posterior and lateral transversus abdominis plane block techniques for transverse lower abdominal incisions: a meta-analysis. Br J Anaesth. 2013;111(5):721–735. doi:10.1093/bja/aet214
11. Rafiq S, Steinbruchel DA, Wanscher MJ, et al. Multimodal analgesia versus traditional opioid-based analgesia after cardiac surgery, a randomized controlled trial. J Cardiothorac Surg. 2014;9(52):1–8. doi:10.1186/1749-8090-9-52
12. Ilfeld BM, Le LT, Ramjohn J, et al. The effects of local anesthetic concentration and dose on continuous infraclavicular nerve blocks: a multicenter, randomized, observer masked, controlled study. Anesth Analg. 2009;108:345–350. doi:10.1213/ane.0b013e31818c7da5
13. Yamak Altinpulluk E, García Simón D, Fajardo-Pérez M. Erector spinae plane block for analgesia after lower segment caesarean section: case report. Rev Esp Anestesiol Reanim. 2018;65(5):284–286. doi:10.1016/j
14. Tulgar S, Selvi O, Kapakli MS. Erector spinae plane block for different laparoscopic abdominal surgeries: case series. Anesthesiology. 2018;2018:3947281.
15. Hamed MA, Goda AS, Basiony MM, Fargaly OS, Ahmed Abdelhady M. Erector spinae plane block for postoperative analgesia in patients undergoing total abdominal hysterectomy: a randomized controlled study original study. J Pain Res. 2019;12:1393–1398. doi:10.2147/JPR.S196501
16. Kanazi GE, Aouad MT, Abdallah FW, et al. The analgesic efficacy of subarachnoid morphine in comparison with ultrasound-guided transversus abdominis plane block after cesarean delivery: a randomized controlled trial. Anesth Analg. 2010;111:475–481. doi:10.1213/ANE.0b013e3181e30b9f
17. Loane H, Preston R, Douglas MJ, Massey S, Papsdorf M, Tyler JA. Randomized controlled trial comparing intrathecal morphine with transversus abdominis plane block for post-cesarean delivery analgesia. Int J Obstet Anesth. 2012;21:112–118. doi:10.1016/j.ijoa.2012.02.005
18. McMorrow RC, Ni Mhuircheartaigh RJ, Ahmed KA, et al. Comparison of transversus abdominis plane block vs spinal morphine for pain relief after caesarean section. Br J Anaesth. 2011;106:706–712. doi:10.1093/bja/aer061
19. Mishriky B, George R, Habib A. Transversus abdominis plane block for analgesia after cesarean delivery: a systematic review and meta-analysis. Can J Anesth. 2012;59(8):766–778. doi:10.1007/s12630-012-9729-1
20. Champaneria R, Shah L, Wilson MJ, Daniels JP. Clinical effectiveness of transversus abdominis plane (TAP) blocks for pain relief after caesarean section: a meta-analysis. Int J Obstet Anesth. 2016. doi:10.1016/j.ijoa.2016.07.00
21. Ueshima H. Pneumothorax after the erector spinae plane block. J Clin Anesth. 2018;48:12. doi:10.1016/j.jclinane.2018.04.009
22. Selvi O, Tulgar S. Ultrasound-guided erector spinae plane block as a cause of unintended motor block. Rev Esp Anestesiol Reanim. 2018. doi:10.1016/j.redar.2018.05.009
23. Farooq MCM, Carey M. A case of liver trauma with a blunt regional anesthesia needle while performing transversus abdominis plane block. Reg Anesth Pain Med. 2008;33(3):274–275. doi:10.1097/00115550-200805000-00016
24. Belavy D, Cowlishaw PJ, Howes M, et al. Ultrasound-guided transversus abdominis plane block for analgesia after caesarean delivery. Br J Anaesth. 2009;103(5):726–730. doi:10.1093/bja/aep235
25. Jankovic Z. Transversus abdominis plane block: the holy grail of anesthesia for (lower) abdominal surgery. Period Biol. 2009;111(2):203–208.
26. Kadam RV, Field JB. Ultrasound-guided continuous transverse abdominis plane block for abdominal surgery. J Anaesth Clin Pharmacol. 2011;27:333–336. doi:10.4103/0970-9185.83676
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
