Back to Journals » Clinical Ophthalmology » Volume 14
Comparison Between Pars Plana Vitrectomy with and without Encircling Band in the Treatment of Pediatric Traumatic Rhegmatogenous Retinal Detachment
Authors Ghoraba HH, Mansour HO, Abdelhafez MA , El Gouhary SM, Zaky AG, Heikal MA , Ghali AAA
Received 15 August 2020
Accepted for publication 14 September 2020
Published 13 October 2020 Volume 2020:14 Pages 3271—3277
DOI https://doi.org/10.2147/OPTH.S275778
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Hammouda Hamdy Ghoraba,1,2 Hosam Othman Mansour,1,3 Mohamed Ahmed Abdelhafez,1 Sameh Mohamed El Gouhary,4 Adel Galal Zaky,4 Mohamed Amin Heikal,5 Ali Ahmed Ali Ghali3
1Magrabi Eye Hospital, Tanta, Egypt; 2Tanta University, Tanta, Egypt; 3Al Azhar University, Damietta Branch, New Damietta, Egypt; 4Meunofia University, Meunofia, Egypt; 5Benha University, Benha, Egypt
Correspondence: Hosam Othman Mansour
Al Azhar University, Damietta Branch, New Damietta, Egypt
Tel +201001559282
Email [email protected]
Background and Objectives: To compare anatomical and visual results of pars plana vitrectomy (PPV) with or without additional encircling band in the management of pediatric traumatic rhegmatogenous retinal detachment (RD) in a tertiary referral center.
Methods: A retrospective review of children diagnosed with traumatic rhegmatogenous retinal detachment treated by pars plana vitrectomy with or without encircling band.
Results: One hundred thirty-nine eyes of 139 children diagnosed with traumatic rhegmatogenous retinal detachment. Surgeries were performed between May 2011 and November 2016. Patients were followed up for at least 18 months after last intervention. The included eyes were categorized into two groups. Group A (vitrectomy with additional encircling band) included 72 eyes of 72 children; 58 boys and 14 girls. Group B (vitrectomy without encircling band) included 67 eyes of 67 children; 58 boys and 9 girls. In group A, the mean age was 9.21± 3.24. Attached retina was achieved in 61% (44 out of 72 eyes), of which 34 eyes remained attached after silicon oil removal, and 10 eyes remained attached under silicon oil tamponade. Recurrent RD under oil was present in 28 eyes (38.9%). In group B, the mean age was 11.06± 3.64. Attached retina was present in 61.2% (41 out of 67 eyes), of which 30 eyes remained attached after oil removal, and 11 eyes remained attached under silicon oil tamponade. Recurrent RD was present in 26 eyes (38.8%). In group A, the final visual acuity (VA) ranged from NLP to 0.5; 58.7% of patients achieved VA more than counting fingers at 1 meter, and 34.6% of patients achieved VA of 0.05 or more. In group B, the final postoperative VA ranged from NLP to 0.9; 16% of patients achieved VA from counting fingers at 1 meter to 0.05, and 29.2% achieved VA of 0.05 or more.
Conclusion: Although no statistically significant difference between the two groups (combined vitrectomy and encircling band versus vitrectomy alone in pediatric traumatic retinal detachment), it is wise to consider adding encircling band in severe trauma cases.
Keywords: trauma, pediatric retinal detachment, encircling band, pars plana vitrectomy, silicon oil
Background
Eye injuries are the leading cause of monocular visual disability and monocular blindness in children.1
One of the consequences of ocular trauma is retinal detachment.2 Pediatric retinal detachment (RD) constitutes 3.2–6.6% of all cases of RD.3 Consequently, pediatric RD is a great challenge for ophthalmologists. Children usually present late and have clinical features of longstanding RD such as macular involvement and proliferative vitreoretinopathy (PVR).4 Although traumatic retinal detachments in the pediatric population have been discussed, no study compared the role of adding or omitting encircling band in conjunction with pars plana vitrectomy. The introduction of trans conjunctival surgery decreased the need for 360° SB. Starting from 2009, we shifted to trans conjunctival PPV (20G, 23G, 25G, or combined cannula system). We omitted using 360ₒ encircling band to get the benefits of transconjunctival surgery in 2009. As we were convinced by the role of the encircling band in combination to PPV, we postponed using this technique in children. In this retrospective series we tried to evaluate the role of encircling band in pediatric traumatic RD and whether omitting its use will affect the final results.
Methods
This was a retrospective interventional non-comparative case series that included children with traumatic rhegmatogenous retinal detachment. Data of patients was retrospectively collected from medical records among pediatric RRD cases operated on in Magrabi eye hospital in the period from May 2011 to November 2016. The follow-up period was at least 18 months after the last surgical intervention. All surgeries were performed by the same surgeon (H.G.).
Ethics Approval and Consent to Participate
The institutional review board of Magrabi Eye Hospital and Center approved the present study. All parents or legal custodians of the children recruited in the study received a thorough explanation of the nature of the surgical procedures entailed, the expected outcome and possible complications, and provided an informed consent. The informed consent ensured the use of their data to be used in these study. Only those accepted for publication were enrolled in the study. The study adhered strictly to the tenets of the Declaration of Helsinki (2013 revision).
Inclusion Criteria
Children diagnosed as traumatic rhegmatogenous retinal detachment.
Exclusion Criteria
- Children treated by scleral buckle only (conventional buckle and cryo).
- Children who did not complete the follow-up period, ie, 18 months after the last surgical intervention.
- Children who had previous PPV.
- Cases of retinal detachment secondary to traumatic endophthalmitis.
Surgical Procedures
A written (informed) consent was obtained from the parents. Vitreoretinal intervention was done immediately after referral once the condition of the globe was suitable. Group A (operated before June 2014) included 72 children, and we applied 360° encircling scleral 240 band. Group B (operated after June 2014), included 67 children without additional encircling band. Lens-sparing vitrectomy in both groups, but a lensectomy was done in cataractous eyes, subluxated lens or if lens touch occurred. The vitrectomy procedure consisted of core vitrectomy; triamcinolone acetonide (TA) assisted posterior vitreous detachment (PVD) induction. Perfluorocarbon liquid was used to stabilize the posterior retina. Vitreous base shaving was done (as safe as possible). Air-fluid exchange and aspiration of subretinal fluid, endo laser retinopexy followed by silicone oil (SO) 5000 centistokes (CS)/air exchange. Inferior surgical iridectomy (at 6 o’clock) was created in aphakic eyes. Closure of sclerotomies was done using 7/0 vicryl sutures.
Postoperative Care
Cooperative children were instructed to maintain a prone position 8 hours per day for 1 week. All the included children had slit-lamp examination in the first postoperative day. If possible, fundus examination, and color fundus photography were done to asses and document retinal reattachment. The follow-up was scheduled at 1, 3, and 6 weeks, and then every 8 weeks. In each visit, the following data were recorded: best-corrected visual acuity (when possible), intraocular pressure in cooperative children, retinal reattachment. Uncooperative or young children had examination under general anesthesia; anterior segment examination was done using the surgical microscope, IOP was measured using Schiotz tonometer and the fundus was examined using the indirect ophthalmoscope.
Revision Vitrectomy
A second (revision) vitrectomy was preceded for recurrent RD. The revision surgery consisted of SO removal. Triamcinolone assisted removal of any residual vitreous cortex; peeling of epiretinal membranes. Relaxing retinotomy and or retinectomy were used for immobile and shortened retina. Air–fluid exchange and aspiration of sub retinal fluid were done. Endo laser was applied followed by silicone oil 5000 CS injection, and closure of sclerotomies.
Silicone Oil Removal
In eyes with stable retinae for at least 6 months postoperative, SO was removed using 2 ports (20G, 23G or combination of both). One port was used for infusion, and the other for oil aspiration. The retina was thoroughly examined looking at the retinal periphery and the sites of retinal breaks. SO was manually or mechanically aspirated, followed by partial air fluid exchange (multiple times). Some adjuvant procedures were done (if needed) such as peeling of epimacular membranes; IOL implantation in aphakic eyes if there’s enough capsular support. 7/0 vicryl sutures were used to close sclerotomies.
Statistical Analysis
The clinical data were recorded in a report form. These data were tabulated and analyzed using SPSS computer program (statistical package for social science) version 20. Statistical tests used are mean, SD, chi-square test, and P value. P value ˂ 0.05 was considered statistically significant, whereas ˃ 0.05 was statistically insignificant. A P value ˂ 0.01 was considered highly significant in all analyses.
Results
Demographic Data
Age
In group A the mean age was 9.21± 3.24, while in group B the mean age was 11.06±3.64, with no statistically significant difference.
Gender
Group A included 72 children; 58 boys, and 14 girls, while group B included 67 children; 58 boys, and 9 girls, Table 1.
 |
Table 1 Demographic Data of the Two Groups |
Preoperative Visual Acuity (VA)
The preoperative visual acuity (VA) ranged from PL to 0.2, and could not be assessed in 4.5% of children in both groups.
In group A, 37.5% of patients had VA of HM, 33.3% had visual acuity PL. Other grades of VA were distributed as follows; CF at 50 cm in 6.9%, CF at 1 m in 11.1%, CF at 2 m in 1.4%, 0.05 in 6.9%, 0.1 in 1.4%, and 0.2 in 1.4%.
In group B, 41.8% of patients had visual acuity of HM, PL vision was present in 32.8%. Other grades of VA were distributed as follows; CF at 20 cm in 1.5%, CF at 50 cm in 4.5%, CF at 1 m in 7.5%, CF at 2 m in 1.5%, 0.05 in 3%, 0.1 in 1.5%, 0.2 in 1.5%, and the vision could not be assessed in 4.5% of cases, Table 2.
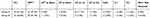 |
Table 2 Preoperative VA in the Two Groups: + Counting Fingers, * Perception of Light, ** Hand Motion, ++ Visual Acuity |
Lens Status
In group A the lens was clear in 38.9%, cataractous in 8.3%, pseudophakic in 9.7%, aphakic in 38.9%, subluxated in 2.8%, and dislocated in 1.4% of patients.
In group B the lens was clear in 46.3%, cataractous in 22.4%, pseudophakic in 8.9%, aphakic in 19.4%, subluxated in 1.5% and dislocated in 1.5%, Table 3
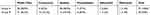 |
Table 3 Lens Status |
Type of Retinal Break
In group A the retinal breaks were located in the upper quadrants in 22.2% and in the lower quadrants in 13.9%, multiple breaks were found in 2.8%, disinsertion in 6.9%, macular hole in 4.2%, giant breaks in 11.1%, central breaks in 2.8%, and undetectable breaks in 34.7%
In group B the retinal break was located in the upper quadrants in 10.4%, in the lower quadrants in 10.4%, multiple breaks in 9%, disinsertion in 4.5%, macular hole in 7.5%, giant breaks in 11.9%, macular exit in 3%, extra macular exit 11.9%, and undetectable in 25.4%, Table 4.
 |
Table 4 Types of the Retinal Breaks; * Macular Hole, ** Giant Tear |
Silicone Oil Removal (SOR)
In cases of stable retinae at least 6 months silicone oil was removed. Silicone oil removal (SOR) was carried out in 34 eyes in group A (47.2%) and in 30 eyes (44.8%) in group B.
Causes of non-removal of SO include hypotony, and recurrent RD under oil that could not be repaired (due to extensive proliferation), Table 5.
 |
Table 5 Silicone Oil Removal |
Duration of SO
The mean duration between the first surgery and silicone oil removal was 11.13±5.46 months in group A and it was 11.7±7.63 months in group B.
Duration of Follow-Up After SOR
All cases were followed up after the last surgical intervention for at least 18 months. Range of follow-up in group A was 18–60 months, and it was 18–81 months in group B.
Procedures Carried Out During SOR
In phakic cataractous eyes irrigation aspiration (IA) of the lens with IOL implantation was done. In group A irrigation and aspiration of the lens with IOL implantation in 16 eyes out of 32 eyes from which SO was removed (50%). Peeling of epimacular membranes (EMM) was done in one eye (3.1%). In group B irrigation and aspiration of the lens with IOL implantation was done in 19 eyes out of 30 eyes from which SO was removed (63.3%), Table 6.
 |
Table 6 Procedures Carried Out During Silicone Oil Removal, * Irrigation Aspiration, ** Intra Ocular Lens, + Epimacular Membrane |
Postoperative (Final) VA
In both groups, the final VA ranged from no PL to 0.9, and the VA could not be assessed in 2.5% of children.
In group A the final VA was distributed as follows; NPL (5%), PL (10.6%), HM (21.3%), CF at 50 cm (1.4%), CF at 1 m (18.4%), CF at 2 m (5.7%), 0.05 (12%), 0.1 (7.8%), 0.16 (5.7%), 0.2 (1.4%), 0.3 (2.8%), 0.4 (2.8%), 0.5 (2.1%).
In group B the final VA was distributed as follows; NPL (10.2%), PL (12.4%), HM (18.2%), CF at 50 cm (8.8%), CF at 1 m (12.4%), CF at 2 m (3.6%), 0.05 (6.6%), 0.1 (5.1%), 0.16 (5.1%), 0.2 (4.4%), 0.3 (2.9%), 0.4 (0.7%), 0.5 (2.2%), 0.6 (1.5%), and 0.9 (0.7%). Table 7 shows the final VA distribution in the two groups.
 |
Table 7 Final VA: Visual Acuity, No Perception of Light, Perception of Light, † Hand Motion, ‡ Counting Fingers |
Final Anatomical Results
In group A attached retina was achieved 44 eyes out of 72 (61.1%), of which 34 eyes (47.2%) remain attached after SOR, and 10 eyes (13.9%) were attached in the presence of SO. Recurrent RD under oil was present in 28 eyes (38.9%). In group B attached retina were reported in 41 eyes (61.2%), 30 eyes (44.8%) remained attached after silicone oil removal, and 11 eyes (16.4%) were kept flat in the presence of SO. Recurrent RD under oil was present in 26 eyes (38.8%%)(Table 8).
 |
Table 8 Final Anatomical Status * Silicone Oil Removal, ** Silicone Oil, + Retinal Detachment |
Discussion
The addition of an encircling band during vitrectomy is a debatable issue especially in pediatric retinal detachment surgery. Since the introduction of transconjunctival PPV there is a decreasing interest in the use of an encircling band.
Starting from 2009, we started transconjunctival PPV without an encircling band, especially this era was accompanied by the introduction of high-speed cutters and bright illuminations that improved the shaving abilities. Nevertheless, we were conservative in abundant encircling band in pediatric retinal detachments until the year 2014. Previous studies5 compared vitrectomy with and without encircling band in cases of myopic macular hole retinal detachment (MHRD) showed no statistically significant difference whether the buckle was added or not. We started to do transconjunctival PPV without additional encircling band in pediatric retinal detachment starting from June 2014.
Many studies6–9 discussed pediatric traumatic retinal detachment from many aspects such as the clinical features, the anatomical and visual outcomes, and the risk factors. Neither of these studies discussed the effect of change in the surgical technique on the outcomes, ie, whether abundant use of encircling band has any effect on either anatomical or visual outcomes.
The aim of this retrospective analysis is to evaluate whether the abundant use of encircling band will affect the final results in pediatric traumatic RD surgery or not. In this study, we compared anatomical and visual results of PPV and SO tamponade with or without encircling band in pediatric traumatic retinal detachment.
We think that it is valuable to address this idea in the category of pediatric traumatic RD as many of these cases have a bad fundus view; due to corneal scarring making vitrectomy more challenging. The rationale of adding scleral buckle is to support the vitreous base, to create new ora; that may compensate inadequate vitreous base shaving (due to poor visualization or strongly adherent vitreous), Moreover the buckle may decreases traction from PVR.
The use of additional buckle helps to preserve the clear crystalline lens as much as possible. In our opinion, keeping the crystalline lens in pediatric surgery is beneficial because it decreases the incidence of postoperative inflammation (which usually is marked in children), as well as aphakia is a huge risk for amblyopia and aphakic glaucoma.
A suggested advantage is that the buckle might decrease the need for retinotomies, and or retinectomies, or it might decrease their size, although there was no statistically significant difference between the two groups in our results.
Sarrazin et al6 compared two groups of pediatric traumatic retinal detachment due to open and closed globe injuries. The study included 60 eyes of 58 children. Retinal detachment followed open globe injury in 37 eyes and in 23 eyes was due to closed globe injuries. The surgical technique included 3-port pars plana vitrectomy with encircling band. The study did not emphasize the change of the technique and its impacts on the outcomes. The study concluded that the anatomic and functional results were guarded. Anatomic outcome was 45% in cases of open globe injury and 65% after closed globe injury. In our study the final anatomical results were 61.2% in both groups, which are comparable to Sarrazin et al.
Chen et al7 studied pediatric RD in Taiwan. The study included 35 eyes, and the main risk factors for RD were congenital anomalies, myopia, and trauma. The study ensured the fact that multiple interventions were needed, and the fellow eye is at risk of RD. The surgical techniques were scleral buckle, vitrectomy or a combination of both techniques. The study showed that anatomical results in the vitrectomy patients approached 50%. Our final anatomical results are comparable to Chen et al; 62.1% in both groups. The visual results ranged from NLP to 1.0. In our study, the VA ranged from NLP to 0.9 in both groups.
Weinberg et al8 studied the risk factors and surgical outcomes of pediatric retinal detachment. The study included 39 eyes treated by conventional scleral buckle 41%, vitrectomy 13%, or combined buckle and vitrectomy 46%. The study concluded the need for multiple procedures, and the poor visual outcomes, which are also similar to our observations. Weinberg et al recorded that 31% of patients had a final vision of NLP. In our study, the incidence of NLP vision was 7.6% in both groups.
Read et al9 reviewed 231 pediatric eyes of different etiologies; 60 eyes of the studied group were traumatic detachments. The surgical procedures were scleral buckle (SB), PPV alone or a combination of both techniques. The incidence of missed retinal break was 50% and 32% of open and closed globe injuries respectively, which are similar to the results in our work; the incidence of missed break was 34.7% in group A, and 25.4% in group B. The overall anatomical success was 65% compared to 62.1% in our study.
All the previous studies used different surgical techniques, scleral buckle, vitrectomy or additional encircling band in addition to vitrectomy. Neither of those studies made a clear conclusion whether the additional band may improve the surgical outcomes.
A summary of some pediatric RD studies is presented in Table 9.
 |
Table 9 Review of Literature of Pediatric Retinal Detachment, SB Scleral Buckle, PPV Pars Plana Vitrectomy, RD Retinal Detachment |
Conclusion
Although there was no statistically significant difference between the two groups (combined vitrectomy and encircling band versus vitrectomy alone in pediatric traumatic retinal detachment), it is wise to consider adding an encircling band in severe trauma cases.
Limitations of the Study
This study is limited by its retrospective nature.
Disclosure
The authors have not received grant support or research funding and they do not have any proprietary interests in the materials described in the article.
References
1. Maltzman HA, Pruzon H, Mund ML. A survey of ocular trauma. Surv Ophthalmol 21: 285–290- Niiranen M, Raivio I (1981) Eye injuries in children. Br J Ophthalmol 65: 436–438- Werner S (1952) on injuries to the eye in children. Acta Ophthalmol. 1976;30:37–104.
2. Haimann MH, Burton TC, Brown CK. Epidemiology of retinal detachment in childhood. Arch Ophhthalmol. 1982;100:289–292. doi:10.1001/archopht.1982.01030030291012
3. Wang N-K, Tsai C-H, Chen Y-P, et al. Pediatric rhegmatogenous retinal detachment in East Asians. Ophthalmology. 2005;112(11):1890–1895. doi:10.1016/j.ophtha.2005.06.019
4. Hjelmel LM, Harvey AK. Chapter 9 gliosis of the mammalian retina: migration and proliferation of retinal glia. Progress Retinal Res. 1988;7:259–281. doi:10.1016/0278-4327(88)90011-9
5. Ghoraba HH, Mansour HO, Elgouhary SM. Effect of 360° episcleral band as adjunctive to pars plana vitrectomy and silicon oil tamponade in the management of myopic macular hole retinal detachment. RETINA. 2014;34(4):670–678. doi:10.1097/IAE.0b013e3182a487ea
6. Sarrazin L, Averbukh E, Halpert M, Hemo I, Rumelt S. Traumatic pediatric retinal detachment, a comparison between open and closed globe injuries. Am j Ophthalmol. 2004;137(6):1042–1048. doi:10.1016/j.ajo.2004.01.011
7. Chen S, Jiunn-Fengn H. Te-Cheng; pediatric rhegmatogenous retinal detachment in Taiwan. Retina. 2006;26:410–414.
8. Weinberg DV, Lyon AT, Greenwald MJ, Mets MB. Rhegmatogenous retinal detachments in children: risk factors and surgical outcomes. Ophthalmology. 2003;110(9):1708–1713. doi:10.1016/S0161-6420(03)00569-4
9. Read S, Aziz H, Kuriyan A, et al. Retinal detachment surgery in pediatric population visual and anatomical outcomes. Retina. 2017;1–10.
10. Butler TK, Kiel AW, Orr GM. “Anatomical and visual outcome of retinal detachment surgery in children. B J O. 2001;85(12):1437–1439. doi:10.1136/bjo.85.12.1437
11. Madanat AS, Mustafa TA. Pediatric retinal detachment, is it a real challenge? Middle East j Family Med. 2005;3:3.
12. Gonzales CR, Singh S, Singh CR, Kreiger AE, Gupta A, Schwartz SD. Pediatric rhegmatogenous retinal attachment clinical features and surgical outcomes. Retina. 2008;28(6):847–852. doi:10.1097/IAE.0b013e3181679f79
13. Oono Y, Uehara K, Haruta M, Yamakawa R. Characteristics and surgical outcomes of pediatric rhegmatogenous retinal detachment. Clin Ophthalmol. 2012;6:939–943. doi:10.2147/OPTH.S31765
14. Rejdak R, Nowakowska D, Wrona K, Maciejewski R, Junemann AG, Nowomiejska K. Outcomes of vitrectomy in pediatric retinal detachment with proliferative vitreoretinopathy. J Ophthalmol. 2017;6.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
