Back to Journals » Clinical Ophthalmology » Volume 17
Comparing Visual Performance and Subjective Outcomes with an Enhanced Monofocal Intraocular Lens When Targeted for Emmetropia or Monovision
Authors Sandoval HP, Potvin R , Solomon KD
Received 1 October 2023
Accepted for publication 29 November 2023
Published 1 December 2023 Volume 2023:17 Pages 3693—3702
DOI https://doi.org/10.2147/OPTH.S442752
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 6
Editor who approved publication: Dr Scott Fraser
Helga P Sandoval,1 Richard Potvin,2 Kerry D Solomon1
1Carolina Eyecare Physicians / US Eye, Mt. Pleasant, SC, USA; 2Science in Vision, Frisco, TX, USA
Correspondence: Kerry D Solomon, Carolina Eyecare Physicians, LLC, 1101 Clarity Road, Suite 100, Mt. Pleasant, SC, 29464, USA, Email [email protected]
Purpose: To evaluate relative visual performance and subjective outcomes after implantation of the TECNIS Eyhance™ intraocular lens (IOL) targeted for bilateral emmetropia or monovision.
Methods: This was a prospective, single-center randomized, patient-masked trial. Patients were implanted with the enhanced IOL targeted for bilateral emmetropia or slight monovision (− 0.75 D in the non-dominant eye). At 3 months the binocular visual acuity (VA) was measured at distance, intermediate and near, along with low contrast VA in photopic and mesopic conditions, and the distance corrected defocus curve. Questionnaires related to spectacle independence, satisfaction, visual symptoms, and functional vision were administered.
Results: Data from 71 subjects (34 Emmetropia, 37 Monovision) were analyzed. There was no difference in the mean uncorrected distance VA (p = 0.11), but uncorrected intermediate and near VAs were one line better in the Monovision group (p = 0.02 and 0.01, respectively). Mesopic and photopic low contrast VA were similar between groups. There was a trend for less difficulty and higher satisfaction with near and intermediate vision in the Monovision group, but no significant differences in any of the subjective questionnaires. Difficulty reading was the most reported concern in both groups, though 93% of all subjects reported “little” or “no” difficulty with daily activities. Overall, 82% of subjects were “completely” or “very” happy with their lens choice.
Conclusion: Using this enhanced IOL with slight monovision in the non-dominant eye increased intermediate and near VA with no apparent effect on low contrast distance VA, subjective visual quality, or satisfaction.
Keywords: Tecnis Eyhance, enhanced monofocal, monofocal plus, monovision
Introduction
The range of correction options for patients presenting for cataract surgery has arguably never been broader, with monofocal intraocular lenses (IOLs), bifocal and trifocal IOLs, extended depth of focus (EDOF) IOLs, and hybrid diffractive/EDOF designs.1–3 These have been used bilaterally as well as in combination in an attempt to provide the best vision for each patient, based on their post-surgical vision goals.4 For patients interested in reducing their dependence on spectacles after surgery the tradeoff with multifocal and EDOF IOLs versus monofocal IOLs is between a longer range of focus and a higher likelihood of visual disturbances such as glare or halos.2,5,6
With the increasing use of computers and hand-held devices, vision at intermediate distances appears a more important indicator of post-surgical satisfaction than vision at near, though this is likely to remain patient-specific based on individual preferences and tolerance for visual disturbances.7–9 Postoperative photic phenomena remain a concern for multifocal and EDOF patients.
An alternative to EDOF and multifocal IOLs is an enhanced monofocal IOL; the Tecnis Eyhance™ IOL (Johnson & Johnson Surgical Vision, Santa Ana, CA) is one such lens. It was approved by the US FDA as a monofocal IOL in February of 2021. It incorporates a higher level of asphericity on the anterior surface to slightly extend the focal length of the lens. It is not defined as an EDOF lens, but is a modification of a monofocal IOL designed to provide improved intermediate vision with no change in the frequency or severity of visual disturbances relative to a monofocal IOL. A multicenter study in Europe found that the lens provided about one line of additional intermediate vision with no significant effect on distance vision and a comparative visual disturbance profile to a monofocal IOL of similar design.10 These results have been corroborated with several smaller studies.11–14
To extend the useful range of vision, monofocal IOLs may be used in a monovision modality, leaving the non-dominant eye slightly myopic. This is a procedure that has shown very good success with standard monofocal IOLs, with levels of anisometropia up to 1.5 D generally well-tolerated, though a target of < 1.0 D of myopia is most common.15–17 However, some recent reports have shown that a non-diffractive EDOF IOL can cause significantly higher levels of visual disturbances in some patients when used in a monovision modality18,19 It is prudent, therefore, to consider whether slight monovision is appropriate with the enhanced monofocal lens studied here.
This study was designed to compare the clinical and subjective results obtained with this lens when implanted with a target of emmetropia in both eyes to results when the non-dominant eye was targeted for slight monovision.
Methods
This was a prospective, patient-masked, randomized study conducted at one site in the USA. It was designed to compare clinical results and subjective patient responses after bilateral implantation of the study lens in two groups. The first group was targeted for a plano refraction in both eyes (Emmetropia group) while the second group had a slight monovision target (−0.75 D ± 0.15 D) in the non-dominant eye (Monovision group). The study was reviewed and approved by an institutional review board (Salus IRB, Austin, TX, USA) and registered with clinicaltrials.gov (record NCT05069415). The study was conducted using good clinical practice (GCP) protocols and adhered to the tenets of the Declaration of Helsinki. All subjects reviewed and signed an approved informed consent document.
Subjects included patients over 50 presenting for bilateral cataract surgery, with no corneal or retinal pathology likely to influence results, who were willing and able to sign the informed consent. Subjects had to have a potential postoperative visual acuity of 0.2 logMAR (20/32 Snellen) or better in both eyes. Exclusion criteria included, but were not limited to: prior cataract or refractive surgery, systemic inflammation, uncontrolled diabetes, irregular astigmatism, severe dry eye, any planned secondary procedure (eg, glaucoma stent) and use of systemic or topical drugs known to affect visual performance.
The preoperative visit was conducted using the standard procedure, including measurement of visual acuity, refraction, corneal topography (if a toric IOL was being considered), eye dominance, with slit lamp and dilated fundus examinations also being conducted. Eligible subjects were then randomized to Group A (Emmetropia) or Group B (Monovision). Spherical IOL power was calculated using the Barrett Universal II formula. Toric power was calculated using the Barrett K Calculator (Barrett Integrated K, BIK) using data from the Lenstar LS900® (Haag-Streit AG, Koeniz, Switzerland), the IOLMaster® 700 (Carl Zeiss Meditec, Inc., Dublin, CA), and the Pentacam® (Oculus, Inc., Arlington, WA, USA). Small incision cataract surgery was performed using the surgeon’s preferred technique with traditional phacoemulsification procedures. Cataract extraction by standard phacoemulsification was performed using a 2.2 mm clear corneal incision. The primary incision location for all surgeries was 170 degrees in the right eye and 350 degrees in the left eye. After lens removal and IOL implantation, the posterior capsule was polished and the residual viscoelastic was removed using irrigation/ aspiration. The incision was closed using stromal hydration. No sutures were used. An intracameral antibiotic was irrigated into the anterior chamber at the conclusion of the procedure. All surgeries were performed by the same surgeon (KDS). The clinic’s standard postoperative care routines were followed after surgery.
Subjects had their final study evaluation 3 months (75 to 115 days) after second-eye surgery. Postoperative data collected included a manifest refraction and binocular distance-corrected and uncorrected VA at distance (CDVA, UDVA, respectively), intermediate (66 cm, DCIVA, UIVA, respectively) and near (40 cm, DCNVA, UNVA, respectively). The binocular distance-corrected defocus curve was measured as well as binocular low contrast (10%) photopic and mesopic CDVA. For the purposes of this study, distance-corrected is defined as the dominant eye corrected for emmetropia and the non-dominant eye corrected for either emmetropia (Emmetropia group) or −0.75 D (Monovision group). Lens position and orientation (for toric IOLs) were checked. All subjects were screened for adverse events at all visits.
A series of questionnaires were also administered to subjects, including the Patient Reported Spectacle Independence Questionnaire (PRSIQ),20 the Patient Reported Visual Symptom Questionnaire (PRVSQ) and a supplemental questionnaire used at the practices to evaluate issues with specific activities such as driving (the latter two are proprietary).
The primary endpoint for the study was the binocular distance-corrected intermediate visual acuity. Assuming a standard deviation of 0.12 D for the intermediate visual acuity endpoint (from a previous Eyhance study), it was determined that to detect a difference of 0.1 logMAR (a 1-line difference) with 90% power a total of 31 subjects in each group (emmetropia / mini monovision) would be required. This was based on a two-sided t-test (alpha =0.05).
The diagnostic data were collected in Excel spreadsheets, and imported into an Access database for preliminary analysis (both Microsoft Corp., Redmond, USA). Statistical analyses were conducted using the Statistica data analysis software system, version 12 (TIBCO Software Inc., Palo Alto, CA, USA). Analysis of variance was used for parametric comparisons while appropriate non-parametric tests were used for categorical data; in all cases a P value of 0.05 was considered statistically significant. The informed consent document precluded sharing data outside the study, so the data are not available.
Results
A total of 75 subjects were successfully recruited. Two subjects voluntarily withdrew from the study while two others experienced unrelated adverse events that resulted in their exit from the study (one central retinal vein occlusion, one ischemic optic neuropathy). Analysis therefore included 34 subjects in the Emmetropia group and 37 in the Monovision group. Demographic data, preoperative refraction and the IOL power implanted for these 71 subjects are summarized in Table 1. Groups were well matched by age, sex, preoperative refractive status and IOL sphere power. About half the eyes in each group received a toric IOL (68/142, 48%), with no significant difference in these variables between groups (t-test for parametric variables, chi-squared test for categorical variables, p > 0.05 in all cases).
 |
Table 1 Demographics and Preoperative Status by Group |
The postoperative mean refraction spherical equivalent (MRSE) for the 37 non-dominant eyes in the Monovision group was −0.76 ± 0.10 D, ranging from −0.52 D to – 0.91 D. The remaining 105 eyes had a postoperative (MRSE) of 0.00 ± 0.11 D, with a range of −0.19 to +0.16 D. In the Monovision group the postoperative MRSE was statistically significantly different in the non-dominant eyes vs the dominant eyes (−0.64 ± 0.52 D vs 0.04 ± 0.28 D, P < 0.001). There was no statistically significant difference in the MRSE of eyes targeted for emmetropia by group (P = 0.15). Overall postoperative refractive cylinder was 0.20 ± 0.22 D, ranging from 0.0 to 0.75 D, with no statistically significant difference between the eyes targeted for monovision or emmetropia (p = 0.18).
Figure 1 shows the binocular uncorrected visual acuity at various test distances by group. There was no statistically significant difference in the mean uncorrected distance visual acuity (UDVA, P = 0.11), but uncorrected intermediate (UIVA) and near (UNVA) VAs were statistically significantly better in the Monovision group (P = 0.02 and 0.01, respectively), averaging just over one line better at both distances. Results, while not shown, were slightly better for the distance-corrected VA data. There was no statistically significant difference between groups at distance (P = 0.53), but the Monovision group had a mean distance-corrected intermediate visual acuity (DCIVA) that was 1.5 lines better than the Emmetropia group (0.04 vs 0.19, P < 0.01) and a mean distance-corrected near visual acuity (DCNVA) that was 2 line better than the Emmetropia group (0.21 vs 0.43, P < 0.01). The preferred reading distance in both groups was 41 cm (range 32 to 57 cm), with no significant difference between groups (P = 0.87), though the Monovision group had a distance-corrected VA at the preferred distance that was about 2 lines better than the Emmetropia group (0.18 vs 0.37, P < 0.01).
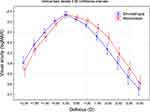
Figure 2 shows the distance-corrected binocular defocus curve for the two groups; data were available for 34 subjects from each group. Results are very similar to those obtained from the visual acuity testing at various distances, with statistically significantly better VA in the Monovision group from −1.00 D to −2.50 D (P < 0.03 in all cases), a dioptric range approximately equivalent to a range of vision from one meter to 40 cm. The percentage of subjects in the Monovision group that had 0.2 logMAR (20/32) or better VA from 0.0 D to −2.0 D (distance to 50 cm) was significantly higher than in the Emmetropia group (71% vs 31%, P < 0.01).
Figure 3 contains a box plot showing the distribution of the distance-corrected low contrast visual acuity (LCVA) by lighting condition and group. There was no statistically significant difference between the groups in either mesopic (P = 0.79) or photopic conditions (P = 0.81), though for both groups the LCVA in mesopic conditions was about two lines lower than in photopic conditions; this was a statistically significant difference (P < 0.01).
 |
Figure 3 Distance-corrected low contrast visual acuity by group and lighting level. Abbreviation: logMAR, log of the minimum angle of resolution. |
Table 2 summarizes the results for the Patient Reported Spectacle Independence Questionnaire. There were clear trends for the Monovision group to have less difficulty with intermediate and near tasks, and higher satisfaction with near and intermediate vision, but the results were not statistically significantly different between the groups.
 |
Table 2 PRSIQ Summary Results |
Figure 4 shows a summary of the frequency of various visual disturbances reported in the Patient Reported Visual Symptom Questionnaire, while Figure 5 shows how much subjects reported being bothered by them. The most frequently reported visual disturbances in both groups were halos and sensitivity to light. There was no statistically significant difference between the groups in terms of the number of subjects reporting that they “never” or “rarely” experienced these (P > 0.24). While most common, they were not deemed particularly bothersome: 88% and 86% in the Emmetropia and Monovision groups respectively reporting they were “never” or “rarely” bothered by light sensitivity, with 88% and 95% in the Emmetropia and Monovision groups respectively reporting they were “never” or “rarely” bothered by halos.
 |
Figure 4 Frequency of visual disturbances, by group. Abbreviation: PRVSQ, patient reported visual symptoms questionnaire. Note: occlusions refer to fixed dark or light blocked areas within vision. |
The additional visual function questionnaire indicated that 79% of subjects in the Emmetropia group and 84% of subjects in the Monovision group were “completely” or “very” happy with their lens choice; the difference between groups was not statistically significant (P = 0.63). Only one subject, in the Emmetropia group, reported being “very” or “completely” unhappy. The most reported concern with functional vision in both groups was difficulty reading and the need for reading glasses to do close work. About 20% of subjects across the several questionnaires reported this, though 93% of subjects (66/71) reported “little” or “no” difficulty with daily activities, with no difference between groups (P = 0.71).
Discussion
This study was conducted to determine if slight monovision to improve intermediate and near vision was a viable surgical modality for patients receiving the subject enhanced monofocal IOL. Results indicated that there was no significant difference in distance VA with slight monovision, but binocular intermediate and near vision improved by one or two lines on average. In addition, visual disturbances were low in both groups and not statistically significant between groups. Overall satisfaction and subjective visual quality were similar between groups, with near vision being the primary reported issue.
The uncorrected and corrected binocular VAs reported at various distances for the Emmetropia group are consistent with those reported in previous studies.10,11,21 The VAs reported for the Monovision group at intermediate and near appear more similar to those obtained with an EDOF IOL of similar design and material.21,22
The binocular defocus curve in the Emmetropia group in the current study was consistent with, though slightly better than, the same curves reported in several prior studies; the latter studies demonstrated significant improvements in intermediate VA relative to a monofocal IOL.11,21–23 The Monovision group in the current study had a defocus curve more similar to the EDOF lens included in those prior studies.21,22 Furthermore, the differences in the defocus curves between the Monovision and Emmetropia groups in the current study were similar to the differences in the defocus curves of the same enhanced monofocal IOL (targeted for emmetropia) and the comparative EDOF IOL in those studies.
Subjective responses indicated that the frequency and degree of bother associated with various visual disturbances was low overall, and not significantly different between groups. This appears consistent with reports from prior studies, though direct comparisons can be problematic when different questionnaires are used. In general, the frequency and severity of visual disturbances appear much lower than have been reported for various EDOF IOLs.24,25
One of the most common functional vision complaints from subjects was the inability to read without reading glasses, with about 20% of subjects indicating this was a limitation in the various questionnaires. While this result is as expected for an enhanced monofocal IOL, it appears that it may not have been sufficiently well understood before surgery. This highlights the importance of patient counseling regarding IOL options before surgery.
One limitation of the study is that it considers results after 3 months, so no comment can be made about longer-term outcomes. Another was the sample size. While sample size was calculated for reliably comparing binocular distance-corrected visual acuity (a parametric variable), the group size may have been insufficient to determine the statistical significance of differences in categorical variables, such as questionnaire responses.
One additional finding in our results was that the likelihood of achieving the targeted level of myopia appeared slightly lower than the likelihood of achieving emmetropia. Further research showed that this has been observed in other studies in the past, and there are suggested strategies to improve results.26
Conclusion
The results of the current study show that the enhanced monofocal IOL here can be used effectively in a monovision modality to improve the intermediate vision provided by the lens when implanted for bilateral emmetropia, with no appreciable change in visual quality. The improved intermediate vision, along with lower levels of visual disturbances associated with use of this enhanced monofocal IOL relative to an EDOF IOL, suggests monovision with the enhanced monofocal may be a viable alternative to bilateral EDOF IOL implantation targeted for emmetropia.
Funding
The study was supported by an investigator-initiated study grant from Johnson & Johnson Surgical Vision, Santa Ana, USA.
Disclosure
Richard Potvin is a consultant to Alcon and Hoya. Kerry D. Solomon is a consultant for Alcon Laboratories, Allergan, Aquesys, Bausch and Lomb, Clarvista Medical, Glaukos, Icon Bioscience, Imprimis, Integrity Digital Solutions, Johnson & Johnson Vision, Kala Pharmaceuticals, Lenstec, Mati Therapeutics, Octane Visionary VC Fund, Ocuhub, Omeros Corporation, Pogotec, PRN, Rayner, Tearlab, Versuant. The authors report no other conflicts of interest in this work.
References
1. Zamora-de La Cruz D, Bartlett J, Gutierrez M, Ng SM. Trifocal intraocular lenses versus bifocal intraocular lenses after cataract extraction among participants with presbyopia. Cochrane Database Syst Rev. 2023;1(1):CD012648. doi:10.1002/14651858.CD012648.pub3
2. Cho JY, Won YK, Park J, et al. Visual Outcomes and Optical Quality of Accommodative, Multifocal, Extended Depth-of-Focus, and Monofocal Intraocular Lenses in Presbyopia-Correcting Cataract Surgery: a Systematic Review and Bayesian Network Meta-analysis. JAMA Ophthalmol. 2022;140(11):1045–1053. doi:10.1001/jamaophthalmol.2022.3667
3. Rampat R, Gatinel D. Multifocal and Extended Depth-of-Focus Intraocular Lenses in 2020. Ophthalmology. 2021;128(11):e164–e185. doi:10.1016/j.ophtha.2020.09.026
4. Melvani R, Farid M. The evidence of implanting a different intraocular lens in each eye. Curr Opin Ophthalmol. 2023;34(1):36–40. doi:10.1097/ICU.0000000000000921
5. Kelava L, Barić H, Bušić M, Čima I, Trkulja V. Monovision Versus Multifocality for Presbyopia: systematic Review and Meta-Analysis of Randomized Controlled Trials. Adv Ther. 2017;34(8):1815–1839. doi:10.1007/s12325-017-0579-7
6. de Silva SR, Evans JR, Kirthi V, Ziaei M, Leyland M. Multifocal versus monofocal intraocular lenses after cataract extraction. Cochrane Database Syst Rev. 2016;12(12):CD003169. doi:10.1002/14651858.CD003169.pub4
7. Lwowski C, Pawlowicz K, Petermann K, et al. Visual and patient-reported factors leading to satisfaction after implantation of diffractive extended depth-of-focus and trifocal intraocular lenses. J Cataract Refract Surg. 2022;48:421–428. doi:10.1097/j.jcrs.0000000000000780
8. Mester U, Vaterrodt T, Goes F, et al. Impact of personality characteristics on patient satisfaction after multifocal intraocular lens implantation: results from the “happy patient study”. J Refract Surg. 2014;30:674–678. doi:10.3928/1081597X-20140903-05
9. Rudalevicius P, Lekaviciene R, Auffarth GU, Liutkeviciene R, Jasinskas V. Relations between patient personality and patients’ dissatisfaction after multifocal intraocular lens implantation: clinical study based on the five factor inventory personality evaluation. Eye. 2020;34(4):717–724. doi:10.1038/s41433-019-0585-x
10. Auffarth GU, Gerl M, Tsai L, et al. Quantum Study Group. Clinical evaluation of a new monofocal IOL with enhanced intermediate function in patients with cataract. J Cataract Refract Surg. 2021;47(2):184–191. doi:10.1097/j.jcrs.0000000000000399
11. Mencucci R, Cennamo M, Venturi D, Vignapiano R, Favuzza E. Visual outcome, optical quality, and patient satisfaction with a new monofocal IOL, enhanced for intermediate vision: preliminary results. J Cataract Refract Surg. 2020;46(3):378–387. doi:10.1097/j.jcrs.0000000000000061
12. Wan KH, Ack A, Kua WN, et al. Enhanced Monofocal Versus Conventional Monofocal Intraocular Lens in Cataract Surgery: a Meta-analysis. J Refract Surg. 2022;38(8):538–546. doi:10.3928/1081597X-20220707-01
13. Steinmüller LN, Greve D, Rua Amaro D, Bertelmann E, von Sonnleithner C. Analysis of higher-order aberrations in relation to the clinical outcome of an enhanced monofocal IOL. Eur J Ophthalmol. 2022;22:11206721221134171. doi:10.1177/11206721221134171
14. Garzón N, Poyales F, Albarrán-Diego C, Rico-Del-Viejo L, Pérez-Sanz L, García-Montero M. Visual and optical quality of enhanced intermediate monofocal versus standard monofocal intraocular lens. Graefes Arch Clin Exp Ophthalmol. 2022;260(11):3617–3625. doi:10.1007/s00417-022-05700-y
15. Abdelrazek Hafez T, Helaly HA. Spectacle Independence And Patient Satisfaction With Pseudophakic Mini-Monovision Using Aberration-Free Intraocular Lens. Clin Ophthalmol. 2019;13:2111–2117. doi:10.2147/OPTH.S215229
16. Goldberg DG, Goldberg MH, Shah R, Meagher JN, Ailani H. Pseudophakic mini-monovision: high patient satisfaction, reduced spectacle dependence, and low cost. BMC Ophthalmol. 2018;18(1):293. doi:10.1186/s12886-018-0963-3
17. Greenstein S, Pineda R. The Quest for Spectacle Independence: a Comparison of Multifocal Intraocular Lens Implants and Pseudophakic Monovision for Patients with Presbyopia. Semin Ophthalmol. 2017;32(1):111–115. doi:10.1080/08820538.2016.1228400
18. Jandewerth T, Biller M, Kohnen T. Intolerance of a non-diffractive extended-depth-of-focus IOL with mini-monovision. Am J Ophthalmol Case Rep. 2022;29:101770. doi:10.1016/j.ajoc.2022.101770
19. Solomon KD, Sandoval HP, Potvin R. Visual outcomes, satisfaction and spectacle Independence with a non-diffractive extended vision intraocular lens targeted for slight monovision. J Cataract Refract Surg. 2023;49(7):686–690. doi:10.1097/j.jcrs.0000000000001191
20. Morlock R, Wirth RJ, Tally SR, Garufis C, Heichel CWD. Patient-Reported Spectacle Independence Questionnaire (PRSIQ): development and Validation. Am J Ophthalmol. 2017;178:101–114. doi:10.1016/j.ajo.2017.03.018
21. Corbelli E, Iuliano L, Bandello F, Fasce F. Comparative analysis of visual outcome with 3 intraocular lenses: monofocal, enhanced monofocal, and extended depth of focus. J Cataract Refract Surg. 2022;48(1):67–74. doi:10.1097/j.jcrs.0000000000000706
22. Lee JH, Moon SY, Chung HS, et al. Clinical outcomes of a monofocal intraocular lens with enhanced intermediate function compared with an extended depth-of-focus intraocular lens. J Cataract Refract Surg. 2022;48(1):61–66. doi:10.1097/j.jcrs.0000000000000710
23. Nanavaty MA, Ashena Z, Gallagher S, Borkum S, Frattaroli P, Barbon E. Visual Acuity, Wavefront Aberrations, and Defocus Curves With an Enhanced Monofocal and a Monofocal Intraocular Lens: a Prospective, Randomized Study. J Refract Surg. 2022;38(1):10–20. doi:10.3928/1081597X-20211109-02
24. Newsom TH, Potvin R. Evaluation of Quality of Vision and Visual Outcomes with Bilateral Implantation of a Non-Diffractive Extended Vision Intraocular Lens with a Target of Slight Myopia in the Non-Dominant Eye. Clin Ophthalmol. 2022;16:183–190. doi:10.2147/OPTH.S350850
25. Reinhard T, Maier P, Böhringer D, et al. Comparison of two extended depth of focus intraocular lenses with a monofocal lens: a multi-centre randomised trial. Graefes Arch Clin Exp Ophthalmol. 2021;259(2):431–442. doi:10.1007/s00417-020-04868-5
26. Turnbull AMJ, Hill WE, Barrett GD. Accuracy of intraocular lens power calculation methods when targeting low myopia in monovision. J Cataract Refract Surg. 2020;46(6):862–866. doi:10.1097/j.jcrs.0000000000000187
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.