Back to Journals » Infection and Drug Resistance » Volume 12
Comparative study of antimicrobial resistance and biofilm formation among Gram-positive uropathogens isolated from community-acquired urinary tract infections and catheter-associated urinary tract infections
Authors Shrestha LB , Baral R , Khanal B
Received 9 January 2019
Accepted for publication 18 February 2019
Published 23 April 2019 Volume 2019:12 Pages 957—963
DOI https://doi.org/10.2147/IDR.S200988
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Sahil Khanna
Lok Bahadur Shrestha, Ratna Baral, Basudha Khanal
Department of Microbiology & Infectious Diseases, B.P. Koirala Institute of Health Sciences, Dharan, Sunsari 56700, Nepal
Background: Gram-positive cocci have emerged to be an important cause of urinary tract infection (UTI) both in community-acquired UTI (Com-UTI) and catheter-associated urinary tract infection (CA-UTI). The objective of this study was to investigate the frequency of Gram-positive cocci urinary tract infections, their susceptibility patterns to commonly used antimicrobial agents and the biofilm forming property with respect to catheter-associated UTI and community-acquired UTI.
Methods: A total of 1,360 urine samples from indwelling catheter and 10,423 from mid-stream urine were obtained during a 6-month period and processed following standard microbiological guidelines. Biofilm formation was detected using congo red agar (CRA), tube method (TM) and tissue culture plate (TCP) method. Chi-square test and independent sample t-test were employed to calculate the significance. Statistical significance was set at P-value ≤0.05.
Results: The infection rate was significantly higher in CA-UTI as compared to Com-UTI (25% vs 18%, p=0.0001). Among 2,216 organisms isolated, 471 were Gram-positive cocci; 401 were obtained from Com-UTI while 70 were from CA-UTI. Enterococcus faecalis was the most common organism isolated from Com-UTI, while Staphylococcus aureus was commonest among CA-UTI. Multi-drug resistance, methicillin-resistant Staphylococcus aureus and vancomycin-resistant Enterococci were also significantly higher in CA-UTI as compared to Com-UTI. Biofilm-forming property was significantly higher in CA-UTI than Com-UTI. The sensitivity of congo red agar method and tube method was 79% and 81.9% respectively and specificity was 98.5% each. Antimicrobial resistance was significantly higher in biofilm-formers as compared to non-formers.
Conclusion: Gram-positive bacteria are a significant cause of both CA-UTI and Com-UTI with Enterococcus faecalis and Staphylococcus aureus as common pathogen. Biofilm formation and multi-drug resistance is significantly higher in CA-UTI than Com-UTI. Routine surveillance of antimicrobial resistance and biofilm formation is necessary in all cases of UTI to ensure the proper management of patients.
Keywords: CA-UTI, multi-drug resistant, biofilm, MRSA
Background
Urinary tract infections (UTIs) are the most common infections in both community and hospital settings infections.1 Although Gram-negative bacteria cause the majority of UTI, Gram-positive bacteria have emerged to cause UTI, particularly among individuals who are elderly, pregnant, or who have other risk factors.2,3 Catheter-associated urinary tract infection (CA-UTI) is one of the most common healthcare-acquired infections; 70–80% are attributable to use of an indwelling urethral catheter.4 Gram-positive bacteria like Staphylococcus aureus, Enterococcus faecalis and Enterococcus faecium are responsible for a minority of community-acquired UTI (Com-UTI), but together cause 30–45% of catheter-associated UTIs and are the third leading cause of hospital-acquired UTIs.5 Bacterial biofilms play an important role in UTIs, being responsible for both acute and persistent infections. Biofilm-forming bacteria involved up to 80% of all infections, with urology being one of the main fields in which biofilm can become a serious problem.6 Biofilms can not only develop into urethral stents but they can also form on catheters, causing their blockage. One of the most important concerns of biofilm is the antimicrobial resistance shown by these structures. Biofilm can be up to 1,000-fold more resistant to antibiotics than planktonic cells due to several mechanisms.6,7
The objective of this study was to compare the frequency of Gram-positive cocci urinary infection, their susceptibility patterns to commonly used antimicrobial agents and the biofilm forming property between Com-UTI and CA-UTI.
Methods
Case definition
CA-UTI is defined as an infection in a patient with a urinary catheter meeting the National Healthcare Safety Network definition of UTI.8 Com-UTI is defined as an infection of the urinary tract that occurs in the community or within less than 48 h of hospital admission and was not incubating at the time of hospital admission.9,10 Multi-drug resistance (MDR) is defined as resistance to at least one agent in three or more classes of antimicrobials.11
Study population and bacterial isolates
This is a prospective study carried out at Department of Microbiology, from 1 January 2018 to 30 June 2018. Ethical clearance was obtained from institutional review committee before starting the research. A total of 10,423 clean-catch midstream urine and 1,360 catheter urine samples were collected from the same number of clinically suspected patients of UTI. Once the sample was collected, it was transferred to the laboratory immediately and inoculated on cysteine lactose electrolyte deficient agar using a standard calibrated loop. Isolates from cases with significant bacteriuria (105 colonies/mL) were identified based upon standard microbiological procedures involving morphological characteristics, Gram’s stain, rapid tests (catalase, oxidase, coagulase, bile solubility), and biochemical tests like indole, methyl red, Voges–Proskauer and citrate, triple sugar iron, oxidation/fermentation, urease and nitrate reduction.12
Antimicrobial susceptibility testing
Antimicrobial susceptibility testing was performed on Mueller–Hinton agar using disk diffusion technique according to Clinical and Laboratory Standards Institute (CLSI) guidelines.13 The isolates were tested against the following antimicrobial discs (HiMedia, Mumbai, India): amikacin (10 μg), cephalexin (30 μg), ceftriaxone (30 μg), gentamicin (10 μg), nitrofurantoin (50 μg), cotrimoxazole (25 μg), penicillin (10 μg), ofloxacin (5 μg), vancomycin (30 μg), and linezolid (30 μg).
Minimum inhibitory concentration (MIC)
Resistance to methicillin and vancomycin in S. aureus and vancomycin-resistant Enterococci were confirmed by calculating the MIC of the antibiotics using broth dilution method.14 S. aureus isolates with MIC to vancomycin ≤2 µg/mL was considered susceptible, 4–8 µg/mL intermediate and ≥16 µg/mL resistant. For methicillin-resistant Staphylococcus aureus, MIC to oxacillin ≤2 µg/mL was considered susceptible and ≥4 µg/mL considered resistant. For E. faecalis, MIC to vancomycin ≤4 µg/mL was considered susceptible, 8–16 µg/mL intermediate and ≥32 µg/mL resistant.13,14
Biofilm formation
Biofilm formation was detected by congo red agar (CRA),15 tube method (TM)16 and tissue culture plate (TCP) method.17 The statistical analysis of CRA and TM was done using TCP as the reference method.18,19
Congo red agar method15
This method was proposed by Freeman et al. Congo red agar was prepared by mixing brain heart infusion broth, sucrose, congo red dye and agar (HiMedia) in 1 L distilled water. The organisms were plated on it and incubated aerobically at 37 ºC for 24 h. The observation of black colored colony was considered as biofilm positive and red colored colony as negative.
Tube method16
Test tubes containing trypticase soy broth with 1% glucose (HiMedia) were prepared. Bacterial suspension was inoculated and incubated overnight at 35ºC. After incubation, tubes were decanted and washed properly with phosphate buffer solution of pH 7.3 (HiMedia). Upon drying, the tubes were stained with 0.1% crystal violet (HiMedia) and washed several times with water. Test tubes with uniform stain deposits on the walls were considered positive for biofilm formation.
Tissue culture plate method17
For the TCP method the test organism was inoculated in trypticase soy broth with 1% glucose (HiMedia) and incubated at 35ºC aerobically. Culture (0.2 mL) was added into individual wells of 92-well flat-bottom tissue culture plates; the plate was then incubated for 24 h. The plates were first tapped gently and then cleaned with PBS (pH 7.3) four times. After that, the plate was fixed with sodium acetate (2%) (HiMedia) and stained with 0.1% crystal violet. The wells with uniformly stained floor and walls were considered biofilm formers.
Quality control
Staphylococcus aureus ATCC 25923 and Enterococcus faecalis ATCC 29212 were used for quality control of the biochemical tests, MIC and antimicrobial discs.13 For biofilm formation, S. epidermidis ATCC 35984 was used as positive control and S. epidermidis ATCC 12228 was used as negative control.17
Data analysis
The data were entered in Microsoft Excel 2013 (Microsoft Corporation, Redmond, WA, USA) and interpreted using SPSS version 16 (SPSS Inc., Chicago, IL, USA). Data were expressed in terms of numbers and percentages and analyzed using chi-square test and t-test. P-value <0.05 was considered significant.
Ethical approval and consent
Ethical clearance was obtained from Institutional Review Committee, B. P. Koirala Institute of Health Sciences, before starting the research (code no: IRC/1011/017). Written informed consent was obtained from each patient.
Results
During the study period, a total of 10,423 urine samples from mid-stream urine and 1,360 from indwelling catheter and were obtained. The infection rate was significantly higher in CA-UTI as compared to Com-UTI (n=340, 25% vs n=1876, 18%, p=0.0001) (Table 1). Among 2,216 organisms isolated, 1,745 (78.74%) were Gram-negative bacilli and 471 (21.25%) were Gram-positive cocci (GPC). Among the GPC isolates, 401 were obtained from Com-UTI and 70 from CA-UTI. E. faecalis (n=217, 54.11%) was the most common organism isolated from community-associated UTI, followed by S. aureus (n=157, 39.15%). However, in case of catheter-associated UTI, S. aureus (n=37, 52.85%) was the most common isolate (Table 2).
 | Table 1 Total number of samples and infection rate in Com-UTI and CA-UTI |
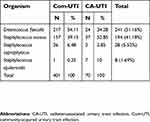 | Table 2 Gram-positive cocci isolated from Com-UTI and CA-UTI |
 | Table 3 comparison of biofilm formation and multi-drug resistance among CA-UTI and Com-UTI |
 | Table 4 Statistical analysis of congo red agar and tube method using tissue culture plate method as gold standard |
 | Table 5 Antimicrobial resistance and comparison between biofilm formers and non-formers, Com-UTI and CA-UTI |
Discussion
The present study demonstrates a significantly high infection rate in catheter-associated urinary tract infection as compared to community-acquired UTI. The infection rate of 25% in CA-UTI is similar to the study done by Dougnon et al in West Africa.20 However, some studies like Zarb et al (17.2%) and Prashamsa et al (12.5%) have suggested a lower incidence of CA-UTI.21,22 Higher incidences of CA-UTI (35.6%) has been reported by Iwuafor et al23. The high infection rate of CA-UTI in our study might be attributed to the fact that this hospital is a tertiary care referral hospital; most patients admitted here usually received treatment elsewhere and might have been catheterized elsewhere as well. Several studies have suggested that the use of indwelling urethral catheters increases the risk of UTI occurrence by up to 14-fold.2,4
In the present study, E. faecalis was the most common Gram-positive coccus isolated from community-acquired UTI while S. aureus was the most common GPC isolated from CA-UTI. The result is in agreement with study done by Lewis et al in South Africa.24 In contrast to our finding, the study done by Baral et al demonstrated S. aureus as the most common Gram-positive bacterium causing Com-UTI.25 Although the study was conducted in the same setup, it was 9 years before and did not differentiate between community-acquired UTI and catheter-associated UTI. A study done by Bardoloi et al concluded that S. aureus was the most common organism isolated both from Com-UTI and CA-UTI.26 S. aureus and E. faecalis are the most common Gram-positive bacteria causing UTI.2 The increased number of enterococcal UTI in this part might be due to the rapid surge in number of diabetic patients; diabetes mellitus is one of the important risk factors of enterococcal UTI.27 The increased incidence of enterococcal UTI is alarming; resistance to most commonly used antimicrobial agents is a typical characteristic of these bacteria. It is far more difficult to treat enterococcal UTI as compared to UTI caused by other bacteria due to intrinsic resistance to many antimicrobials and rapidly increasing acquired resistance.28–30
Antimicrobial resistance was compared between CA-UTI and Com-UTI. A significant rise in resistance to the usually prescribed antimicrobials was noted among patients with CA-UTI compared to those with Com-UTI. Multi-drug resistance was much higher in CA-UTI in comparison with Com-UTI. The finding is similar to the study done by Bardoloi et al in Kerala, India26 and Michno et al in Poland.31 The result suggests that catheterization increases the degree of drug resistance in bacteria. Previous hospitalization, long-term broad-spectrum antimicrobial therapy, co-morbidity, frequent instrumentation, and cross-transmission of pathogens in catheterized patients might explain the higher antimicrobial resistance.23
The present study suggested that incidences of MRSA and VRE were much higher in patients with CAUTI than that of Com-UTI; these results were not different from those published by Mody et al in Michigan32 and Iwuafor et al in Nigeria.23 The higher incidence of MRSA and VRE from patients with catheter-associated UTI might be due to previous antimicrobial therapy, biofilm formation and previous hospitalization in those patients. Catheterization is the most important risk factor for MRSA and VRE associated UTI.33,34
Biofilm formation was noted in 75% of isolates from CA-UTI and 24% of isolates from Com-UTI. Similar results were obtained in the study conducted by Sabir et al35. Discordantly, Bardoiloi et al26 concluded biofilm formation was higher in Com-UTI (76% vs 60%). The higher prevalence of biofilm in catheters is probably due to the survival advantage provided by the catheter to the microorganisms.36 Catheter create an environmental condition on its surface that make it an ideal site for bacterial attachment and formation of biofilm structures.6
Even though the principle of CRA, TM and TCP method is the same, which is based on the enhancement of exopolysaccharide production using enriched media (TSB with glucose/sucrose), they detect biofilm with variable sensitivity.37 The sensitivity of TM was slightly higher than CRA for the detection of biofilm; the finding is similar to several other studies.38,39 However, some studies also suggest that CRA is superior to TM in detection of biofilm formation.40,41 The results of our finding gave us enough evidence that these phenotypic methods can be used routinely for the detection of biofilm formation. Even though tissue culture plate method is considered as the gold standard for the detection of biofilm formation, congo red agar and tube method are easy, inexpensive and reliable method for the detection of biofilm formation.18,38,40
The antimicrobial resistance pattern, when compared with respect to their biofilm forming property, showed significant differences. The level of resistance to antibiotics was higher in biofilm formers than non-formers. The results are consistent with findings of Bardoloi et al,26 Shrestha et al38 and Soumya et al42. This might be due to the fact that biofilm makes it notoriously difficult for the antibiotics to penetrate them and act upon the microorganisms. Similarly, biofilm also protects the organism from being swept away by shear forces and phagocytosis.36 Hence, detection of biofilm production by uropathogens is crucial, and it can help in initiating the appropriate intervention, especially in cases of symptomatic UTI.43
The limitation of our research includes the inability to follow up catheterized patients to collect history of prior hospital admissions, intake of antimicrobials, type of catheter used and clinical outcome.
Conclusion
Gram-positive bacteria are a significant cause of both CA-UTI and Com-UTI with Enterococcus faecalis and Staphylococcus aureus as common pathogen. The most worrisome finding is the high prevalence of multidrug resistant uropathogens. Biofilm formation and multi-drug resistance is significantly higher in CAUTI than Com-UTI. Since the management of UTI with biofilm-forming bacteria is different and difficult, routine surveillance of biofilm formation and antimicrobial resistance is necessary in all cases of UTI to ensure the optimum management of patient and for epidemiological surveillance.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Stefaniuk E, Suchocka U, Bosacka K, Hryniewicz W. Etiology and antibiotic susceptibility of bacterial pathogens responsible for community-acquired urinary tract infections in Poland. Eur J Clin Microbiol Infect Dis. 2016;35(8):1363–1369. [PMC ID: PMC4947106]. doi:10.1007/s10096-016-2673-1
2. Kline KA, Lewis AL. Gram-positive uropathogens, polymicrobial urinary tract infection, and the emerging microbiota of the urinary tract. Microbiol Spectr. 2016;4(2). [PMC ID: 4888879]. doi:10.1128/microbiolspec.UTI-0012-2012
3. Hooton TM. Clinical practice. Uncomplicated urinary tract infection. N Engl J Med. 2012;366(11):1028–1037. doi:10.1056/NEJMcp1104429
4. Nicolle LE. Catheter associated urinary tract infections. Antimicrob Resist Infect Control. 2014;3:23. [4114799]. doi:10.1186/2047-2994-3-23
5. Maki DG, Tambyah PA. Engineering out the risk for infection with urinary catheters. Emerg Infect Dis. 2001;7(2):342–347. [PMC ID: 2631699]. doi:10.3201/eid0702.700342
6. Soto SM. Importance of biofilms in urinary tract infections: new therapeutic approaches. Adv Biol. 2014;2014:13. doi:10.1155/2014/543974
7. Mack D, Becker P, Chatterjee I, et al. Mechanisms of biofilm formation in Staphylococcus epidermidis and Staphylococcus aureus: functional molecules, regulatory circuits, and adaptive responses. Int J Med Microbiol. 2004;294(2–3):203–212. doi:10.1016/j.ijmm.2004.06.015
8. Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control. 2008;36(5):309–332. doi:10.1016/j.ajic.2008.03.002
9. Kabugo D, Kizito S, Ashok DD, et al. Factors associated with community-acquired urinary tract infections among adults attending assessment centre, Mulago Hospital Uganda. Afr Health Sci. 2016;16(4):1131–1142. [5398460]. doi:10.4314/ahs.v16i4.31
10. Moyo SJ, Aboud S, Kasubi M, Lyamuya EF, Maselle SY. Antimicrobial resistance among producers and non-producers of extended spectrum beta-lactamases in urinary isolates at a tertiary Hospital in Tanzania. BMC Res Notes. 2010;3:348. [3017072]. doi:10.1186/1756-0500-3-348
11. Magiorakos AP, Srinivasan A, Carey RB, et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012;18(3):268–281. doi:10.1111/j.1469-0691.2011.03570.x
12. Winn W, Allen S, Janda W, et al. Koneman’s Color Atlas and Textbook of Diagnostic Microbiology.
13.
14.
15. Freeman DJ, Falkiner FR, Keane CT. New method for detecting slime production by coagulase negative staphylococci. J Clin Pathol. 1989;42(8):872–874. [1142068].
16. Christensen GD, Simpson WA, Bisno AL, Beachey EH. Adherence of slime-producing strains of Staphylococcus epidermidis to smooth surfaces. Infect Immun. 1982;37(1):318–326. [347529].
17. Christensen GD, Simpson WA, Younger JJ, et al. Adherence of coagulase-negative staphylococci to plastic tissue culture plates: a quantitative model for the adherence of staphylococci to medical devices. J Clin Microbiol. 1985;22(6):996–1006. [271866].
18. Mathur T, Singhal S, Khan S, Upadhyay DJ, Fatma T, Rattan A. Detection of biofilm formation among the clinical isolates of Staphylococci: an evaluation of three different screening methods. Indian J Med Microbiol. 2006;24(1):25–29. [PMID: 16505551].
19. Jain A, Agarwal A. Biofilm production, a marker of pathogenic potential of colonizing and commensal staphylococci. J Microbiol Methods. 2009;76(1):88–92. doi:10.1016/j.mimet.2008.09.017
20. Dougnon TV, Bankole HS, Johnson RC, et al. Catheter-associated urinary tract infections at a hospital in Zinvie, Benin (West Africa). Int J Infect. 2016;3(2). doi:10.17795/iji-34141
21. Prashamsa K, Devi D, Madhup SK, Shrechand JB. Catheter associated urinary tract infection: prevalence, microbiological profile and antibiogram at a tertiary care hospital. Acclm. 2017;3(2):3–10.
22. Zarb P, Coignard B, Griskeviciene J, et al. The European Centre for Disease Prevention and Control (ECDC) pilot point prevalence survey of healthcare-associated infections and antimicrobial use. Euro Surveill. 2012;17(46). doi:10.2807/ese.17.46.20316-en
23. Iwuafor AA, Ogunsola FT, Oladele RO, et al. Incidence, clinical outcome and risk factors of intensive care unit infections in the Lagos University Teaching Hospital (LUTH), Lagos, Nigeria. PLoS One. 2016;11(10):e0165242. [5077115]. doi:10.1371/journal.pone.0165242
24. Lewis DA, Gumede LY, van der Hoven LA, et al. Antimicrobial susceptibility of organisms causing community-acquired urinary tract infections in Gauteng Province, South Africa. S Afr Med J. 2013;103(6):377–381. doi:10.7196/samj.6722
25. Baral R, Timilsina S, Jha P, et al. Study of antimicrobial susceptibility pattern of Gram positive organisms causing UTI in a tertiary care hospital in eastern region of Nepal. Health Renaissance. 2013;11(2):119–124. doi:10.3126/hren.v11i2.8218
26. Bardoloi V, Yogeesha Babu KV. Comparative study of isolates from community-acquired and catheter-associated urinary tract infections with reference to biofilm-producing property, antibiotic sensitivity and multi-drug resistance. J Med Microbiol. 2017;66(7):927–936. doi:10.1099/jmm.0.000525
27. Nitzan O, Elias M, Chazan B, Saliba W. Urinary tract infections in patients with type 2 diabetes mellitus: review of prevalence, diagnosis, and management. Diabetes Metab Syndr Obes. 2015;8:129–136. [4346284]. doi:10.2147/DMSO.S51792
28. Wisell KT, Kahlmeter G, Giske CG. Trimethoprim and enterococci in urinary tract infections: new perspectives on an old issue. J Antimicrob Chemother. 2008;62(1):35–40. doi:10.1093/jac/dkn147
29. Moellering RC
30. Tacconelli E, Cataldo MA. Vancomycin-resistant enterococci (VRE): transmission and control. Int J Antimicrob Agents. 2008;31(2):99–106. doi:10.1016/j.ijantimicag.2007.08.026
31. Michno M, Sydor A, Walaszek M, Microbiology SW. Drug resistance of pathogens in patients hospitalized at the nephrology department in the South of Poland. Pol J Microbiol. 2018;67(4):517–524. doi:10.21307/pjm-2018-061
32. Mody L, Maheshwari S, Galecki A, Kauffman CA, Bradley SF. Indwelling device use and antibiotic resistance in nursing homes: identifying a high-risk group. J Am Geriatr Soc. 2007;55(12):1921–1926. [3319402]. doi:10.1111/j.1532-5415.2007.01468.x
33. Walker JN, Flores-Mireles AL, Pinkner CL, et al. Catheterization alters bladder ecology to potentiate Staphylococcus aureus infection of the urinary tract. Proc Natl Acad Sci U S A. 2017;114(41):E8721–E8730. [5642702]. doi:10.1073/pnas.1707572114
34. Padmavathy K, Praveen S, Madhavan R, Krithika N, Kiruthiga A. Clinico-microbiological investigation of catheter associated urinary tract infection by enterococcus faecalis: vanA Genotype. J Clin Diagn Res. 2015;9(8):DD05–6. [4576540]. doi:10.7860/JCDR/2015/13856.6378
35. Sabir N, Ikram A, Zaman G, et al. Bacterial biofilm-based catheter-associated urinary tract infections: causative pathogens and antibiotic resistance. Am J Infect Control. 2017;45(10):1101–1105. doi:10.1016/j.ajic.2017.05.009
36. Trautner BW, Darouiche RO. Role of biofilm in catheter-associated urinary tract infection. Am J Infect Control. 2004;32(3):177–183. [2963581]. doi:10.1016/j.ajic.2003.08.005
37. Onawunmi GO. Antibiotic resistance profiles of biofilm-forming bacteria associated with urine and urinary catheters in a tertiary hospital in Ile-Ife, Nigeria AU - Osungunna, Michael O. S Afr J Infect Dis. 2018;33(3):80–85.
38. Shrestha LB, Bhattarai NR, Khanal B. Comparative evaluation of methods for the detection of biofilm formation in coagulase-negative staphylococci and correlation with antibiogram. Infect Drug Resist. 2018;11:607–613. [5926075]. doi:10.2147/IDR.S159764
39. Oliveira A, Cunha Mde L. Comparison of methods for the detection of biofilm production in coagulase-negative staphylococci. BMC Res Notes. 2010;3:260. [2973941]. doi:10.1186/1756-0500-3-260
40. Shrestha LB, Bhattarai NR, Khanal B. Antibiotic resistance and biofilm formation among coagulase-negative staphylococci isolated from clinical samples at a tertiary care hospital of eastern Nepal. Antimicrob Resist Infect Control. 2017;6:89. [5579930]. doi:10.1186/s13756-017-0251-7
41. Saising J, Singdam S, Ongsakul M, Voravuthikunchai SP. Lipase, protease, and biofilm as the major virulence factors in staphylococci isolated from acne lesions. Biosci Trends. 2012;6(4):160–164.
42. Soumya KR, Philip S, Sugathan S, Mathew J, Radhakrishnan EK. Virulence factors associated with Coagulase Negative Staphylococci isolated from human infections. 3 Biotech. 2017;7(2):140. [PMC ID: PMC5462657]. doi:10.1007/s13205-017-0753-2
43. Panda PS, Chaudhary U, Dube SK. Comparison of four different methods for detection of biofilm formation by uropathogens. Indian J Pathol Microbiol. 2016;59(2):177–179. doi:10.4103/0377-4929.182013
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
