Back to Journals » Journal of Pain Research » Volume 15
Comparative Study Between the Mini-Open (≤2.5 Cm) Approach and Conventional Open Lateral Approach in the Surgical Treatment of Radial Head Fractures
Authors Zhou X , Wang B, Liu Y , Wang Z, Zhao X, Liu F, Lu S, Xu W, Li L, Dong J
Received 24 May 2022
Accepted for publication 18 October 2022
Published 26 October 2022 Volume 2022:15 Pages 3413—3422
DOI https://doi.org/10.2147/JPR.S374599
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor E Alfonso Romero-Sandoval
Xiaofeng Zhou,1 Bingzhi Wang,2 Yu Liu,1 Zicheng Wang,2 Xuehui Zhao,2 Fanxiao Liu,2 Shun Lu,2 Weicheng Xu,2 Lianxin Li,1,2 Jinlei Dong2
1Department of Orthopaedics Surgery, Shandong Provincial Hospital, Shandong University, Jinan, People’s Republic of China; 2Department of Orthopaedics Surgery, Shandong Provincial Hospital Affiliated to Shandong First Medical University, Jinan, People’s Republic of China
Correspondence: Lianxin Li, Department of Orthopaedics, Shandong Provincial Hospital, Shandong University, Jinan, Shandong, 250021, People’s Republic of China, Tel +8613505312449, Email [email protected] Jinlei Dong, Department of Orthopaedics, Shandong Provincial Hospital affiliated to Shandong First Medical University, Jinan, Shandong, 250021, People’s Republic of China, Tel +861509874540, Email [email protected]
Purpose: The conventional lateral approach is widely used to treat radial head fractures with screws. However, the traditional incision may have shortcomings, including excessive exposure and significant scarring. We propose an innovative method – a mini-open lateral approach of less than 2.5 cm for surgical treatment of radial head fractures with screws.
Methods: From Jan 2017 to Dec 2020, 34 patients diagnosed with closed radial head fracture were treated with open reduction and internal fixation (ORIF) in this study. The novel group (mini-open group) included 15 patients, and the other 19 patients were in the traditional group. The time of operation and the blood loss during operation were recorded. Postoperative clinical outcomes and radiographic results were recorded and compared between the two groups. The range of motion (ROM) in the elbow, the Visual Analogue Scale (VAS), the Mayo Elbow Performance Score (MEPS), Rating Scale of the American Shoulder and Elbow Surgeons (ASES), and the Shortened Disabilities of the Arm, Shoulder and Hand Questionnaire (Q-DASH) score and complications, such as wound infection, vascular and nerve damage, and fragment redisplacement were observed in the two groups.
Results: In the comparison between the two groups, there was no significant difference in age, sex, cause of radial head fracture, or other basic information. The operation time, intraoperative blood loss, and VAS score at 3 days postoperation were significantly reduced in the novel group (p < 0.05). The follow-up results showed that there was no significant difference in MEPS, ASES, or Q-DASH scores between the two groups.
Conclusion: The mini-open approach reduced intraoperative blood loss, shortened operation time, relieved patient pain, and achieved a satisfactory postoperative clinical result, which demonstrates that the novel approach is a safe and effective option for treating radial head fractures.
Keywords: radial head, mini-open, fracture, screw, clinical efficacy
Introduction
Radial head fracture is one of the most common injuries in the human body, accounting for one-third of all elbow fractures.1–3 Mason first reported radial head fractures and proposed the initial classification in 1945,3 which was modified in 1986.4 It is well evidenced that radial head fractures with a nondisplacement of < 2 mm (type I) can be treated nonoperatively with good results. Open reduction and internal fixation (ORIF) is the most common treatment choice for radial fractures.5
Commonly used internal fixations include screws, plates, Kirschner wires, and biodegradable screws.6 A previous study reported that K-wire cannot compress the fracture line, which may result in migration of the fracture.7 The plate is usually considered to be bulky and leads to annular ligament injury.8 Screws are the most commonly used fixation because of the advantages of less damage to soft tissue and firm fixation.9
Interest in the minimally invasive surgical treatment of radial head fracture in this context seems to have increased in the literature. Many scholars have argued that minimally invasive surgery significantly reduces blood loss and shortens operative time.10–12 Gao et al reported a minimally invasive method of closed reduction using titanium elastic nails.13 Jia et al also studied this method and improved it.14 Wang et al described the excellent result of arthroscopic fixation using Kirschner wires.15 Hence, the best surgical method for the treatment of radial head fractures remains controversial.
Traditionally, ORIF using screws requires an incision from the lateral epicondyle to the proximal part of the radius along the mid axial line.5,16 This method is suitable for all types of radial head fractures. However, the traditional incision may have some shortcomings, including excessive exposure and significant scarring. It could cause additional pain and psychological burden to the patient.17–20 Therefore, we propose an innovative method - a mini-open lateral approach of less than 2.5 cm for surgical treatment of radial head fractures with screws. The purposes of this study are to (1) offer an idea that radial head fracture can be exposed through a minimally invasive approach based on the Kocher approach or the Kaplan approach; (2) demonstrate that this approach supports anatomical reduction under direct vision and results in fewer complications related to surgery; and (3) describe the operation methods and the clinical utility of this approach and evaluate the safety, efficacy, and benefits through radiographic, clinical, and functional outcome data on patients with radial head fractures.
Materials and Methods
Inclusion and Exclusion Criteria
The inclusion criteria in this retrospective study were as follows: (i) patients diagnosed with fracture of the radial head by X-ray; (ii) patients who underwent ORIF with screws; (iii) patients with a follow-up of more than 6 months.
The exclusion criteria were as follows: (i) patients younger than 16 years. (ii) any other injuries around the elbow except fracture of the radial head; (iii) time from injury to operation of more than 3 weeks; (iv) open fracture; (v) mason type I or non-operation (Figure 1)
 |
Figure 1 Exclusion criteria. |
Surgical Technique
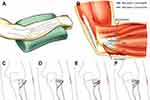
Patients were placed in the supine position with their injured limb in 90° of abduction and elbow joint in 90° flexion. The location of the radial head was determined according to the body-surface markers and drawn with a marker pen (Figure 2A). A Kirschner wire was placed parallel to the brachioradialis joint on the lateral side to confirm its placement using fluoroscopy (Figure 2B). A vertical line of approximately 2.5 cm was made across the k-wire, which was the surgical incision. The radial long carpal extensor and radial short carpal extensor muscles were visible anteriorly in the incision, and the elbow muscles were visible posteriorly after separating the subcutaneous tissue. The deep radial nerve branch was kept away from the operative field by rotating the forearm forward. The joint capsule was incised along the incision to create a precise exposure of the fracture. Reduction of the fracture was performed by leveraging the K-wire and probe. Screws were inserted into the radial head after satisfactory reduction (Figure 2C). The incision is approximately 2.5 cm in length (Figure 2D). Different screw fixation methods were used for the fixation of different types of fractures (Figure 3). A K-wire was used to predrill a hole to prevent the bone block from breaking before drilling the screws. The screw can be replaced by a K-wire when the bone mass is quite small. For Mason III fractures with two large and stable bone masses, screws are used to turn two bone blocks into one. X-ray imaging was used to verify fracture fixation refinement.
Postoperative Management
All patients were bandaged with light dressings after operation. Ice compressions were applied for swelling at least 2 days. All patients were given non-steroidal anti-inflammatory and analgesic drugs (NSAIDs) to relieve acute pain and prevent heterotopic ossification (HO).21 Each of them was encouraged to perform passive flexion, extension, and rotation exercises on the injured limb 1 day after surgery, with no restrictions on the rest of the limbs. Active functional exercise was started at 3 weeks, and unrestricted activity was observed after fracture healing at 3 months after surgery. The first follow-up was usually two weeks after discharge from the hospital and included only clinical evaluation. Radiographic evaluation was also performed after one and two months, unless any complications occurred sooner.
Evaluation Criteria of the Clinical Effectiveness
The interval between injury and surgery, operative time, blood loss, length of hospital stay, and operative complications were collected and reviewed. The Visual Analogue Scale (VAS) score at 3 days postoperation was used to evaluate the pain difference between the two groups. Patients were evaluated by the same surgeon at each of the follow-up visits, where the range of motion (ROM) in the elbow, the VAS, the Mayo Elbow Performance Score (MEPS), Rating Scale of the American Shoulder and Elbow Surgeons (ASES), and the Shortened Disabilities of the Arm, Shoulder and Hand Questionnaire (Q-DASH) score were recorded.
Statistical Analysis
All results were evaluated using SPSS 25.0 for Windows (IBM, USA). Differences in patient characteristics between the two approaches, such as sex, mechanism of injury, and fracture classification, were compared along with clinical and radiographic outcomes using Fisher’s exact test. Patient age, blood loss, and surgery time were compared using Student’s t test. Complications were assessed using Fisher’s exact test, including the rates of nerve injury, stiff elbow, and fracture nonunion. A p value of less than 0.05 was considered significant.
Results
From Jan 2017 to Dec 2020, a total of 34 patients with closed radial head fractures underwent ORIF using screws in our department. The mechanisms of injury were fall injuries in 31 cases, and traffic accidents in 3 cases. The demographics of the patients in the two groups are shown in Table 1. All patients were followed up for at least 1 year without death or loss to follow-up. The mean age of patients was 30.13 years (range 16 to 55 years) in the novel group, with a male/female ratio of 9:6. The mean age of patients was 30.79 years (range 19 to 48 years) in the conventional group, with a similar male/female ratio as the novel group. The mini-open approach was used in 15 patients, and the traditional lateral approach was used in 19 patients. The mini-open population was composed of 11 Mason II and 4 Mason III fractures, while the traditional population was composed of 11 Mason II and 8 Mason III fractures. There were no significant differences between the two groups in terms of mean age, gender composition, or type of fracture between the two surgical approaches.
 |
Table 1 Demographics of Patients Between the Two Groups |
Operative Records
The operative time for the novel group was 66.20 ± 11.74 min, with intraoperative blood loss of 18.70 ± 11.25 mL. The operative time for the conventional group was 87.58 ± 32.02 min, with intraoperative blood loss of 35.79 ± 17.10 mL. There were significant differences in blood loss (p =0.002) and operative time (p =0.020) between the approaches. The hospital stays were 5.13 ± 1.60 days in the novel group and 6.26 ± 2.13 days in the conventional group, with no significant difference (p > 0.05). The VAS score at 3 days postoperation was 3.20 ± 0.68 in the novel group and 3.89 ± 9.34 in the conventional group (p =0.022; Table 2).
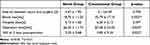 |
Table 2 The Operative Records and Statistical Analysis Between the Two Groups |
Functional Assessment
The mean elbow ROM for the novel group was 139.50° ± 3.44 for flexion-extension, 86.87° ± 3.11 for pronation, and 86.47° ± 3.13 for supination, whereas the mean ROM for the conventional group was 139.53° ± 3.36 for flexion-extension, 87.05° ± 2.68 for pronation, and 87.37° ± 2.65 for supination (Figure 4).
The mean MEPS scores were 96.33 ± 3.99 points in the novel group and 93.68 ± 5.74 points in the conventional group (p = 0.138). The mean ASES scores were 13.80 ± 0.41 in the novel group and 13.89 ± 0.32 points in the conventional group (p = 0.454). The mean Q-DASH scores were 0.60 ± 1.40 points in the novel group and 0.84±1.95 points in the conventional group (p = 0.689). Comparing the ROM, ASES, MEPS, and Q-DASH scores between the two groups, no significant differences were observed (Table 3).
 |
Table 3 The ROM and Clinical Scores at 6 Months Postoperation |
Complications
All surgical incisions healed without complications, such as wound infection, vascular damage, nerve damage, and fragment redisplacement, and all patients had radiographic union at the 3-month follow-up. Only 2 patients underwent removal of the internal fixation at 12 and 14 months postoperatively, and the remaining patients did not undergo secondary surgery. All patients achieved good clinical and radiological results, with no nonunion or delayed fracture healing and no elbow pain, joint stiffness, heterotopic ossification, or posttraumatic arthritis until the last follow-up (Figure 5).
Discussion
Compared with the traditional lateral approach, the mini-open approach for radius fractures can significantly reduce intraoperative bleeding, shorten the operative time, and relieve patient pain, with satisfactory postoperative function.
At present, ORIF has been recommended for radial head fractures above Mason type II.22–24 For this type of fracture, the conventional surgical approaches include the Kocher approach and the Kaplan approach.25 The advantage of those approaches is reduction under direct vision, which can achieve a complete anatomical reduction of the radial head and maximize the restoration of elbow joint function. Anatomical reduction of fracture is critical for optimal long-term outcomes and prevention of postoperative complications.26 However, there are several disadvantages to those approaches, including possible excessive tissue damage. Both approaches require a sizeable lateral incision, which leads to excessive damage and reduces the blood supply to the fracture site. It can also result in tissue damage and intraarticular haematoma formation, which increases the risk of elbow stiffness, heterotopic ossification, nerve injury, and other complications.27
The plate and the screw are commonly used in the treatment of radius fractures. T. C. Koslowsky et al compared four different fixations for Mason type III fractures in a cadaver study of 96 cases and found that the Fragment Fixation System (FFS) provided a better quality of reduction than others and that there was significantly better stability when using FFS implants, mini-screws, and K-wires than when using mini plates.28 A similar test was performed in cadavers and indicated that cross-cannulated screws were superior to conventional T-plates.29 Another study demonstrated that the stiffness of the screw and plate are similar in all planes, even though the stiffness of the screw was 1.8 times that of the plate from medial to lateral.30 Iacobellis C et al described good results in a clinical study treated by screws alone and suggested that screws are less invasive and can be used alone to treat Mason type II and III fractures of the radial head, especially for Herbert screws, which can be completely buried in the bone.31 Thus, screws for internal fixation of the radial head fracture can greatly replace conventional plates.5
The surgical treatment for radial head fracture tends to be minimally invasive.32 The minimally invasive concept was first applied to the proximal radius by Metaizeau et al in 1980. He suggested that elastic stable intramedullary nail fixation (ESIN) can be used for radial neck fractures in children.33 Sandmann et al proposed this method as a suitable and reliable choice for radial neck fractures in adults.34 Gao et al reported good outcomes in Mason type II radial head fractures studied via intramedullary pinning.13 Jia et al improved this technology to double elastic titanium nails and achieved excellent clinical effectiveness.14
Given the above, we proposed a novel approach based on conventional methods for Mason type II and III radial head fractures with crossed screws. No significant differences were found in the function of the elbow between the two approaches in our study, which indicates that our approach provides an adequate view to expose the fracture site, allowing accurate reduction of the radial head facet and convenient placement of the screws to achieve rigid fixation, although the incision is approximately 2.5 cm in length. There are several advantages to our new approach. First, our incision does not need to cross the elbow joint, which may alleviate pain when the patient performs rehabilitation exercises before the wound heals. In our study, there was a significant difference in the VAS score at 3 days postoperatively between the two groups. Second, our approach can reduce intraoperative blood loss and decrease operative time substantially. There were significant differences in blood loss and operative time between the two groups. However, it should be noted that the blood loss of these two incisions may have little effect on the human body. Finally, the scar of our novel approach is smaller, resulting in long-term cosmetic improvement that is particularly beneficial for patients with specific cosmetic requirements.
Postoperative pain may affect patients’ motivation to engage in rehabilitation exercises.35,36 Meanwhile, pain intensity is aggravated by rehabilitation, which may limit the patient’s participation.37 A previous study have shown that lack of rehabilitation is an independent risk factor for stiff elbow.38 Ranawat et al have emphasized that pain is an important factor to consider throughout the rehabilitation process.39 Vincent et al also proposed that joint pain can affect physical functions and reduce the quality-of-life.40 In our study, the VAS score of the mini-open incision group was significantly lower than that of the controls, it may be beneficial for early rehabilitation exercise.
In the treatment of radial head fracture with a novel small incision, our experience was as follows: (1) This method is only applicable to mason type II and type III fractures with few fracture fragments and small displacement. It should also not be used in patients with radial head fractures with ligament injuries, such as lateral collateral ligament (LUCL) injuries. (2) The deep branch of the radial nerve should be kept away from the operative site by rotating the forearm anteriorly to reduce the chance of injury. (3) When the fracture fragment is posterior, a gap between the anconeus and the extensor carpi ulnaris (ECU), as is used with the Kocher approach, should be used to expose the radial head. When the fracture fragment is anterior, a gap between the extensor digitorum communis (EDC) and the extensor carpi radialis brevis (ECRB), as is used in the Kaplan approach, should be used.41 (4) If the patient’s radial head is not easy to recognize, the C-arm X-ray machine can help localize the incision accurately.
There are still some limitations to this study. First, our study was retrospective rather than prospective. Our analysis was conducted on a small number of patients. Future multicentre, large sample and adequately powered randomized controlled trials are needed to assess the efficacy of these interventions. In addition, the lack of postoperative CT data in some patients is another limitation. Moreover, follow-up of long-term functional outcomes is missing and is expected to improve after 3 years. Finally, the possibility of further reduction of the incision remains to be investigated intensely.
Conclusion
The mini-open approach reduced intraoperative blood loss, shortened operation time, relieved patient pain, and achieved a satisfactory postoperative clinical result, which demonstrates that the novel approach is a safe and effective option for treating radial head fractures.
Data Sharing Statement
All data generated or analysed during this study are included in this published article.
Ethical Statement and Informed Consent
The experimental protocol was established, according to the ethical guidelines of the Helsinki Declaration and was approved by the Human Ethics Committee of Shandong Provincial Hospital Affiliated to Shandong First Medical University. Written informed consent was obtained from each study participant. The typical case in this study provided written informed consent for this image to be published.
Funding
This study was supported by the Shandong Province Major Scientific and Technical Innovation Project (No. 2021SFGC0502), the Shandong Provincial Natural Science Foundation (No. ZR2021MH013; No. ZR2021QH307; No. ZR2020MH088), the Jinan Clinical Medical Science and Technology Innovation Plan (NO. 202019168), the China Scholarship Council (CSC) (grant No. 201808080126), and the incubation fund of Shandong Provincial Hospital (grant No. 2020FY019). The authors, their immediate families, and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Klug A, Gramlich Y, Wincheringer D, Hoffmann R, Schmidt-Horlohé K. Epidemiology and treatment of radial head fractures: a database analysis of over 70,000 inpatient cases. J Hand Surg Am. 2021;46(1):27–35. doi:10.1016/j.jhsa.2020.05.029
2. Duckworth AD, Clement ND, Jenkins PJ, Aitken SA, Court-Brown CM, McQueen MM. The epidemiology of radial head and neck fractures. J Hand Surg Am. 2012;37(1):112–119. doi:10.1016/j.jhsa.2011.09.034
3. Mason ML. Some observations on fractures of the head of the radius with a review of one hundred cases. Br J Surg. 1954;42(172):123–132. doi:10.1002/bjs.18004217203
4. Broberg MA, Morrey BF. Results of treatment of fracture-dislocations of the elbow. Clin Orthop Relat Res. 1987;1(216):109–119.
5. Swensen SJ, Tyagi V, Uquillas C, Shakked RJ, Yoon RS, Liporace FA. Maximizing outcomes in the treatment of radial head fractures. J Orthop Traumatol. 2019;20(1):15. doi:10.1186/s10195-019-0523-5
6. Gokaraju K, Domos P, Aweid O, et al. Mid-term outcomes of surgical management of complex, isolated radial head fractures: a multicentre collaboration. Eur J Orthop Surg Traumatol. 2020;30(8):1369–1376. doi:10.1007/s00590-020-02709-z
7. Ertürer E, Seçkin F, Akman S, Toker S, Sari S, Oztürk I. The results of open reduction and screw or K-wire fixation for isolated type II radial head fractures. Acta orthopaedica et traumatologica turcica. 2010;44(1):20–26. doi:10.3944/aott.2010.2234
8. Han SH, Lee SC, Ryu KJ, Lee JH. Repairing the annular ligament is not necessary in the operation of Mason type 2, 3 isolated radial head fractures if the lateral collateral ligament is intact: minimum 5 years follow-up. Injury. 2013;44(12):1851–1854. doi:10.1016/j.injury.2013.07.019
9. Blomfeldt R, Törnkvist H, Ponzer S, Söderqvist A, Tidermark J. Comparison of internal fixation with total Hip replacement for displaced femoral neck fractures. Randomized, controlled trial performed at four years. J Bone Joint Surg Am. 2005;87(8):1680–1688. doi:10.2106/jbjs.D.02655
10. Kang H, Rho JY, Song JK, Choi J, Kwon YS, Choi S. Comparison between intramedullary nailing and minimally invasive plate osteosynthesis for tibial shaft fractures. Injury. 2021;52(4):1011–1016. doi:10.1016/j.injury.2021.01.038
11. Tsai YT, Hsu CL, Hung CC, Chou YC, Wu CC, Yeh TT. Conventional plate fixation versus minimally invasive modified pedicle screw-rod fixation for anterior pelvic ring fractures. PLoS One. 2019;14(4):e0215233. doi:10.1371/journal.pone.0215233
12. Zhang Y, Xu J, Zhang C, Sun Y. Minimally invasive plate osteosynthesis for midshaft clavicular fractures using superior anatomic plating. J Shoulder Elbow Surgery. 2016;25(1):e7–12. doi:10.1016/j.jse.2015.06.024
13. Gao X, Yin HL, Zhou GJ. Minimally Invasive Treatment of Mason Type II Radial Head Fracture by Intramedullary Pinning. Orthop Surg. 2019;11(5):879–885. doi:10.1111/os.12540
14. Jia Z, Hong Y, Li C, Lin J, Hu X. The clinical efficacy of the minimally invasive treatment of Mason type II radial head fractures using intramedullary fixation with double titanium elastic nails. Am J Transl Res. 2021;13(11):12807–12815.
15. Wang J, Qi W, Shen X, Tao S, Liu Y. Results of arthroscopic fixation of Mason type II radial head fractures using Kirschner wires. Medicine. 2018;97(12):e0201. doi:10.1097/md.0000000000010201
16. Li SL, Lu Y, Wang MY. Is cross-screw fixation superior to plate for radial neck fractures? Bone Joint J. 2015;97-b(6):830–835. doi:10.1302/0301-620x.97b6.34868
17. Grabowski G, Pacana MJ, Chen E. Keloid and Hypertrophic Scar Formation, Prevention, and Management: standard Review of Abnormal Scarring in Orthopaedic Surgery. J Am Acad Orthop Surg. 2020;28(10):e408–e414. doi:10.5435/jaaos-d-19-00690
18. Malhotra S, Hu MS, Marshall CD, et al. Mesenchymal Stromal Cells as Cell-Based Therapeutics for Wound Healing. Stem Cells Int. 2016;2016:4157934. doi:10.1155/2016/4157934
19. Bock O, Schmid-Ott G, Malewski P, Mrowietz U. Quality of life of patients with keloid and hypertrophic scarring. Arch Dermatol Res. 2006;297(10):433–438. doi:10.1007/s00403-006-0651-7
20. Dorr LD, Chao L. The emotional state of the patient after total Hip and knee arthroplasty. Clin Orthop Relat Res. 2007;463:7–12. doi:10.1097/BLO.0b013e318149296c
21. Sun Y, Cai J, Li F, Liu S, Ruan H, Fan C. The efficacy of celecoxib in preventing heterotopic ossification recurrence after open arthrolysis for post-traumatic elbow stiffness in adults. J Shoulder Elbow Surgery. 2015;24(11):1735–1740. doi:10.1016/j.jse.2015.07.006
22. Zwingmann J, Welzel M, Dovi-Akue D, Schmal H, Südkamp NP, Strohm PC. Clinical results after different operative treatment methods of radial head and neck fractures: a systematic review and meta-analysis of clinical outcome. Injury. 2013;44(11):1540–1550. doi:10.1016/j.injury.2013.04.003
23. Sanders RA, French HG. Open reduction and internal fixation of comminuted radial head fractures. Am J Sports Med. 1986;14(2):130–135. doi:10.1177/036354658601400206
24. Ozkan Y, Oztürk A, Ozdemir RM, Aykut S, Yalçin N. Open reduction and internal fixation of radial head fractures. Turkish j Trauma Em Surg. 2009;15(3):249–255.
25. Cheung EV, Steinmann SP. Surgical approaches to the elbow. J Am Acad Orthop Surg. 2009;17(5):325–333. doi:10.5435/00124635-200905000-00007
26. Rollo G, Rotini R, Eygendaal D, et al. Effect of trochleocapitellar index on adult patient-reported outcomes after noncomminuted intra-articular distal humeral fractures. J Shoulder Elbow Surgery. 2018;27(7):1326–1332. doi:10.1016/j.jse.2018.02.073
27. Qian Y, Yu S, Shi Y, Huang H, Fan C. Risk Factors for the Occurrence and Progression of Posttraumatic Elbow Stiffness: a Case-Control Study of 688 Cases. Front med. 2020;7:604056. doi:10.3389/fmed.2020.604056
28. Koslowsky TC, Mader K, Dargel J, Koebke J, Hellmich M, Pennig D. Reconstruction of a Mason type-III fracture of the radial head using four different fixation techniques. An experimental study. J Bone Joint Surg Br. 2007;89(11):1545–1550. doi:10.1302/0301-620x.89b11.19433
29. Giffin JR, King GJ, Patterson SD, Johnson JA. Internal fixation of radial neck fractures: an in vitro biomechanical analysis. Clin Biomechanics. 2004;19(4):358–361. doi:10.1016/j.clinbiomech.2004.01.003
30. Gutowski CJ, Darvish K, Ilyas AM, Jones CM. Comparison of crossed screw versus plate fixation for radial neck fractures. Clin Biomechanics. 2015;30(9):966–970. doi:10.1016/j.clinbiomech.2015.07.001
31. Iacobellis C, Visentin A, Aldegheri R. Open reduction and internal fixation of radial head fractures. Musculoskelet Surg. 2012;96(Suppl 1):S81–6. doi:10.1007/s12306-012-0186-3
32. Wagner FC, Polossek L, Yilmaz T, et al. Biodegradable magnesium vs. polylactide pins for radial head fracture stabilization: a biomechanical study. J Shoulder Elbow Surgery. 2021;30(2):365–372. doi:10.1016/j.jse.2020.06.007
33. Métaizeau JP, Prévot J, Schmitt M. Réduction et fixation des fractures et décollements épiphysaires de la tête radiale par broche centro-médullaire. Technique originale [Reduction and fixation of fractures of the neck of the radious be centro-medullary pinning. Original technic]. Revue de chirurgie orthopedique et reparatrice de l’appareil moteur. 1980;66(1):47–49. French.
34. Sandmann GH, Crönlein M, Neumaier M, et al. Reduction and stabilization of radial neck fractures by intramedullary pinning: a technique not only for children. Eur J Med Res. 2016;21:15. doi:10.1186/s40001-016-0210-4
35. Sharma V, Morgan PM, Cheng EY. Factors influencing early rehabilitation after THA: a systematic review. Clin Orthop Relat Res. 2009;467(6):1400–1411. doi:10.1007/s11999-009-0750-9
36. Földi M, Soós A, Hegyi P, et al. Transversus Abdominis Plane Block Appears to Be Effective and Safe as a Part of Multimodal Analgesia in Bariatric Surgery: a Meta-analysis and Systematic Review of Randomized Controlled Trials. Obes Surg. 2021;31(2):531–543. doi:10.1007/s11695-020-04973-8
37. Ranawat AS, Ranawat CS. Pain management and accelerated rehabilitation for total Hip and total knee arthroplasty. J Arthroplasty. 2007;22(7 Suppl 3):12–15. doi:10.1016/j.arth.2007.05.040
38. Bauer AS, Lawson BK, Bliss RL, Dyer GS. Risk factors for posttraumatic heterotopic ossification of the elbow: case-control study. J Hand Surg Am. 2012;37(7):1422–9.e1–6. doi:10.1016/j.jhsa.2012.03.013
39. Ranawat CS, Ranawat AS, Mehta A. Total knee arthroplasty rehabilitation protocol: what makes the difference? J Arthroplasty. 2003;18(3Suppl 1):27–30. doi:10.1054/arth.2003.50080
40. Vincent KR, Vasilopoulos T, Montero C, Vincent HK. Eccentric and Concentric Resistance Exercise Comparison for Knee Osteoarthritis. Med Sci Sports Exerc. 2019;51(10):1977–1986. doi:10.1249/mss.0000000000002010
41. Barnes LF, Lombardi J, Gardner TR, Strauch RJ, Rosenwasser MP. Comparison of Exposure in the Kaplan Versus the Kocher Approach in the Treatment of Radial Head Fractures. Hand. 2019;14(2):253–258. doi:10.1177/1558944717745662
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.