Back to Journals » Clinical Ophthalmology » Volume 17
Comparative Study Between Non-Diffractive Extended Depth of Focus and Monofocal Intraocular Lenses
Authors Kandavel R, Colvard M , Dredge J, Bayle M, Alam T, Snyder J, Hall B
Received 20 December 2022
Accepted for publication 30 March 2023
Published 14 April 2023 Volume 2023:17 Pages 1161—1168
DOI https://doi.org/10.2147/OPTH.S402069
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Rom Kandavel,1 Michael Colvard,1 Justin Dredge,1 Michael Bayle,1 Tamanna Alam,1 James Snyder,1 Brad Hall2
1Colvard-Kandavel Eye Center, Encino, CA, 91316, USA; 2Sengi, Penniac, NB, E3A 8X8, Canada
Correspondence: Rom Kandavel, Colvard-Kandavel Eye Center, 5363 Balboa Blvd Suite 540, Encino, CA, 91316, USA, Tel +1-818-906-2929, Email [email protected]
Purpose: To evaluate the visual acuity and quality of vision in bilaterally implanted ZCBOO/ZCTx monofocal (Johnson & Johnson Vision) intraocular lens (IOL) and bilaterally implanted DATx15 extended depth of focus (EDOF) IOL (Alcon Vision, LLC).
Methods: A single site, non-interventional study comparing ZCBOO/ZCTx monofocal IOL patients implanted with DATx15 IOL toric or non-toric versions in both eyes. A total of 30 patients (60 eyes) completed the study in the monofocal group, 32 (64 eyes) in the EDOF group, and all were targeted for emmetropia. Binocular uncorrected distance, intermediate (66cm), and near (40cm) visual acuities and distance corrected distance, intermediate (66cm) and near (40cm) visual acuities were assessed. Binocular distance corrected defocus curve testing was from − 3.5 D to +3 D. Patient reported visual disturbances (QUVID) and IOL satisfaction (IOLSAT) questionnaires were administered.
Results: The DATx15 group mean uncorrected visual acuity was 0.15 ± 0.10 logMAR at 66cm and 0.36 ± 0.14 logMAR at 40cm, compared to 0.24 ± 0.15 logMAR and 0.59 ± 0.17 logMAR respectively for the ZCBOO/ZCTx group. The DATx15 group (23 respondents, 74%) also reported significantly more spectacle independence at near with the IOLSAT (p < 0.01), compared to the ZCBOO/ZCTx group (13 respondents, 43%). Glare, halos, starbursts, and blur reported on the QUVID questionnaire were similar in the two groups.
Conclusion: The DATx15 group had improved near and intermediate vision and increased spectacle independence compared to the ZCBOO/ZCTx group.
Keywords: EDOF IOL, cataract surgery, Vivity, monofocal
Plain Language Summary
The natural lens inside the eye can become opaque, reducing visual acuity. Cataract surgery involves replacing the natural lens with an artificial intraocular lens (IOL), to restore visual acuity. There are a variety of IOL designs that are available. One type provides good vision at one distance, and is known as a monofocal. Multifocal IOLs can provide good vision at more than one distance, such as a bifocal IOL (2 distances) or a trifocal IOL (3 distances). In addition, extended depth of focus (EDOF) IOLs are designed to provide one continuous focal point for good vision when looking at far, intermediate, and near objects. The purpose of this study was to compare the visual acuity and quality of vision between a relatively new EDOF IOL and a monofocal IOL.
Introduction
Cataract surgery patients have a variety of intraocular lens (IOL) technologies available, which each provide a different range of spectacle independence. Monofocal IOLs allow good visual acuity at 1 focal point, but patients may still require spectacles to see objects clearly at other distances. Multifocal IOLs are designed to offer 1 or 2 additional focal points and to further reduce spectacle dependence.1–3 The aim of diffractive multifocal IOLs is to split incoming light into multiple distinct focal points that each deliver clear vision at a particular distance (far, intermediate, or near). Visual acuities with multifocal IOLs have been reported to be good at target ranges of vision (far, intermediate, or near),1–3 however as a consequence of splitting incoming light, studies have suggested that visual disturbances are high compared to monofocal IOLs.4–6
Extended depth of focus (EDOF) IOLs are a relatively new class of presbyopia correcting lenses. The optical design of each lens varies significantly, however they are all generally intended to create a continuous focal point, rather than multiple foci, to allow for clear vision at far, intermediate, and near. Current optical designs include wavefront shaping technology,7 small apertures,8 spherical aberration,9 and diffractive optics.10 These EDOF IOLs aim to allow recipients to have good intermediate and functional reading vision with minimal visual disturbances compared to previous multifocal IOL design.11,12 However, there have been reports of visual disturbances with diffractive optic EDOF IOLs.13
The Acrysof IQ Vivity IOL (Alcon Vision, LLC) is a non-diffractive EDOF IOL.7 The EDOF effect is reported to be produced by stretching and shifting of the wavefront, and is termed wavefront shaping technology.7 When compared to a monofocal control in a large clinical trial, the Vivity IOL provided better intermediate and near visual acuity.14 In addition, comparable distance visual acuity and visual disturbance profiles were reported for Vivity and the monofocal control.14 Initial reports of the Vivity IOL have been favorable, however, as this is a relatively new IOL, there remains limited data on real world clinical outcomes. There are also no reports comparing Vivity to Tecnis monofocal IOLs (Johnson & Johnson Vision).
The purpose of this study was to compare visual acuities, defocus curves, and visual disturbance profiles of two similar cohorts of patients bilaterally implanted with either a monofocal IOL or a Vivity IOL.
Methods
This was a non-randomized, non-interventional study. Informed consent for data collection and participation in the study was approved by WCG IRB (20201483) and informed consent was collected in all patients participating prior to data collection. International Harmonization (ICH) guidelines, the tenets of the Declaration of Helsinki, Good Clinical Practice (GCP), and Health Insurance Portability and Accountability Act (HIPAA) regulations were followed.
A total of 33 patients (66 eyes) were bilaterally implanted with a DAT015 or DATx15 toric IOL by a single surgeon, at a single clinical location. Emmetropia was targeted in all eyes. One subject in the DATx15 group did not complete the study as they were lost to follow up. A retrospective chart review was conducted to identify subjects for inclusion as a control group in this study. The control group consisted of a monofocal cohort of previously operated ZCBOO and ZCTx toric patients (Johnson & Johnson Vision) who were identified within the surgeon’s practice. All ZCBOO/ZCTx subjects were identified and recruited to follow up for a study data collection visit that was administered at least 3 months after the last surgery. The chart review identified 35 subjects for inclusion (70 eyes), of which, 33 agreed to participate in this study. A total of 3 subjects in the ZCBOO/ZCTx group did not complete the study as they were lost to follow up.
All patients in both the control and treatment group were previous emmetropes or hyperopes between the ages of 50–80 years old. To be included in the study all patients had to fall within binocularly 0.50 diopters (D) of emmetropia and have less than 0.75 D of astigmatism at the final data collection appointment, no previous corneal or retinal surgery, no strabismus, no macular disease, and no glaucoma. Ocular hypertension without visual field defects or nerve fiber loss were allowed. Most surgeries were traditional phacoemulsification cataract surgeries without femtosecond laser assistance (104 eyes, 84%) and there were no complications in any of the cases enrolled in the study. In cases where femtosecond laser assistance was utilized, the Victus (Bausch + Lomb) was used. Preoperative biometric data that was collected included a preoperative a-scan biometry with the IOL Master 500 (Carl Zeiss Meditec), corneal topography with the Galilei (Ziemer Ophthalmic Systems), macular ocular coherence tomography (OCT) with Zeiss Cirrus OCT (Carl Zeiss Meditec), and an interpupillary distance (IPD) with a Topcon KR-800S (Topcon Healthcare). Postoperative a-scan biometry with the same device was also obtained. All IOL power calculations were performed using the Holladay II or Alcon-Holladay online toric calculator. All vision measurements were obtained using a standard logarithm of the minimum angle of resolution (logMAR) early treatment diabetic retinopathy study (ETDRS) chart.
The primary endpoints were binocular distance corrected intermediate visual acuity (DCIVA; 66 cm) and binocular distance corrected near visual acuity (DCNVA; 40cm). Secondary endpoints included binocular uncorrected distance visual acuity (UDVA), binocular corrected distance visual acuity (CDVA), monocular uncorrected intermediate visual acuity (UIVA; 66cm), monocular DCIVA, monocular uncorrected near visual acuity (UNVA), and monocular DCNVA. Binocular defocus curve from +3.00 to −3.5 diopters in 0.50 diopter increments was also collected for each group using a standard ETDRS chart. Two questionnaires were administered: the questionnaire about satisfaction with your vision after surgery (Post-operative IOLSAT Ver. B, 11 Oct 2019) and the questionnaire about the quality of your vision after surgery (Post-operative QUVID Ver. B, 11 Oct 2019). Both of these questionnaires are proprietary Alcon questionnaires (Alcon Vision, LLC) that ask subjects to rate their satisfaction with their vision at distance, intermediate, and near and to rate the frequency, severity, and bothersomeness of visual disturbances.
Statistical analyses were performed using SAS software (version 9.4; SAS Institute, Inc). The Kruskal–Wallis test was used to compare non-parametric variables, a one-sided 2-sample test for equality of proportions was used for questionnaire responses, and a p-value of less than 0.05 was considered significant. We estimated that a sample size of 20 patients (per group) would be required, assuming the difference in DCNVA between the DAT015/DATx15 and ZCBOO/ZCTx groups was −0.138 logMAR, with a margin of error of 0.034, and an effect size of 1.09.
Results
Both of the DATx15 and ZCBOO/ZCTx groups had similar preoperative biometric measurements and patient demographics (Table 1). No statistically significant differences were found in any of the baseline characteristics of the two groups using the Kruskal–Wallis test. Average age, axial length, anterior chamber depth, average keratometry, interpupillary distance, and average IOL power implanted were all similar in both groups (p > 0.05). There were more toric lenses implanted in the DATx15 group (29) compared to the ZCBOO/ZCTx group (7).
 |
Table 1 Preoperative and Patient Demographics |
The 3 month postoperative monocular and binocular visual acuities are summarized in Table 2 and Table 3 respectively. There was the same general trend for both monocular and binocular visual acuities. Postoperative binocular and monocular UDVA was not statistically significant between groups (p > 0.05). Postoperative monocular and binocular CDVA was statistically significantly different between groups (p = 0.007; p = 0.034), with the ZCBOO/ZCTx group having a lower mean than the DATx15 group. The DATx15 group maintained an average monocular CDVA of 0.02 ± 0.07 logMAR. Postoperative binocular and monocular UIVA, DCIVA, UNVA, and DCNVA were also significantly better in the DATx15 group (p ≤ 0.02).
 |
Table 2 Summary of Monocular Visual Acuity |
 |
Table 3 Summary of Binocular Visual Acuity |
Defocus curve data was recorded as binocular data for both ZCBOO/ZCTx and DATx15 groups, and is summarized in Figure 1. Binocular defocus curve testing followed a similar pattern to near, intermediate, and distance visual acuity. In the hyperopic spectrum, from +3 to 0 D, the ZCBOO/ZCTx group demonstrated better visual acuity than the DATx15 group (p < 0.05). No statistically significant difference was seen at −0.5 D between the two groups (p = 0.6). At all myopic or reading defocus points from −1.0 to −3.5 D the DATx15 group demonstrated significantly better visual acuity than the ZCBOO/ZCTx group (p < 0.05).
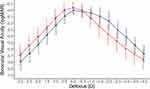 |
Figure 1 Binocular defocus curve for ZCBOO/ZCTx group (red) and DATx15 group (blue). Error bars represent mean ± standard deviation. |
Satisfaction (IOLSAT) and quality of vision (QUVID) questionnaires were collected in all participants, and results are summarized in Table 4 and Table 5 respectively. These were patient self-administered questionnaires and there were 3 patients in the control group and 1 patient in the DAT group that returned questionnaires that were incomplete. Overall, there was a statistically significant difference with a reduced reported dependency on glasses in general (p = 0.035) and for near (p = 0.004) in the DATx15 group compared to the ZCBOO/ZCTx group. There was no statistically significant difference in reported frequency of glasses use between the two groups for distance and intermediate (p > 0.05 for both). In bright and dim light at distance, both groups performed similarly, with approximately 90% of subjects in each group never or rarely needing glasses. Similarly, both groups had approximately the same percentage of subjects reporting never or rarely needing glasses at intermediate in bright light. A higher percentage of subjects in the DATx15 group reported never or rarely needing glasses at near in bright and dim light and at intermediate in dim light (71% [22 subjects], 58% [18 subjects], and 90% [28 subjects] respectively) compared to the ZCBOO/ZCTx group (23% [7 subjects], 20% [6 subjects], and 74% [22 subjects] respectively). The reported use of glasses for near in both dim and bright conditions was statistically significant (p = 0.005 and p = 0.004) in the IOLSAT questionnaire responses. In addition, the percentage of subjects reporting being satisfied or very satisfied with their vision was 84% (26 subjects) in the DATx15 group and 83% (25 subjects) in the ZCBOO/ZCTx group. Nighttime starburst and haloes, daytime glare and blur, and negative dysphotopsias were reported in both groups at similar frequencies. Almost all subjects reported a complete resolution of these symptoms, if reported, with the use of corrective lenses.
 |
Table 4 Summary of IOLSAT Questionnaire Responses |
 |
Table 5 Summary of QUVID Questionnaire Responses |
Finally, the monocular (n = 64) and binocular (n = 32) corrected and uncorrected visual outcomes of the DATx15 group were analyzed in relation to preoperative and postoperative biometric data to determine if any statistical associations could be made with the postoperative vision at near and intermediate. Preoperative and postoperative biometric variables considered were axial length, interpupillary distance (IPD), anterior chamber depth (ACD), IOL power implanted, and preoperative average keratometry. The results are summarized in Table 6. Axial length was not found to have any correlation with postoperative near or intermediate visual acuity. Better intermediate visual acuity was not predicted by any of the biometric variables measured. A deeper preoperative average anterior chamber depth was associated with better binocular vision at 40cm (r = −0.38, p = 0.032). There were also positive associations between monocular DCNVA and smaller IPD (r = 0.34, p = 0.005) and larger ACD (r = −0.38, p = 0.032). Similarly, better monocular UNVA was also associated with weaker IOL power (r = 0.35, p = 0.005) implanted as well as higher preoperative ACD (r = −0.28, p = 0.023).
 |
Table 6 Biometric Correlations |
Discussion
In this study, we have compared visual acuity, and patient reported spectacle independence and visual disturbance between a non-diffractive EDOF IOL (Vivity) and a monofocal IOL (Tecnis monofocal). Binocular uncorrected and distance corrected visual acuities at near and intermediate were significantly better in the DATx15 group compared to the ZCBOO/ZCTx group, and there were no significant differences at distance between the groups. This is an expected result, since the aim of any presbyopia correcting IOL (such as a multifocal or EDOF) is to offer increased visual performance at near or intermediate, compared to a monofocal IOL, without degrading visual performance at distance. The results of our study suggest that the Vivity lens achieves this aim. Two large, multicenter15 and multicounty16 studies reported similar visual performance of the Vivity lens compared to a different monofocal IOL (SN60WF AcrySof IQ monofocal; Alcon Vision, LLC).
Patients who undergo cataract surgery and IOL implantation have high expectations of spectacle independence. This is especially true for presbyopia correcting IOLs, which are typically premium IOLs requiring patients to pay extra out of pocket expenses. Spectacle independence overall and under bright lighting conditions was high (> 80%) at distance and intermediate for both groups. Spectacle independence at near under all conditions was significantly higher in the DATx15 group compared to the ZCBOO/ZCTx group (a difference in reported percentage of 38 to 48). This is also expected since the uncorrected near visual acuity was significantly better in the DATx15 group compared to the ZCBOO/ZCTx group. In bright conditions, 71% of patients reported being spectacle independent at near with the DATx15 IOL compared to 23% in the ZCBOO/ZCTx group. Higher spectacle independence with the Vivity lens compared to a monofocal (SN60WF) has been reported in other studies.15,16 There was no significant difference in spectacle independence between groups at intermediate, under bright light conditions. This is unexpected given the nature of the lenses and the differences under dim light conditions. A possible explanation is that under bright conditions, monofocal IOLs can provide acceptable visual acuity at intermediate.
A concern with presbyopia correcting IOLs is that they may lead to increased visual disturbances for patients compared to a monofocal. Increased visual disturbances have been reported with multifocal IOLs (including bifocal and trifocal)4,5 and diffractive EDOF IOLs.13 The QUVID results between the monofocal ZCBOO/ZCTx group and the DATx15 group were very similar for the frequency of all visual disturbances reported. This indicates that the Vivity IOL may have a visual disturbance profile that is similar to a monofocal IOL, which has been observed in other studies.4,15,16 The reported frequency of glare in this study (55 to 62%) appears to be higher than reports of Vivity and monofocal IOLs in other studies (33 to 53%).4,12,16–18 Comparing patient reported outcomes across studies with different endpoints, patient populations, and methodologies is challenging, which may explain these differences.
The biometric data comparison to postoperative visual acuity in this study is, to the best of our knowledge, not reported in any other studies of the Vivity IOL. We found significant correlations between biometric data and postoperative near visual acuity. Correlations between near visual acuity and IPD, ACD, and IOL power were stronger and statistically significant when analyzing these outcomes with the monocular data. The binocular visual acuity results likely yielded less than significant outcomes due to the lower sample size. Interestingly, a smaller IPD relating to better monocular vision would theoretically have no relevance to binocular fusion playing a role in better near vision. Another intrinsic feature of patients with smaller IPD may be a more likely reason for this trend. Further research to help refine our understanding of how reduced IPD may result in better near vision with EDOF IOL is warranted. Weaker IOL power and deeper ACD are also novel trends that may benefit from further study as well. Further study of biometric data may allow improved preoperative patient selection for EDOF lenses.
A limitation of this study was the mix of prospective and retrospective data. A randomized and patient examiner masked prospective study comparing the 2 groups would have yielded stronger results. Unmasked subjects and examiners could have introduced bias. However, including the retrospective control group does add strength to the study compared with a study of a single group. Future comparisons of the EDOF used in this study to other EDOF or multifocal IOLs are warranted. Another limitation was the inclusion of toric and non-toric lenses, as well as the use of both standard phacoemulsification with femtosecond laser assisted cataract surgery. However, this does provide a real world comparison of the ZCBOO/ZCTx and the DATx15 groups.
In conclusion, this study supports previous reports that the DATx15 toric and non-toric IOLs have a similar visual disturbance profile to monofocal IOLs while providing improved near and intermediate vision with reduced dependence on spectacles.
Funding
This study was supported with an investigator-initiated study grant (59269351) from Alcon Vision, LLC, Fort Worth, TX, USA.
Disclosure
Rom Kandavel reports that he has received consulting fees from Alcon Laboratories. Brad Hall reports that he has received consulting fees from Ace Vision Group. The authors report no other conflicts of interest in this work.
References
1. Gatinel D, Houbrechts Y. Comparison of bifocal and trifocal diffractive and refractive intraocular lenses using an optical bench. J Cataract Refract Surg. 2013;39(7):1093–1099. doi:10.1016/j.jcrs.2013.01.048
2. Kohnen T, Marchini G, Alfonso JF, et al. Innovative trifocal (quadrifocal) presbyopia-correcting IOLs: 1-year outcomes from an international multicenter study. J Cataract Refract Surg. 2020;46(8):1142–1148. doi:10.1097/j.jcrs.0000000000000232
3. Chow SSW, Chan TCY, Ng ALK, Kwok AKH. Outcomes of presbyopia-correcting intraocular lenses after laser in situ keratomileusis. Int Ophthalmol. 2019;39:1199–1204. doi:10.1007/s10792-018-0908-0
4. Schallhorn JM. Multifocal and extended depth of focus intraocular lenses: a comparison of data from the United States food and drug administration premarket approval trials. J Refract Surg. 2021;37(2):98–104. doi:10.3928/1081597X-20201111-02
5. Hovanesian JA, Jones M, Allen Q. The PanOptix trifocal IOL vs the ReSTOR 2.5 active focus and ReSTOR 3.0-add multifocal lenses: a study of patient satisfaction, visual disturbances, and uncorrected visual performance. Clin Ophthalmol. 2021;15:983–990. doi:10.2147/OPTH.S285628
6. Cao K, Friedman DS, Jin S, et al. Multifocal versus monofocal intraocular lenses for age-related cataract patients: a system review and meta-analysis based on randomized controlled trials. Surv Ophthalmol. 2019;64(5):647–658. doi:10.1016/j.survophthal.2019.02.012
7. Kohnen T. Nondiffractive wavefront-shaping extended range-of-vision intraocular lens. J Cataract Refract Surg. 2020;46(9):1312–1313. doi:10.1097/j.jcrs.0000000000000247
8. Grabner G, Ang RE, Vilupuru S. The small-aperture IC-8 intraocular lens: a new concept for added depth of focus in cataract patients. Am J Ophthalmol. 2015;160(6):1176–1184 e1171. doi:10.1016/j.ajo.2015.08.017
9. Bellucci R, Cargnoni M, Bellucci C. Clinical and aberrometric evaluation of a new extended depth-of-focus intraocular lens based on spherical aberration. J Cataract Refract Surg. 2019;45(7):919–926. doi:10.1016/j.jcrs.2019.02.023
10. Cochener B, Concerto Study G. Clinical outcomes of a new extended range of vision intraocular lens: international multicenter concerto study. J Cataract Refract Surg. 2016;42(9):1268–1275. doi:10.1016/j.jcrs.2016.06.033
11. Ozulken K, Kiziltoprak H, Yuksel E, Mumcuoglu T. A comparative evaluation of diffractive trifocal and new refractive/extended depth of focus intraocular lenses for refractive lens exchange. Curr Eye Res. 2021;46(6):811–817. doi:10.1080/02713683.2020.1833347
12. Hovanesian JA, Jones M, Allen Q. The vivity extended range of vision IOL vs the PanOptix trifocal, ReSTOR 2.5 active focus and ReSTOR 3.0 multifocal lenses: a comparison of patient satisfaction, visual disturbances, and spectacle Independence. Clin Ophthalmol. 2022;16:145–152. doi:10.2147/OPTH.S347382
13. Pedrotti E, Carones F, Talli P, et al. Comparative analysis of objective and subjective outcomes of two different intraocular lenses: trifocal and extended range of vision. BMJ Open Ophthalmol. 2020;5:e000497. doi:10.1136/bmjophth-2020-000497
14. US FDA. AcrySofTM IQ VivityTM extended vision Intraocular Lens (IOL): summary of safety and effectiveness data; 2022. Available from: https://www.accessdata.fda.gov/cdrh_docs/pdf/P930014S126B.pdf.
15. McCabe C, Berdahl J, Reiser H, et al. Clinical outcomes in a United States registration study of a novel extended depth of focus intraocular lens with a nondiffractive design. J Cataract Refract Surg. 2022;48(11):1297–1304. doi:10.1097/j.jcrs.0000000000000978
16. Bala C, Poyales F, Guarro M, et al. Multicountry clinical outcomes of a new nondiffractive presbyopia-correcting IOL. J Cataract Refract Surg. 2022;48(2):136–143. doi:10.1097/j.jcrs.0000000000000712
17. Kohnen T, Petermann K, Bohm M, et al. Nondiffractive wavefront-shaping extended depth-of-focus intraocular lens: visual performance and patient-reported outcomes. J Cataract Refract Surg. 2022;48(2):144–150. doi:10.1097/j.jcrs.0000000000000826
18. Guarro M, Sararols L, Londono GJ, et al. Visual disturbances produced after the implantation of three extended-depth-of-focus intraocular lenses versus one monofocal lens. J Cataract Refract Surg. 2022;48(12):1354–1359. doi:10.1097/j.jcrs.0000000000000988
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
