Back to Journals » Clinical Ophthalmology » Volume 17
Clinical Outcomes of a Non-Diffractive Extended Depth-of-Focus IOL in Eyes with Mild Glaucoma
Authors Ferguson TJ , Wilson CW, Shafer BM , Berdahl JP , Terveen DC
Received 11 January 2023
Accepted for publication 8 March 2023
Published 15 March 2023 Volume 2023:17 Pages 861—868
DOI https://doi.org/10.2147/OPTH.S404369
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Tanner J Ferguson,1,2 Caroline W Wilson,3 Brian M Shafer,4 John P Berdahl,1,2 Daniel C Terveen1,2
1Vance Thompson Vision, Sioux Falls, SD, USA; 2University of South Dakota Sanford School of Medicine, Sioux Falls, SD, USA; 3Wolfe Eye Clinic, Cedar Rapids, IA, USA; 4Chester County Eye Care, Malvern, PA, USA
Correspondence: Tanner J Ferguson, Vance Thompson Vision, 3101 W. 57th Street, Sioux Falls, SD, 57108, USA, Email [email protected]
Purpose: To evaluate the clinical outcomes of a non-diffractive, wavefront-shaping extended depth-of-focus (EDOF) intraocular lens (IOL) in eyes with mild open-angle glaucoma (OAG).
Setting: Private practice; Sioux Falls, South Dakota.
Design: Prospective, open-label, interventional study.
Methods: In total, 52 eyes of 26 patients with mild OAG were enrolled and completed the study. All patients were bilaterally implanted with a non-diffractive, wavefront-shaping EDOF IOL. Seventy-seven percent of the patients were implanted with a trabecular microbypass stent at the time of surgery. Primary outcome measures included binocular corrected and uncorrected distance visual acuity (CDVA and UDVA), uncorrected intermediate and near visual acuity (UIVA and UNVA) and contrast sensitivity as measured by a Pelli-Robson chart. A subjective questionnaire was also administered to patients.
Results: At 4 months postoperative, the mean binocular UDVA and CDVA was 0.03 ± 0.12 and − 0.06 ± 0.07, respectively. The mean UIVA and UNVA were 0.18 ± 0.12 and 0.31 ± 0.18, respectively. Eighty-five percent of the subjects achieved ≥ 20/25 UDVA and 77% of the subjects achieved ≥ 20/32 UIVA at 4 months postoperative. The mean binocular mesopic contrast sensitivity was 1.76 ± 0.16 at a spatial frequency of 1 cycle-per-degree (cpd). Eighty-five percent of the subjects reported they would choose the same lens and 1 subject reported they would choose a different IOL if it meant reduced spectacle independence.
Conclusion: The non-diffractive, wavefront-shaping EDOF IOL can be safely implanted in eyes with mild, pre-perimetric open-angle glaucoma with favorable uncorrected distance and intermediate visual acuity. The contrast sensitivity measurements were favorable and the subjective questionnaire revealed satisfactory spectacle independence and patient satisfaction.
Keywords: EDOF IOL, extended depth-of-focus IOL, cataract surgery, refractive cataract surgery, cataract surgery in glaucoma
Introduction
Modern refractive cataract surgery continues to evolve with the continued introduction of newer-generation intraocular lens (IOL) options aimed at mitigating spectacle independence.1 The advancements in IOL technology have led to improved outcomes and consequently elevated patient expectations.1,2
The advent of minimally invasive glaucoma surgery (MIGS) has led to earlier surgical management of glaucoma in patients undergoing cataract surgery.3,4 It has long been thought that patients with glaucoma are not candidates for refractive cataract surgery with presbyopia-mitigating IOL options owing to a concern of further decreasing contrast sensitivity and compromising visual quality.5 While the early generation multifocal IOLs did appreciably reduce contrast sensitivity, novel presbyopia-correcting IOL options have been introduced that offer a more favorable side effect profile.6,7
The presbyopia-correcting IOL landscape has grown considerably over the past 5 years with the introduction and expansion of bifocal, trifocal, and EDOF technology.2,8 Many of the currently available presbyopia-correcting IOL options employ diffractive technology and focus or split light into multiple foci. However, presbyopia-correcting IOL options that use diffractive technology to establish multiple foci are associated with photic phenomena such as glare, halos and a reduction in contrast sensitivity.9 Recently, a new, non-diffractive, wavefront-shaping extended depth-of-focus (EDOF) IOL (AcrySof IQ Vivity, DFT015) was introduced. As the first non-diffractive EDOF option, the Vivity IOL utilizes novel wavefront-shaping technology using surface transition elements that stretch and shift the wavefront to provide a continuous, extended range of vision. Multiple studies have been completed demonstrating favorable visual outcomes with this IOL including an increased degree of spectacle independence compared to a monofocal IOL.7,10 Further, this IOL has been demonstrated to provide favorable mesopic contrast sensitivity and a visual disturbance profile comparable to a monofocal IOL.7 Moreover, a recent study comparing the Vivity IOL to a monofocal IOL reported favorable long-term outcomes with patients in the Vivity group reporting enhanced spectacle independence out to 3 years postoperative.11 Despite the growing evidence supporting its use as a presbyopia-mitigating IOL, no studies have been performed evaluating its use in eyes with glaucoma.
This present study aims to evaluate visual outcomes in patients with mild glaucoma and concomitant cataract implanted with a presbyopia-mitigating, non-diffractive EDOF IOL (AcrySof IQ Vivity, Alcon). A prospective, single-site, non-comparative trial was performed to evaluate visual performance, contrast sensitivity and assess patient-reported outcomes.
Methods
This was a prospective, controlled, open-label, interventional study performed at a single site (Sioux Falls, SD). This study was reviewed and approved by the University of South Dakota Institutional Board. All participants provided written informed consent and the study was conducted in accordance with the tenets of the Declaration of Helsinki. This study was funded by an investigator-initiated trial grant and was registered with clinicaltrials.gov (NCT04670575). This study enrolled patients from January 2021 to April 2022.
Patients
This study aimed to enroll subjects age ≥45 with previously diagnosed mild stage (pre-perimetric) open-angle glaucoma and visually significant cataracts. Disease staging was based on the American Academy of Ophthalmology Preferred Practice Pattern guidelines, which states that mild glaucoma is defined as “definite optic disc, RNFL, or macular imaging abnormalities consistent with glaucoma and a normal visual field.”12 All patients were implanted with a non-diffractive, wavefront-shaping EDOF non-toric or toric IOL (AcrySof IQ Vivity or AcrySof IQ Vivity Toric). A trabecular microbypass stent device (iStent inject, Glaukos Corp.) was concomitantly implanted at the time of cataract surgery following IOL implantation for additional IOP control in certain cases based on the discretion of the surgeon.
Patients with secondary forms of open-angle glaucoma were excluded. Patients were excluded if they did not have the potential for BCDVA of 20/20 or better in each eye based on the investigator’s medical opinion. Patients with prior refractive surgery were excluded. Patients with ocular comorbidities other than OAG that could impact the potential postoperative BCDVA were also excluded. There was no IOP criterion for determining concomitant implantation of trabecular microbypass stent, and the decision was made on an individualized basis at the discretion of the surgeon.
Following screening and informed consent, baseline testing was performed. In addition to a comprehensive anterior and dilated fundoscopic exam, adjunct baseline testing included a 24–2 SITA Fast Humphrey Visual Field, OCT retinal nerve fiber layer and OCT of the macula. All subjects were set to a refractive target of plano (0.00) in both eyes as calculated by Barrett Universal II/Barrett Toric Calculator. ORA (Optiwave Refractive Analysis, Alcon) was used intraoperatively on all subjects.
Outcome Measures
Cataract surgery occurred in a unilateral, sequential fashion on different days and was not performed on the same day as in immediately sequential bilateral cataract surgery (ISBCS). Following the procedure, patients were treated with a combination steroid, antibiotic and non-steroid anti-inflammatory drop once daily in each eye for 4 weeks. Following bilateral implantation of the non-diffractive EDOF IOL, data was collected at a 4-month postoperative visit, which ranged from 3 to 5 months after surgery. At the postoperative visit, a manifest refraction was obtained. Uncorrected and corrected distance visual acuity (UCDVA and CDVA) were obtained on an ETDRS chart at a distance of 20 feet. Uncorrected and corrected intermediate visual acuity were obtained at 66 cm. Uncorrected and corrected near visual acuity were obtained at 40 cm. For visual acuity measurements, monocular and binocular measurements were obtained and all visual acuity testing occurred in photopic lighting conditions.
Contrast sensitivity measurements were obtained using the Pelli-Robson chart according to what has been described in prior studies in mesopic conditions.13,14 Contrast sensitivity was not obtained prior to cataract surgery owing to the presence of a cataract impacting baseline measurements. For testing, letters are arranged in triplets, where contrast is constant within a group. The last group in which at least 2 of the 3 letters were correctly identified determined the value, which was reported in log units. A subjective questionnaire, adapted from the Patient Reported Spectacle Independence Questionnaire (PRSIQ), was employed to patient satisfaction and spectacle independence.15
Intraocular Lens
The AcrySof IQ Vivity IOL was FDA approved in 2020 and is a non-diffractive, single-piece, foldable IOL composed of a high refractive index, hydrophobic acrylic material. The anterior surface of the IOL employs a novel, wavefront-shaping X-WAVE™ technology. The X-Wave technology is incorporated into the central 2.2 mm of the IOL and thus, postoperative vision may be influenced by the size of the pupil.16 The IOL also incorporates a negative spherical aberration profile to compensate for the cornea’s spherical aberration profile.
The wavefront-shaping X-WAVE technology is designed to stretch and shift the wavefront without splitting light to produce an extended, continuous range of vision rather than multiple focal points. The two elements – stretch and shift – collectively create an extended region of focus without splitting light. This wavefront-shaping technology and spherical optics of the Vivity IOL are thought to minimize optical phenomena with prior studies showing a low incidence of visual disturbances.7
Statistical Analysis
All statistical analysis was performed using GraphPad Prism software (Version 9, GraphPad Software, Inc.). Descriptive data were recorded as mean ± standard deviation (SD) unless noted otherwise.
Results
Patient Demographics
52 eyes of 26 subjects were successfully enrolled and completed the study. All 52 eyes were implanted with a non-diffractive toric or non-toric Vivity EDOF IOL in both eyes. The mean age of the 26 subjects was 69.4 ± 6.6 and 54% (n=14) of the subjects were female. Seventy-seven percent (n=20) of the subjects were implanted with a trabecular microbypass device at the time of surgery. All subjects had a confirmed diagnosis of mild glaucoma based on testing obtained on the day of screening. For visual field testing, the baseline mean deviation value across all 52 eyes was −1.4 ± 1.9 dB. The mean pattern deviation value was 2.1 ± 1.1 dB. The mean visual field index (VFI) was 97.6 ± 2.4. For IOP, the mean baseline IOP amongst all eyes was 18.5 ± 4.6 mmHg. The baseline characteristics are summarized in Table 1.
 |
Table 1 Preoperative Characteristics |
Refractive and Visual Outcomes
For refractive outcomes, 83% (n=43) had a mean refractive spherical equivalent (MRSE) within ±0.50 D across all 52 eyes and 96% (n=50) were within ±1.00 D; the overall mean MRSE was −0.27 ± 0.35 D at month 4. The mean binocular UDVA was 0.03 ± 0.12 LogMAR with 85% (n=22) of the subjects achieving 20/25 or better UDVA and 65% of the subjects achieving 20/20 or better UDVA. Only 1 subject was worse than 20/32 and was 20/40 UCVA owing to residual refractive error after surgery. The mean CDVA was −0.06 ± 0.07 LogMAR and 96% (n=25) were 20/20 or better.
For intermediate visual acuity, the mean binocular UIVA was 0.17 ± 0.12 LogMAR with 77% of subjects achieving 20/32 or better UIVA. Forty-six percent (n=12) of the subjects were 20/25 or better. For near visual acuity, the mean binocular UNVA was 0.31 ± 0.17 LogMAR. Sixty-five percent (n=17) achieved J3 or better and 46% (n=12) achieved J2 or better UNVA. The visual and refractive outcomes are summarized in Figures 1 and 2.
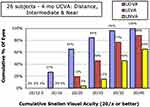 |
Figure 2 Uncorrected visual acuity outcomes are shown. The percentage of eyes achieving 20/× or better is shown for uncorrected distance, intermediate and near visual acuity. |
Binocular measures of mesopic contrast sensitivity were obtained with the Pelli-Robson chart. At the 4-month visit, the mean binocular CS value was 1.78 ± 0.17. Overall, 92% of the subjects had a mean binocular CS value ≥1.6 and 62% had a mean binocular CS value ≥1.8.
The baseline glaucoma testing – VF and OCT optic nerve head – was not repeated at the 4-month visit. The mean IOP at that visit was 13.3 ± 2.9, representing a >5 mmHg reduction in IOP from baseline across all eyes.
Subjective Questionnaire
On a scale of 1–5 (1 = very satisfied, 5 = very dissatisfied), subjects reported a mean response of 1.8 ± 1.2 when asked about satisfaction with their vision. On a scale of 1–5 (1 = not at all, 5 = extremely), subjects reported a mean response of 2.6 ± 1.3 when asked about noting glare/halos in dim light situations; 65% of the patients reported not being bothered or very little dissatisfaction with glare/halo symptoms. When asked if subjects would choose a different IOL with reduced glare and halos if it meant increased reliance on glasses for near/intermediate tasks, only one subject reported that they would choose a different IOL. When asked if subjects would choose the same lens, 85% of the patients reported they would choose the same IOL.
Results from the questionnaire evaluating spectacle independence are summarized in Table 2. Regarding reliance on glasses, 92% (n=24) of the patients reported never requiring glasses for daytime driving and 92% (n=24) of the subjects that drove at night reported never requiring glasses. When asked about intermediate tasks (eg, using the computer), 24% (n=6) of the subjects reported frequently or always requiring glasses and 50% (n=13) reported never using glasses for this activity. When asked about use of spectacles for mobile phone use, 38% (n=10) of the subjects reported never requiring glasses and 38% (n=10) of the subjects also reported frequent or consistent use of glasses with mobile phone use.
 |
Table 2 Results from the Subject Questionnaire Evaluating Spectacle Independence at the 4-Month Postoperative Visit are Summarized |
Discussion
This prospective, single-arm clinical study evaluated visual outcomes in patients with mild glaucoma bilaterally implanted with a non-diffractive EDOF IOL. To our knowledge, this is the first study to evaluate results of the Vivity non-diffractive EDOF IOL in eyes with glaucoma. EDOF, or extended range-of-vision (EROV) lenses, represent a growing category of IOL technology. While EDOF IOLs do not offer the near vision of a multifocal IOL, the purported benefits include a continuous range of vision from distance to intermediate and more favorable visual disturbance profile with reduced photic phenomena.1,17 Further, as light is not allocated to a specific focal point but is broadened across a continuous range of vision, EDOF IOLs are thought to provide a larger “landing zone” and forgive the imperfections associated with IOL power calculations.18 The Vivity EDOF IOL, in particular, has been shown to offer a favorable visual disturbance profile with reduced photic phenomena, likely owing to the non-diffractive properties of the IOL. A recently published study by Bala et al7 evaluating clinical outcomes with the Vivity IOL in comparison to a monofocal IOL (Alcon SN60WF) demonstrated results showing a comparable visual disturbance profile based on patient-reported outcomes.
The visual outcomes in this study were favorable and consistent with prior studies7,10 evaluating the Vivity EDOF IOL. In the present study, subjects achieved favorable distance and intermediate vision coinciding with reduced spectacle dependence. The mean UDVA was 0.03 ± 0.12 (~20/20) with 65% of patients achieving ≥20/20 UDVA and the mean UIVA was 0.17 ± 0.13 (~20/30) with 77% of patients achieving 20/32 UIVA or better. These outcomes were reflected in the questionnaire with 92% of patients reporting that they never needing glasses for driving and 50% of the patients reporting they never required glasses for computer work. At near, the mean UNVA was 0.31 ± 0.17 (~J3 or 20/40) with 65% of subjects achieving J3 or better. Overall, these outcomes highlight the extended range of vision conferred by the Vivity EDOF IOL and demonstrate that patients with mild glaucoma can achieve similar visual outcomes.
It is well established by prior work that patients with glaucoma have a reduction in contrast sensitivity.5 Owing to the reduction in contrast sensitivity, presbyopia-mitigating IOL options such as trifocal, bifocal and EDOF IOLs have traditionally been avoided in patients with glaucoma. However, many of the current or emerging presbyopia-mitigating IOL options employ novel optical technology such as the non-diffractive, wavefront-shaping IOL evaluated in the present study, offering an improvement in contrast sensitivity and reduced photic phenomena compared to earlier multifocal IOL options.1,2,7 In the present study, the contrast sensitivity results were very encouraging with a mean CS value as measured via Pelli-Robson of 1.78 ± 0.17. Although no control group in the present study, the CS results compare favorably to prior work in which CS values of monofocal IOLs ranged from 1.6 to 1.7.13,14,19 Further, these results align with prior work evaluating the Vivity EDOF IOL in healthy patients and highlight the absence of meaningful CS loss with this IOL.7
The advancements in IOL technology over time have allowed the use of presbyopia-mitigating IOL implantation such as EDOF IOLs to evolve and expand beyond eyes without co-existing ocular disease.20,21 This is particularly true for EDOF IOLs, which are thought to be more forgiving and are associated with reduced photic phenomena compared to multifocal IOLs. A recent paper by Jeon et al22 evaluated the Vivity EDOF IOL in eyes with low-grade epiretinal membrane and reported favorable results. In this study, eyes with low-grade ERM and history of Vivity implantation were compared with an age-matched group of eyes implanted with the Vivity IOL without ERM. Although a single study with limited follow-up, the results were largely similar between the two groups. Given the recent introduction of the Vivity IOL, further study is warranted to evaluate whether the IOL would be tolerated in other situations of pre-existing ocular disease.
This study is not without limitations. There was no control group. The sample size was relatively small, limiting the ability to compare toric versus non-toric IOL outcomes in this study. This study was limited to eyes with mild stage of glaucoma, and it remains unclear how this lens would perform in eyes with more advanced stage of disease. Pupillometry was not performed in this study and a prior study by Arrigo et al16 reported a correlation between pupil size and photic phenomena such as glare and haloes. Some of the eyes were implanted with a trabecular microbypass stent at the time of cataract surgery; however, multiple studies23,24 have demonstrated the refractive neutrality of the trabecular microbypass stent and this would not be expected to impact visual or refractive outcomes. Finally, the Pelli-Robson chart only evaluates the contrast sensitivity score at a spatial frequency of 1 cycle-per-degree. Despite these limitations, this is the first study to evaluate the use of the Vivity EDOF IOL in eyes with glaucoma.
Conclusion
Although compounded contrast sensitivity loss has long been a concern with implanting presbyopia-mitigating IOLs in patients with glaucoma, this study supports the use of the Vivity IOL, a presbyopia-mitigating EDOF IOL with novel optical properties. The favorable outcomes outlined in this study indicate that patients with mild stage of glaucoma can achieve satisfactory visual outcomes with the Vivity non-diffractive, wavefront-shaping EDOF IOL.
Data Sharing Statement
The data set collected and analyzed for this present study is available from the corresponding author per reasonable request.
Acknowledgments
This study was funded by an investigator-initiated trial grant from Alcon and was registered with clinicaltrials.gov (NCT04670575).
Disclosure
Drs. Shafer, Berdahl are consultants and speakers for Alcon. Dr Berdahl also reports personal fees from AbbVie, Aerpio, Alcon, Aldeyra, Aurea Medical, Aurion Biotech/CorneaGen, Bausch and Lomb, Dakota Lions Eye Bank, Elios Vision INC, Equinox, Expert Opinion, Glaukos, Gore, Imprimis, Interfeen, iRenix, Incta Pharmaceuticals, JNJ, Kala, Kedalion, MELT Pharmaceuticals, MicroOptx, New World Medical, Ocular Surgical Data, Ocular Theraputix, Omega Ophthalmic, Orasis, Oyster Point, RxSight, Santeen, Sight Sciences, Surface Inc, Tarsus, Tear Clear, Vertex Ventures, ViaLase, Vittamed, Vance Thompson Vision, Verana Health, Versa Biologics, Visionary Ventures, Visus, and Zeiss, outside the submitted work. Drs Terveen and Ferguson report grant supports from Alcon. Dr Wilson has no relevant disclosures to report for this work.
References
1. Schallhorn JM, Pantanelli SM, Lin CC, et al. Multifocal and accommodating intraocular lenses for the treatment of presbyopia: a report by the American Academy of Ophthalmology. Ophthalmology. 2021;128(10):1469–1482. doi:10.1016/j.ophtha.2021.03.013
2. Rampat R, Gatinel D. Multifocal and extended depth-of-focus intraocular lenses in 2020. Ophthalmology. 2021;128(11):e164–e185. doi:10.1016/j.ophtha.2020.09.026
3. Shah M. Micro-invasive glaucoma surgery – an interventional glaucoma revolution. Eye Vision. 2019;6(1):29. doi:10.1186/s40662-019-0154-1
4. Lavia C, Dallorto L, Maule M, Ceccarelli M, Fea AM, Virgili G. Minimally-invasive glaucoma surgeries (MIGS) for open angle glaucoma: a systematic review and meta-analysis. PLoS One. 2017;12(8):e0183142. doi:10.1371/journal.pone.0183142
5. Ichhpujani P, Thakur S, Spaeth GL. Contrast Sensitivity and Glaucoma. J Glaucoma. 2020;29(1):71–75. doi:10.1097/IJG.0000000000001379
6. Kohnen T. Nondiffractive wavefront-shaping extended range-of-vision intraocular lens. J Cataract Refract Surg. 2020;46(9):1312–1313. doi:10.1097/j.jcrs.0000000000000247
7. Bala C, Poyales F, Guarro M, et al. Multicountry clinical outcomes of a new nondiffractive presbyopia-correcting IOL. J Cataract Refract Surg. 2022;48(2):136–143. doi:10.1097/j.jcrs.0000000000000712
8. Folden DV, Wong JR. Visual outcomes of an enhanced UV protected light adjustable lens using a novel co-managed, open-access methodology. Clin Ophthalmol. 2022;Volume 16:2413–2420. doi:10.2147/OPTH.S378525
9. Rocha KM. Extended depth of focus IOLs: the next chapter in refractive technology? J Refract Surg. 2017;33(3):146–149. doi:10.3928/1081597X-20170217-01
10. Kohnen T, Petermann K, Böhm M, et al. Nondiffractive wavefront-shaping extended depth-of-focus intraocular lens: visual performance and patient-reported outcomes. J Cataract Refract Surg. 2022;48(2):144–150. doi:10.1097/j.jcrs.0000000000000826
11. Shafer BM, McCabe C, Reiser H, Newsom TH, Berdahl J. The REVIVE study: long term outcomes of a novel non-diffractive extended vision IOL versus monofocal control IOL. Clin Ophthalmol. 2022;16:3945–3950. doi:10.2147/OPTH.S390380
12. Gedde SJ, Vinod K, Wright MM, et al. Primary open-angle glaucoma preferred practice pattern®. Ophthalmology. 2021;128(1):P71–P150. doi:10.1016/j.ophtha.2020.10.022
13. Altemir-Gomez I, Millan MS, Vega F, et al. Comparison of visual and optical quality of monofocal versus multifocal intraocular lenses. Eur J Ophthalmol. 2020;30(2):299–306. doi:10.1177/1120672119827858
14. Hall CD, Barnes CS, Gutherie AH, Lynch MG. Visual function and mobility after multifocal versus monofocal intraocular lens implantation. Clin Exp Optom. 2022;105(1):70–76. doi:10.1080/08164622.2021.1896337
15. Morlock R, Wirth R, Tally SR, Garufis C, Heichel CW. Patient-reported spectacle Independence questionnaire (PRSIQ): development and validation. Am J Ophthalmol. 2017;178:101–114. doi:10.1016/j.ajo.2017.03.018
16. Arrigo A, Gambaro G, Fasce F, Aragona E, Figini I, Bandello F. Extended depth-of-focus (EDOF) AcrySof® IQ Vivity® intraocular lens implant: a real-life experience. Graefes Arch Clin Exp Ophthalmol. 2021;259(9):2717–2722. doi:10.1007/s00417-021-05245-6
17. Ruiz-Mesa R, Abengózar-Vela A, Ruiz-Santos M. A comparative study of the visual outcomes between a new trifocal and an extended depth of focus intraocular lens. Eur J Ophthalmol. 2018;28(2):182–187. doi:10.5301/ejo.5001029
18. Kohnen T, Suryakumar R. Extended depth-of-focus technology in intraocular lenses. J Cataract Refract Surg. 2020;46(2):298–304. doi:10.1097/j.jcrs.0000000000000109
19. Nabh R, Ram J, Pandav SS, Gupta A. Visual performance and contrast sensitivity after phacoemulsification with implantation of aspheric foldable intraocular lenses. J Cataract Refract Surg. 2009;35(2):347–353. doi:10.1016/j.jcrs.2008.10.043
20. Baartman BJ, Karpuk K, Eichhorn B, et al. Extended depth of focus lens implantation after radial keratotomy. Clin Ophthalmol. 2019;13:1401–1408. doi:10.2147/OPTH.S208550
21. Do\lowiec-Kwapisz A, Misiuk-Hojlo M, Piotrowska H. Cataract surgery after radial keratotomy with non-diffractive extended depth of focus lens implantation. Medicina. 2022;58(5):689. doi:10.3390/medicina58050689
22. Jeon S, Choi A, Kwon H. Clinical outcomes after implantation of extended depth-of-focus AcrySof® Vivity® intraocular lens in eyes with low-grade epiretinal membrane. Graefe’s Arch Clin Exp Ophthalmol. 2022;260:1–6.
23. López-Caballero C, Sánchez-Sánchez C, Puerto B, Blázquez V, Sánchez-Pina JM, Contreras I. Refractive outcomes of toric intraocular lens in combined trabecular micro bypass stent implantation and cataract surgery in glaucomatous eyes. Int Ophthalmol. 2022;42(9):1–8.
24. Scott RA, Ferguson TJ, Stephens JD, Berdahl JP. Refractive outcomes after trabecular microbypass stent with cataract extraction in open-angle glaucoma. Clin Ophthalmol. 2019;13:1331–1340. doi:10.2147/OPTH.S206619
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

