Back to Journals » Journal of Pain Research » Volume 15
Comparative Study Between Early versus Late Intraperitoneal Administration of Either Bupivacaine/Tramadol or Bupivacaine/Dexmedetomidine for Perioperative Analgesia in Abdominal Laparoscopic Cancer Surgeries: A Prospective Randomized Study
Authors Shaker EH , Soliman MS, Hanafy A, Elsabeeny WY
Received 1 June 2022
Accepted for publication 29 September 2022
Published 18 October 2022 Volume 2022:15 Pages 3233—3243
DOI https://doi.org/10.2147/JPR.S376681
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jinlei Li
Ehab H Shaker,1 Mahmoud S Soliman,2 Ayman Hanafy,3 Walaa Y Elsabeeny1
1Department of Anesthesia, Intensive Care and Pain Management, National Cancer Institute, Cairo University, Cairo, Egypt; 2Department of Anesthesia, Surgical ICU and Pain Management, Faculty of Medicine, Cairo University, Cairo, Egypt; 3Department of Surgical Oncology, National Cancer Institute, Cairo University, Cairo, Egypt
Correspondence: Walaa Y Elsabeeny, Department of Anesthesia and Pain management, National Cancer Institute, Kasr Al Eini Street, Fom El Khalig, Cairo, Egypt, Tel +20 1007798466, Email [email protected]
Objective: Several modalities for analgesia after laparoscopic procedures have been used. This study aimed to investigate the efficacy of early versus late bupivacaine/tramadol combination and bupivacaine/dexmedetomidine combination in analgesia for laparoscopic cancer surgeries.
Methods: A total of 100 patients of both genders scheduled for elective laparoscopic cancer surgeries were included. Patients were randomly assigned to one of four groups each comprises 25 patients. Group 1: early bupivacaine/tramadol, Group 2: late bupivacaine/tramadol, Group 3: early bupivacaine/dexmedetomidine, and Group 4: late bupivacaine/dexmedetomidine. Early groups received the intraperitoneal instillation before start of surgery and late groups received the instillation after completion of surgery. Perioperative heart rate (HR) and mean arterial blood pressure (MAP) were recorded. The degree of postoperative pain was measured at rest and with cough using Visual analogue scale (VAS) score at 2, 4, 6, 12, 18 and 24 h after surgery. In addition, the total intraoperative fentanyl and postoperative morphine doses were calculated.
Results: Both late bupivacaine/tramadol, bupivacaine/dexmedetomidine groups had longer time to receive first analgesic requirement (13.4± 3.9, 11.3± 3.9 h) respectively as compared to early bupivacaine/tramadol, bupivacaine/dexmedetomidine groups (9.8± 3.6, 8.4± 2.8 h), respectively. Between each early and late group, intraoperative fentanyl consumption was higher for the late groups (75± 22.8, 73± 21.55μg) versus (32.7± 10.9, 37.5± 13.3 μg), respectively. As regards to rescue analgesic requirements, both early bupivacaine/tramadol and bupivacaine/dexmedetomidine groups consumed more analgesics (5.2± 2.0 and 6.1± 1.8 mg) as compared to the late groups (3.2± 0.8 and 4.3± 1.5 mg), respectively. The four groups were comparable for their perioperative HR and MAP values.
Conclusion: Intraperitoneal instillation of bupivacaine/tramadol and bupivacaine/dexmedetomidine could be considered an effective route for analgesic administration during laparoscopic cancer surgeries. Early instillation reduced the intraoperative opioid consumption and late instillation resulted in reduced postoperative opioid consumption.
Clinical Trial Registration: https://clinicaltrials.gov/ct2/show/NCT04813016.
Keywords: intraperitoneal analgesia, tramadol, dexmedetomidine, bupivacaine, laparoscopic surgeries
Introduction
Recently, laparoscopic procedures have gained popularity for both surgeons and anesthetists. This popularity is owed to the several merits laparoscopic surgeries offer, as enhancing postoperative recovery, lowering the incidence of complications, and allowing for early mobilization thus help in earlier home discharge with reduced hospital stay and costs.1 Previous studies investigated the possibility of lower postoperative pain associated with laparoscopic procedures; however, it is not totally pain free.2 Some laparoscopic procedures carry the risk of more intense pain with increased analgesic requirements in the immediate postoperative period than after open laparotomies.3,4
Understanding the difference in pain generators between laparotomy and laparoscopy gives an idea that helps in the pain control of each of them. While parietal pain is the main generator in laparotomies, visceral pain is predominant after laparoscopic surgeries. This visceral pain is caused by the stretching of intra-abdominal cavity, peritoneal inflammation and phrenic nerve irritation caused by residual carbon dioxide in the peritoneal cavity resulting in postoperative abdominal and shoulder pain after laparoscopy.2,5 Few studies reported the effectiveness of intraperitoneal (IP) administration of some drugs for pain relief after laparoscopic surgery.6,7 Published studies are heterogeneous and often lack appropriate controls, so definitive conclusion cannot be made regarding its value and effectiveness.
Dexmedetomidine is an α2-adrenergic agonist frequently used in anesthesia due to its sedative, anxiolytic, analgesic, neuroprotective and anesthetic sparing effect. It also provides excellent sedation, anxiolysis, analgesia and sympatholysis.8 In addition, the high selectivity of dexmedetomidine to α2-receptors favored its widespread use in regional anesthesia practice and local nerve block techniques.9 The descending inhibitory pathway significantly contributes to the modulation of pain by controlling impulse transmission. This action is mediated by the noradrenergic neurons descending through the dorsolateral funiculus from the brainstem to the dorsal horn. Like all adrenergic agonists, dexmedetomidine has a significant antinociceptive activity through both a central action on the brainstem and a spinal action on the substantia gelatinosa of the dorsal horn.10
Tramadol is a synthetic opioid treating moderate to moderately severe pain. It exists as a racemic mixture, the positive enantiomer inhibits serotonin reuptake while the negative enantiomer inhibits noradrenaline reuptake, by binding to and blocking the transporters. In addition, tramadol has also been shown to act as a serotonin-releasing agent. Both enantiomers are agonists of the μ-opioid receptor and its metabolite O-demethylate, is 6 times more potent than tramadol itself. All these effects work synergistically to induce analgesia.11–14
The aim of this study is to examine and compare the effect of both early and late intraperitoneal administration of both bupivacaine/tramadol and bupivacaine/dexmedetomidine on the effectiveness of perioperative analgesia and the requirement of postoperative rescue analgesics after laparoscopic surgery for abdominal cancer surgeries.
Methods
This double blinded (participant, care provider) study was held in the National Cancer Institute, Cairo University, in the period from March 2021 to April 2022 after the approval of the Institutional Review Board and was prospectively registered at ClinicalTrials.gov NCT04813016. The study followed the standards of Declaration of Helsinki. Un-identified study data generated and analyzed during this study (clinical data and results) are available upon reasonable request through contacting the corresponding author following the publication and for a period of 2 years. The study was designed to investigate the analgesic efficacy and effect of timing of intraperitoneal instillation of either tramadol or dexmedetomidine added to bupivacaine in patients undergoing laparoscopic abdominal cancer surgeries.
One hundred patients aged from 18 to 65 with American Society of Anesthesiologists (ASA I and II) of both genders scheduled for elective abdominal laparoscopic cancer surgery were included after a written informed consent was obtained. Patients with hepatic, renal and cardiac diseases, those with extensive intraperitoneal adhesions, a history of chronic pain medications, drug allergy, change of surgical plan (intraoperative lavage of more than 500mL, prolonged surgery more than 3 hours, complicated surgical cases converted to open laparotomies or surgical re-exploration in less than 24 hours) were excluded from the study.
All included patients were randomly allocated to one of four groups – each comprises 25 patients by means of computer-generated sealed envelopes, which were opened in the operating theatre.
- Group 1 (early tramadol): patients received intraperitoneal instillation of 50 mL bupivacaine 0.25% mixed with tramadol 150mg immediately after creation of a pneumoperitoneum.
- Group 2 (late tramadol): patients received intraperitoneal instillation of 50 mL bupivacaine 0.25% mixed with tramadol 150mg after completion of surgery and before trocars removal.
- Group 3 (early dexmedetomidine): patients received intraperitoneal instillation of 50mL bupivacaine 0.25% mixed with dexmedetomidine (1µg/kg) after creation of a pneumoperitoneum.
- Group 4 (late dexmedetomidine): patients received intraperitoneal instillation of 50mL bupivacaine 0.25% mixed with dexmedetomidine (1µg/kg) after completion of surgery and before trocars’ removal.
All the operative procedures were laparoscopic colectomies which were operated upon by the same colorectal surgery team with the same standardized technique to minimize bias. Standard procedures for laparoscopic surgeries were used in all patients, the peritoneal cavity was accessed through a 1-cm umbilical incision. A pneumoperitoneum was created using carbon dioxide with an insufflation pressure of 15 mmHg with a maximum flow of 2 L/min. Flow and pressure were maintained electronically throughout the procedure. Local anesthetic infiltration was applied at all port sites before skin incision for port introduction. Four trocars were inserted into the abdominal cavity with the following order: optic umbilical trocar (10 mm), right iliac fossa midclavicular line (12mm), right hypochondrial midclavicular line (5mm) and left iliac fossa mid clavicular line (5 mm).
Peritoneal Topical Analgesia
In Groups 1 and 3, immediately after placement of the first two trocars and creation of the pneumoperitoneum a 50 mL of the analgesic solution (either 0.25% bupivacaine with 150 mg tramadol in Group 1 or 0.25% bupivacaine with dexmedetomidine 1 µg/kg in Group 3) was sprayed in the abdominal cavity.
In Groups 2 and 4, at the end of the operation, 50mL of analgesic solution (either 0.25% bupivacaine with 150 mg tramadol in Group 2 or 0.25% bupivacaine with dexmedetomidine 1 µg/kg in Group 4) was sprayed in the abdominal cavity.
The instillation at the operative bed was guided by the camera and instilled uniformly into the peritoneal cavity by the surgeon using nelton tube 16 fr into left and right paracolic gutter (10 mL on each side), subdiaphragmatic spaces (10 mL on each side) and pelvis (10 mL).
A head-down position of 15–20 degrees was maintained for 2 minutes in all patients after intraperitoneal installation of the analgesic solution.
General Anesthesia
All patients received 2 mg midazolam intravenously in the holding area before transfer to the operating room. Anesthesia was induced with 2mg/kg intravenous propofol, 0.5 mg/kg intravenous atracurium and 2µg/kg intravenous fentanyl. In addition, as a part of the multimodal analgesic regimen all patients received dexamethasone 8 mg IV. After tracheal intubation, patient received mechanical ventilation to keep end tidal CO2 between 35 and 45 mmHg, general anesthesia was maintained using inhalational anesthesia with 1.5–2.0% sevoflurane (end-tidal concentration) and top-up doses of muscle relaxant as needed. Intraoperative hemodynamics were measured and recorded. Rescue fentanyl (25 µg) per dose was given in case of elevation of HR or MAP ≥20% above the measured baseline. At the end of surgery, reversal of residual muscle relaxant was done as needed.
Outcome Measures
The primary endpoint was the total analgesic requirements in the first 24 hours. Secondary endpoints were intraoperative fentanyl consumption, the degree of postoperative pain (VAS) at rest, VAS with cough, blood pressure and heart rate monitoring.
Before the induction of anesthesia, patients were informed how to use the visual analogue scale (VAS) as measurement of pain severity: the scale ranged from 0 (no pain) to 10 (worst possible pain). For routine postoperative analgesia, all patients received 1gm intravenous (IV) paracetamol every 8 hours alternating with ketorolac 30 mg IV every 12 hours. After assessment of pain scores, a bolus of morphine 3mg was administered intravenously in cases experiencing severe pain (VAS score ≥4). The total consumption of rescue analgesics (morphine) was recorded for all patients.
Both VAS at rest and with cough were assessed at 2, 4, 6, 12, 18 and 24 h after surgery. Hemodynamic variables including mean arterial blood pressure and heart rate were also measured and recorded. Complications as nausea, vomiting, hypotension and bradycardia were reported. In patients who experienced nausea or vomiting, ondansetron 4 mg was given. Data was collected by a junior medical staff member. Both the patients and the medical staff were blinded to the group assignments.
Statistical Analysis
Calculation of sample size was based on a previous study by Shukla et al,15 who reported the average VAS score at 6 hours (2.78±1.22 and 2.02±0.20) for tramadol and dexmedetomidine respectively. Using power 80% and 5% significance level we needed to study 22 patients in each group. This number was increased to a sample size of 25 to adjust for using a nonparametric test. Sample size calculation was achieved using G power.
Numerical data was presented as mean (s.d.), while categorical data was presented as number and percentage. A P value <0.050 was considered statistically significant. One-way ANOVA was done followed by Bonferroni post hoc test for normally distributed data, while Kruskal–Wallis test was used for not normally distributed data. For group comparisons and time points, a significant difference was considered P<0.0167 (Bonferroni error correction). The independent primary variable was assumed to be the analgesic consumption as the pain scores were influenced by the application of analgesics according to on-demand management, these values were compared as secondary variables. SPSS version 12.0 (SPSS, Chicago, Illinois, USA) was used for statistical analysis.
Results
One hundred twenty-seven patients referred to anaesthesia assessment clinic were assessed for eligibility, 11 patients did not meet the criteria, and 8 patients refused to participate in the study (Figure 1). One hundred and eight patients were allocated into four groups, eight patients were excluded due to change in the surgical plan and 100 patients were analysed (25 patients in each group). Patients’ demographic data (age, sex, height, weight and BMI), clinical characteristics (hypertension, DM, medication and chemotherapy) and duration of surgery were comparable among the four groups (Table 1).
 |
Table 1 Patients’ Demographic Data, Clinical Characteristics, and Duration of Surgery |
 |
Figure 1 Patients’ CONSORT flow chart. Notes: Adapted from Schulz KF, Altman DG, Moher D, CONSORT Group. CONSORT 2010 Statement: Updated Guidelines for Reporting Parallel Group Randomised Trials. PLoS Med. 2010;7(3):e1000251.25 Copyright: © 2010 Schulz et al. Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/legalcode). https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1000251. |
MAP and HR values were insignificantly different among the four groups at all time measurements (Figures 2 and Figure 3).
 |
Figure 2 Perioperative heart rate values. Abbreviations: HR, heart rate; G1, early tramadol group; G2, late tramadol group; G3, early dexmedetomidine group; G4, late dexmedetomidine group. |
Intraoperative fentanyl requirement was significantly different among the four groups. All patients in Groups 2 and 4 needed intraoperative rescue fentanyl doses compared to nine patients in Group 1 and 8 patients in Group 3 (P value <0.001). Average intraoperative fentanyl requirement was significantly higher in Group 2 (75±22.8µg) compared to Groups 1 and 3 (32.7±10.9, 37.5±13.3 µg) respectively and in Group 4 (73±21.55µg) compared to Groups 1 and 3 (32.7±10.9, 37.5±13.3 µg) respectively (P value <0.001) (Table 2).
 |
Table 2 Intraoperative Fentanyl, Postoperative Morphine Consumption, and First Time to Receive Morphine |
There was no statistically significant difference among the four groups regarding VAS at rest and VAS with cough at all time measurements (Table 3) (Figures 4 and Figure 5).
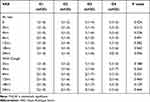 |
Table 3 Postoperative VAS Scores at Rest and with Cough |
 |
Figure 4 Visual analogue scale score at rest. °Outliers. *Extreme outliers. Abbreviation: VAS, visual analogue scale. |
 |
Figure 5 Visual analogue scale score with cough. °Outliers, *Extreme outliers. Abbreviation: VAS, visual analogue scale. |
Time of first analgesic requirement was significantly different among the four groups, where time of first analgesic requirement was significantly longer in Group 2 (13.4±3.9 h) compared to Groups 1 and 3 (9.8±3.6 and 8.4± 2.8 h, respectively), and in Group 4 (11.3±3.9 h) compared to Groups 1 and 3 (9.8±3.6 and 8.4± 2.8 h, respectively) (P<0.001), while there was no significant difference between Groups 1, 3 and Groups 2, 4 (P>0.001) (Table 2).
Total morphine requirement was significantly lower in Group 2 (3.2± 0.8 mg) compared to Groups 1 and 3 (5.2± 2.0 and 6.1±1.8 mg), respectively (P value <0.001). In the same time, Group 4 showed a statistically significant lower consumption compared to Group 3 (4.3± 1.5 and 6.1± 1.8 mg), respectively (P value <0.001) (Table 2).
No statistically significant difference was found regarding nausea (P value = 0.906) and vomiting (P value = 0.686) among the four studied groups (Table 4).
 |
Table 4 Incidence of Nausea and Vomiting in the Studied Group |
Discussion
Although investigating intraperitoneal analgesic instillation techniques in different laparoscopic procedures were previously done, evaluating this technique in laparoscopic cancer resection procedures is still limited. This study demonstrated that patients undergoing laparoscopic cancer surgeries can experience significant postoperative pain that requires postoperative opioid analgesics, and this may be related to the relatively longer duration of pneumo-peritoneum and complexity of the procedures done. To ensure adequate analgesia throughout the study, the authors applied a multimodal analgesic regimen to all included patients using dexamethasone given with induction of general anesthesia, intraoperative fentanyl and postoperative paracetamol/NSAID, in addition to rescue opioid analgesic (morphine sulphate) in cases with VAS ≥4. This multimodal regimen with perioperative opioids comes in contrast to a trial conducted by Bisgaard et al on patients undergoing laparoscopic cholecystectomy where it was suggested that an opioid sparing multimodal regimen can be applied efficiently to control postoperative pain and short acting opioids can be added only if needed. However, such difference might be related to the difference in procedures’ nature.4 In this study, it was observed that pre-emptive administration of LA with adjuvant drugs resulted in reduced intra-operative analgesic requirements while its administration at the end of surgery resulted in longer time to receive first dose of postoperative opioids and decreased opioid consumption after surgery. Additionally, intraperitoneal administration of bupivacaine/tramadol resulted in comparable postoperative analgesia when compared to bupivacaine/dexmedetomidine combination.
Investigating the effect of intraperitoneal instillation of local anesthetics has proven its efficacy in improving perioperative pain and reducing opioid consumption.7 Combination of local anesthetics with additives results in better analgesic outcome. Dexmedetomidine is a sedative analgesic drug that is used as an adjuvant to reduce anesthetic and analgesic requirements.8 The analgesic effect of α2 agonists is still not entirely explained; however, it affects both supraspinal and spinal sites modulating nociceptive transmission. Additionally it is thought to have a peripheral action through acting on peripheral α2 adrenoceptors.16 Bupivacaine/dexmedetomidine combination showed a superior effect to bupivacaine only administration during different laparoscopic surgeries.9,17–19
Oza et al compared the antinociceptive effect of bupivacaine versus bupivacaine/dexmedetomidine combination for intraperitoneal instillation in laparoscopic cholecystectomy procedures. They stated that adding dexmedetomidine resulted in prolonged analgesic effect and lower postoperative analgesic consumption.9 One more study by Namrata et al reported same results with different local anesthetic volume.18 Rokhgireh et al further investigated the efficacy of intraperitoneal instillation of analgesic drugs in patients undergoing laparoscopic procedures for endometriosis. They concluded that compared to normal saline both bupivacaine and bupivacaine/dexmedetomidine combination had superior analgesic profile, additionally bupivacaine/dexmedetomidine had a superb effect with prolonged postoperative analgesia and reduced postoperative analgesic requirements.19
Furthermore, in a group of patients similar to the current study, Fares et al evaluated the efficacy of laparoscopic instillation of saline versus bupivacaine versus bupivacaine/dexmedetomidine combination in cancer patients undergoing laparoscopic colorectal resection surgeries. Their results stated that both saline and bupivacaine alone were comparable with inferior analgesia to bupivacaine/dexmedetomidine combination. They also reported average time needed to receive first analgesic opioid in the bupivacaine/dexmedetomidine group was (9.50± 7.5) hours, while in the current study, it was reported to be (8.4±2.8) hours in the early bupivacaine/dexmedetomidine group compared to (11.3±3.9) hours late bupivacaine/dexmedetomidine group.
Moreover, adding tramadol as an analgesic drug that acts as an adjuvant to local anesthetics during intraperitoneal installation can augment the analgesic effect of local anesthetics, this may be attributed to that it exerts its analgesic action through a variety of different targets on the noradrenergic, serotoninergic, and opioid receptors systems.11 Studies investigating the intraperitoneal administration of tramadol alone without a local anesthetic although showed superior analgesic effect to saline instillation but had less comparable results when compared to intravenous tramadol.12,20 On the other hand, the adjuvant effect of local anesthetic/analgesic combination was further investigated by Jamal et al who compared either bupivacaine or tramadol alone versus the two drugs combination recording that the adjuvant effect of bupivacaine/tramadol had a superior analgesic profile with significant reduction in opioid consumption when compared to either drug alone.21 Adding tramadol to local anesthetic (ropivacaine) resulted in reduced postoperative pain score as well as reduced postoperative opioid consumption when compared to local anesthetic alone or saline.14,22
When Yadava et al compared bupivacaine/tramadol to bupivacaine/magnesium combination, they reported the superiority of magnesium to tramadol. However, after going through their posted results, it was noticed that still tramadol can be considered as an effective adjuvant as the average time to request analgesia was approximately 5 hours, and the analgesic used for rescue analgesia was paracetamol not opioid. On the other hand, in this study, perioperative analgesia was offered as a multimodal regimen given to all patients, with paracetamol and NSAIDs given as an integral part of the protocol and morphine used as the rescue analgesic.13
Deshmukh et al compared bupivacaine/dexmedetomidine versus bupivacaine/tramadol instillation during laparoscopic cholecystectomy. Their results showed that adding dexmedetomidine to bupivacaine provided better analgesic profile than adding tramadol.23 In another two studies done by Shukla et al and Mukkavilli et al, they had different results to the current study results where they assessed the analgesic efficacy of bupivacaine versus bupivacaine/dexmedetomidine versus bupivacaine/tramadol combination. They recorded that drug combination was superior to single agent and that bupivacaine/dexmedetomidine had a superior analgesic profile.15,24 We owed such difference in the previous studies compared to the current study results to the difference in procedure nature, time of procedure, different analgesic regimen as well as the higher dose of tramadol we used.
Conclusion
In the current study, it was observed that early intraperitoneal instillation of bupivacaine/tramadol and bupivacaine/dexmedetomidine combination resulted in significant reduction in intraoperative fentanyl consumption when compared to late instillation. Additionally, the late intraperitoneal instillation of bupivacaine/tramadol and bupivacaine/dexmedetomidine combination resulted in delayed first dose of postoperative morphine requirement with reduced total postoperative morphine consumption.
Significance
This study evaluates the efficacy of early versus late intraperitoneal instillation of either bupivacaine/tramadol combination or bupivacaine/dexmedetomidine combination in analgesia for laparoscopic cancer surgeries.
Funding
There was no external funding for this work.
Disclosure
The authors declare that they have no conflicts of interest in relation to this work.
References
1. Heikkinen T, Msika S, Desvignes G, et al. Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol. 2005;6(7):477–484.
2. Sao CH, Chan-Tiopianco M, Chung KC, et al. Pain after laparoscopic surgery: focus on shoulder-tip pain after gynecological laparoscopic surgery. J Chin Med Assoc. 2019;82(11):819–826. doi:10.1097/JCMA.0000000000000190
3. Ekstein P, Szold A, Sagie B, Werbin N, Klausner JM, Weinbroum AA. Laparoscopic surgery may be associated with severe pain and high analgesia requirements in the immediate postoperative period. Ann Surg. 2006;243(1):41–46. doi:10.1097/01.sla.0000193806.81428.6f
4. Bisgaard T, Warltier DC. Analgesic treatment after laparoscopic cholecystectomy. Anesthesiology. 2006;104(4):835–846. doi:10.1097/00000542-200604000-00030
5. Golubović S, Golubović V, Cindrić-Stančin M, Tokmadžić VS. Intraperitoneal analgesia for laparoscopic cholecystectomy: bupivacaine versus bupivacaine with tramadol. Coll Antropol. 2009;33(1):299–302.
6. Chou YJ, Ou YC, Lan KC, Jawan B, Chang SY, Kung FT. Preemptive analgesia installation during gynecologic laparoscopy: a randomized trial. J Minim Invasive Gynecol. 2005;12(4):330–335. doi:10.1016/j.jmig.2005.05.005
7. Marchand G, Ware K, Govindan M, et al. A systematic review and meta-analysis of intraperitoneal bupivacaine in laparoscopic gynecologic surgery. J Pain Res. 2021;14:2699–2707. doi:10.2147/JPR.S326145
8. Gertler R, Brown C, Donald MH, Erin SN. Dexmedetomidine-a novel sedative analgesic agent. Bayl Univ Med Cent Proc. 2001;14(1):13–21. doi:10.1080/08998280.2001.11927725
9. Oza V, Parmar V, Badheka J, Nanavati D, Taur P, Rajyaguru A. Comparative study of postoperative analgesic effect of intraperitoneal instillation of dexmedetomidine with bupivacaine and bupivacaine alone after laparoscopic surgery. J Minim Access Surg. 2016;12(3):260. doi:10.4103/0972-9941.181370
10. Damien J, Luana C, Bellei-Rodriguez C-E, Marchand S. Pain modulation: from conditioned pain modulation to placebo. Int Rev Neurobiol. 2018;2018(139):255–296.
11. Vazzana M, Andreani T, Fangueiro J, et al. Tramadol hydrochloride: pharmacokinetics, pharmacodynamics, adverse side effects, co-administration of drugs and new drug delivery systems. In: Biomedicine and Pharmacotherapy. Elsevier Masson SAS; Vol. 70, 2015:234–238.
12. Akinci SB, Ayhan B, Aycan IO, et al. The postoperative analgesic efficacy of intraperitoneal tramadol compared to normal saline or intravenous tramadol in laparoscopic cholecystectomy. Eur J Anaesthesiol. 2008;25(5):375–381. doi:10.1017/S0265021508003694
13. Yadava A, Rajput SK, Katiyar S, Jain RK. A comparison of intraperitoneal bupivacaine-tramadol with bupivacaine-magnesium sulphate for pain relief after laparoscopic cholecystectomy: a prospective, randomised study. Indian J Anaesth. 2016;60(10):757–762. doi:10.4103/0019-5049.191696
14. Kumari A, Acharya B, Ghimire B, Shrestha A. Post-operative analgesic effect of intraperitoneal ropivacaine with or without tramadol in laparoscopic cholecystectomy. Indian J Anaesth. 2020;64(1):43. doi:10.4103/ija.IJA_526_19
15. Shukla U, Prabhakar T, Malhotra K, Srivastava D, Malhotra K. Intraperitoneal bupivacaine alone or with dexmedetomidine or tramadol for post-operative analgesia following laparoscopic cholecystectomy: a comparative evaluation. Indian J Anaesth. 2015;59(4):234–239. doi:10.4103/0019-5049.155001
16. Nakamura M, Ferreira SH. Peripheral analgesic action of clonidine: mediation by release of endogenous enkephalin-like substances. Eur J Pharmacol. 1988;146(2–3):223–228. doi:10.1016/0014-2999(88)90296-8
17. Fares KM, Mohamed SAE, Abd El-Rahman AM, Mohamed AA, Amin AT. Efficacy and safety of intraperitoneal dexmedetomidine with bupivacaine in laparoscopic colorectal cancer surgery, a randomized trial. Pain Med. 2015;16(6):1186–1194. doi:10.1111/pme.12687
18. Namrata DHSPDNSDBS. Comparison of intraperitoneal instillation of bupivacaine and bupivacaine with dexmedetomidine for postoperative analgesia after laparoscopic surgery. Int J Inn Res Med Sci. 2016;01(07):259–265.
19. Rokhgireh S, Mehdizadehkashi A, Vahdat M, et al. The impact of intraperitoneal dexmedetomidine with bupivacaine on patients’ postoperative pain in endometriosis laparoscopic surgery; a randomized, clinical trial. Shiraz E Med J. 2019;20(7):0–5. doi:10.5812/semj.85296
20. Reza E, Bhuiyan K, Emon RI, et al. Efficacy of intra-peritoneal tramadol instillation for postoperative pain management after laparoscopic cholecystectomy. Mymensingh Med J. 2020;29(2):303–310.
21. Jamal A, Usmani H, Khan MM, Rizvi AA, Siddiqi MMH, Aslam M. Intraperitoneal pre-insufflation of 0.125% bupivaciane with tramadol for postoperative pain relief following laparoscopic cholecystectomy. J Anaesthesiol Clin Pharmacol. 2016;32(2):257–260. doi:10.4103/0970-9185.173402
22. SalwaMS H, El Hefnawy E, Askar W, Suliman Lucy AM. Intraperitoneal instillation of lornoxicam–levobupivacaine versus tramadol–levobupivacaine in patients undergoing laparoscopic cholecystectomy under general anesthesia. Res Opin Anaesth Intensive Care. 2019;6(2):228. doi:10.4103/roaic.roaic_12_19
23. Deshmukh P, Takalkar S, Chaudhari A, Chakole V. A prospective comparative study to assess-post operative analgesic effect of intraperitoneal instillation of bupivacaine with dexmedetomidine to bupivacaine with tramadol in patients undergoing laparoscopic cholecystectomy. Indian J Forensic Med Toxicol. 2020;14(4):6546–6551.
24. Mukkavilli Lakshmi Narasimham BDR. Comparison of intraperitoneal bupivacaine alone or with dexmedetomidine or tramadol for post-operative analgesia. J Clin Anaesth. 2017;4(1):143–146.
25. Schulz KF, Altman DG, Moher D; CONSORT Group. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. PLoS Med. 2010;7(3):e1000251. doi:10.1371/journal.pmed.1000251
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

