Back to Journals » Therapeutics and Clinical Risk Management » Volume 19
Comparative Study About Different Doses of Remimazolam in Short Laparoscopic Surgery: A Randomized Controlled Double-Blind Trial
Authors Luo L, Jiang J, Zhang M, Guo Z, Zhang X, Wang F, Yang F
Received 30 June 2023
Accepted for publication 3 October 2023
Published 20 October 2023 Volume 2023:19 Pages 829—837
DOI https://doi.org/10.2147/TCRM.S428278
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Deyun Wang
Li Luo,1 Jiduan Jiang,2 Min Zhang,1 Zhiqiang Guo,1 Xianzheng Zhang,1 Fenglin Wang,1 Fan Yang1
1Department of Anesthesiology, Suining Central Hospital, Suining City, Sichuan Province, People’s Republic of China; 2Department of Anesthesiology, Suining First People’s Hospital, Suining City, Sichuan Province, People’s Republic of China
Correspondence: Fan Yang, Department of Anesthesiology, Suining Central Hospital, Suining City, Sichuan Province, 629000, People’s Republic of China, Email [email protected]
Objective: To study the efficacy and safety of different doses of remimazolam used for induction and maintenance in short laparoscopic surgery.
Methods: A randomized controlled trial was conducted between May 2021 and May 2022 on patients underwent laparoscopic surgery for 30 minutes to an hour. Based on the drug used and the infusion rate, included patients were allocated into the Low-group of remimazolam (using a constant infusion rate of 6.0 mg/kg/h for induction and the rate of 1 mg/kg/h for maintenance), the Median-group (9.0 mg/kg/h for induction, 2 mg/kg/h for maintenance), the High-group (12.0 mg/kg/h for induction, 3.0 mg/kg/h for maintenance), and the Propofol group. The postoperative extubation time was used as the primary outcome.
Results: A total of 192 patients were included in the study, with 47, 48, 48, and 49 patients in the Low-, Median-, High-, and Propofol group, respectively. There was a significant difference in postoperative extubation time, with the High-group having the highest duration of 15.21± 2.34 minutes compared to the Median-group (13.17± 1.71 minutes, p< 0.001), Low- group (12.72± 1.31 minutes, p< 0.001), and the Propofol group (12.24± 1.23 minutes, p< 0.001). No significant difference was found between the Low-group and the Propofol group, while the Median-group still showed higher postoperative extubation time compared to the Propofol group (p=0.008).
Conclusion: Compared to propofol, total intravenous induction and maintenance with high and median dosages of remimazolam may prolong postoperative extubation time. Remimazolam can be safely used for induction and maintenance at various doses while not increasing the likelihood of adverse events.
Keywords: remimazolam, propofol, general anesthesia, extubation time, laparoscopic surgery
Introduction
Remimazolam, a new ultrashort benzodiazepine, acts through gamma-aminobutyric acid-a (GABA-A) receptors at the amygdala and reticulum activating system binding sites.1 By altering the conformation of chloride channels, it inhibits the action of these channels in the central nervous system and causes hyperpolarization.2 Midazolam, a traditional benzodiazepine used for sedation and anticonvulsants since 1982, has some drawbacks that limit its use for the maintenance of general anesthesia, including drug accumulation and prolonged sedation.3 Remimazolam, on the other hand, is a midazolam derivative with an ester moiety added and two forms - besylate and tosylate.4 Non-specific tissue esterases metabolize it, with its main metabolite CNS7054 possessing reduced binding capacity with the GABA-A receptor.4 Reports indicate that remimazolam has the advantages of rapid onset of action, short recovery time, and stable hemodynamics.4 Furthermore, flumazenil can quickly and specifically reverse its sedative effects, making it increasingly used for clinical anesthesia.5
Remimazolam was first approved for procedural sedation during gastrointestinal endoscopy.4 It was only recently approved in November 2021 for inducing and maintaining general anesthesia in China. Despite the package insert allowing for a 3-fold difference between the maximum and minimum dose of remimazolam for induction and maintenance doses, few studies have been conducted to compare the efficacy of different doses of remimazolam used for induction and maintenance of general anesthesia. To address this gap, this study applied different doses of remimazolam for short laparoscopic surgery and compared it with Propofol, focusing on the efficacy and safety of the different doses of remimazolam for induction and maintenance of general anesthesia, particularly in terms of anesthesia recovery and incidences of adverse event.
Methods and Materials
Patients, Grouping, and Blinding
The study recruited patients who underwent short laparoscopic surgery between May 2021 and May 2022 at Suining Central Hospital as participants. Inclusion criteria were as follows: aged between 18 and 60 years old, American Society of Anesthesiologists (ASA) grade I–II, operation time of 30 minutes to 1 hour, voluntary participation with informed consent signed by the patients and their families. Exclusion criteria included emergency surgeries, body mass index (BMI) > 30, significant blood volume loss or shock, use of other anesthesia methods, transplantation of heart, liver or kidney, severe liver dysfunction, anemia or thrombocytopenia, severe heart disease or infectious heart disease, uncontrolled hypertension or diabetes, potential difficult airway, history of drug abuse or alcoholism, mental system diseases, and allergy to benzodiazepines. Patients were randomly assigned to remimazolam Low-, Median-, and High- groups, as well as the Propofol group, using the digital random table method. Personnel responsible for patient recruitment, follow-up, and data analysis were not informed of the drugs administered. Independent personnel organized different doses of remimazolam and managed patients during the recovery period. The researchers responsible for intraoperative anesthesia management did not participate in other research sessions.
This trial was approved by the Ethics Committee of Suining Central Hospital on September 2, 2020 (LLSNCH20200035) and registered in the Chinese Clinical Trial Registration Center (ChiCTR2000038094, 2020/09/10). This study was conducted in accordance with the principles of the Declaration of Helsinki, and all patients participating in this study provided written informed consent.
Anesthesia Protocol
To calculate the induction and maintenance doses, the patient’s height and weight were obtained. On the day of the operation, standard monitoring was carried out as per ASA recommendations, with the depth of sedation and anesthesia monitored using the bispectral index (BIS) monitor from Aspect Medical Systems, US. Total intravenous induction was carried out in a sequential order of remimazolam (Jiangsu Hengrui Pharmaceutical Co., Ltd., China) or propofol (Sichuan Guorui Pharmaceutical Co., Ltd., China), sufentanil (0.5 ug/kg, Yichang Renfu Pharmaceutical Co., Ltd., China), and cisatracurium (0.15 mg/kg, Shanghai Pharmaceutical Dongying Pharmaceutical Co., Ltd., China), which was followed by endotracheal intubation. The time from the beginning of intravenous induction to the disappearance of eyelash reflex was recorded as the time of loss of consciousness (LoC). An infusion system (B. Braun, Germany) was used for target-controlled infusion. Remimazolam was administered to the Low group with a constant pump rate of 6.0 mg/kg/h and then changed to 1 mg/kg/h for maintenance until the end of the operation, while the Median- and High-groups had induction rates of 9.0 mg/kg/h and 12.0 mg/kg/h respectively, and maintenance rates of 2 mg/kg/h and 3.0 mg/kg/h respectively. The Propofol group received an induction dose of 2.0 mg/kg and a maintenance rate of 6.0 mg/kg/h. During the operation, total intravenous anesthesia was maintained with remifentanil added at a rate of 8–10 ug/kg/h (Yichang Renfu Pharmaceutical Co., Ltd., China). Intraoperative hypotension was treated with norepinephrine to maintain the mean arterial pressure at or above 65mmHg, and to ensure that the systolic blood pressure did not fluctuate more than 20% of the baseline value. Accordingly, the atropine was taken to prevent bradycardia. Core temperature was monitored and maintained at 36.3–36.8°C.
Additionally, a quality of recovery −40 questionnaire (QoR-40)6 was finished face-to-face as a baseline value (QoR-40baseline) 1 day before to the operation. The questionnaire was completed under the guidance of a researcher who had received training on the QoR-40 questionnaire survey.
Anesthesia Recovery Protocol and Follow-Up
The patients were transferred from the operation room to the Post-Anesthesia Care Unit (PACU). The Anesthesiologists in the PACU monitored the awakening of the patients using the Richmond agitation-sedation scale (RASS).7 Eight minutes after entering the PACU, their name was called every 2 minutes, and the passive eye-opening time was recorded. Once consciousness was regained with a RASS score between −3 and 0 and a train-of-four rate (TOFR) greater than 90%, the tracheal tube was removed and the extubation time was noted. After extubation, administer 4-5 L/min medium-flow mask oxygen therapy to the patient and continuously monitor the breathing and state of consciousness. If the RASS score of the patient remains at −3 or even drops to −4 within 5 minutes after extubation, 2mg Flumazenil (Jiangsu Nhua Pharmaceutical Co., Ltd., China) and 0.25 µg/kg nalmefene (Chengdu Tiantaishan Pharmaceutical Co., Ltd., China) were used for intervention. The assessment was repeated every 10 minutes after the intervention, and the same dose of flumazenil and nalmefene was repeated once if necessary. The inability to maintain pulse oxygen saturation (SpO2) levels above 90 after extubation with medium-flow mask oxygen therapy was classified as a post-extubation respiratory depression event. Similarly, a RASS score greater than +2 points was considered as emergence agitation, while a score of −4 or −5 points after 30 minutes in the PACU suggested delayed recovery. In addition, postoperative nausea and vomiting (PONV) were monitored, and tropisetron (5mg, Qilu Pharmaceutical Co., Ltd., China) was used to treat the condition. Once the Alderete score was ≥ 9, patients were transferred to the general ward, and the PACU stay duration was recorded. Following transfer, a nasal cannula was used to deliver continuous low-flow oxygen therapy and SpO2 levels were monitored continuously until 24 hours post-operation. Any SpO2 values below 90 during this period were considered a respiratory depression event. All patients received ultrasound-guided transversus abdominis plane block and intravenous parecoxib sodium (40 mg, Pharmacia & Upjohn Company LLC) as an analgesic in the PACU. Hydromorphone was used as a supplement if pain relief was found to be inadequate.
On the day following the surgery, the patients underwent follow-up, during which they completed the QoR-40 questionnaire (QoR-40postoperative). The incidence of respiratory depression and nausea and vomiting were carefully documented, and the modified Brice questionnaire8 was used to evaluate the occurrence of awareness during operation.
Outcomes
The primary outcome was the time to extubation after surgery. The secondary outcomes comprised various parameters such as: time of LoC, the time of PACU stay, passive eye-opening time, BIS values at different time points (T0: 5 minutes after induction, T1: at the beginning of the operation, T2: 30 minutes after the operation, T3: at the end of the operation, T4: 10 minutes after the operation), type of operation and operation time, volume of intraoperative infusion, dosage of remimazolam, propofol and remifentanil, usage rate of norepinephrine, flumazenil and nalmefene, and incidence of PONV. Besides, the study observed the impact of the sedative drug’s economic cost on the patients and assessed postoperative recovery quality using the QoR-40 questionnaire. The QoR-40 questionnaire included five dimensions of recovery, namely physical comfort (12 items), emotional state (9 items), physical independence (5 items), psychological support (7 items), and pain (7 items). Each item was rated on a five-point Likert scale - none of the time, some of the time, usually, most of the time, and all of the time. The total score obtained through QoR-40 assessment ranged from 40 (indicating poor quality of recovery) to 200 (indicating supreme quality of recovery).6 Besides, the study assessed the basic information of the patients, including gender, age, height, weight, and BMI.
Sample Size Calculation and Statistical Analysis
The PASS software (version 15.0) was used to calculate the sample size for multiple sample mean comparisons. In the preliminary trial, the average postoperative extubation time of each group was: 11.31±1.21 minutes (Low-group), 13.15±1.17 minutes (Median-group), 16.79±1.52 minutes (High-group), and 14.97±1.19 minutes (Propofol-group) respectively, with the lowest detectable difference of 1.82. Mean and standard deviation comparisons were performed using the Turkey method, with α=0.05 and β=0.2. The groups were designed to have a 1:1 ratio, and 42 participants in each group were required to achieve a power of 0.8. Considering a dropout rate of 20%, it was planned to recruit 50 patients to each group.
The statistical evaluation was executed utilizing SPSS software (Version 27.0, Chicago, Illinois, USA). Mean ± standard deviation (M±SD) was adopted to signify measurement data, followed by multi-sample mean-variance analysis. For Count data, n (%) was employed, along with either the chi-square test or Fisher’s exact test. The LSD method was used to performrepeated analysis of variance (ANOVA) measurements and multiple comparisons within and between groups. P-values less than 0.05 were deemed statistically significant.
Results
From May 2021 to May 2022, a total of 211 people met the initial inclusion and exclusion criteria and were divided into groups according to the digital random number method. Among them, 14 people were excluded because the operation lasted more than one hour, 3 people were excluded due to conversion to laparotomy, and 2 people were excluded because the operation time was less than half an hour. In the end, a total of 192 people were included in the study, with 47 people in the Low-group, 48 people in the Median-group, 48 people in the High-group, and 49 people in the Propofol group (Figure 1).
 |
Figure 1 The CONSORT Flow Diagram. |
Primary Outcome
The postoperative extubation time in the High-group was 15.21±2.34 minutes, which was significantly longer than the Median-group (13.17±1.71 minutes, p<0.001), the Low-group (12.72±1.31 minutes, p<0.001), and the Propofol group (12.24±1.23 minutes, p<0.001). The Low-group exhibited no significant difference in the postoperative extubation time compared to the Propofol group, whereas the Median-group still showed a higher postoperative extubation time when compared to the Propofol group, with a p-value of 0.008. (Table 1) The High-group had a range of 11–20 minutes of postoperative extubation time, while the Median-group had a range of 10–16 minutes, and the Low-group had a range of 10–15 minutes. Finally, the Propofol group exhibited a range of 10–16 minutes.
 |
Table 1 Results of Outcomes |
Secondary Outcomes
The duration of LoC decreased gradually with increasing doses of remimazolam, and there were statistically significant differences among the groups. The High-group had the shortest LoC time, which was 60.00±35.51 seconds, followed by the Median-group (82.08±33.28 seconds, p<0.001) and the Low-group (100.23±24.79 seconds, p<0.001). The Propofol group had the shortest LoC time of all, at 34.47±12.56 seconds (p<0.001), as per Table 1.
Patients in the Propofol group had a lower average actual body weight (66.96±10.87 kg) compared to the Median-group (72.46±11.70 kg, p=0.023) along with a lower BMI (23.01±2.87 vs 24.24±2.95 in Median-group, p=0.045 and 22.84±2.93 in High-group, p=0.023). The Propofol group also had a higher intraoperative norepinephrine usage rate and intraoperative hypotensive event rate (53.06% vs 30.61%) compared to the other three groups who received remimazolam during the operation (p<0.05). Furthermore, there were significant differences in the consumption of remimazolam and propofol as well as their corresponding costs among the four groups (p<0.001), as shown in Table 1. There was no statistically significant difference between other outcomes, p>0.05 (Table 1).
The average score of BIS in the Propofol group at T1 and T2 was 48.69±6.44 vs 49.65±6.20, respectively, which was significantly lower than those in the Low-group (56.32±8.28, p<0.001 vs 54.36±9.12, p=0.008), in the Median-group (57.50±8.85, p<0.001 vs 53.79±8.41, p=0.018), and in the High-group (56.06±9.10, p<0.001 vs 55.21±10.08, p=0.002). At T3, the BIS value of the Propofol group was 49.84±6.50, which was lower than that of the Median-group (54.21±9.34, p=0.008) and that of the High-group (53.23±8.06, p=0.04). Additionally, significant differences in the changes of BIS values within each group at each time point were present, p<0.05 (Figure 2).
Compared with the preoperative basic conditions, the total scores of the QoR-40 in the four groups were all statistically reduced after the operation within groups, p<0.05, but the differences were without statistical significance between groups. Correspondingly, the four sub-items of QoR-40 (Emotional status, Physical comfort, Psychological support, and Physical independence) also have statistical differences in the comparison of time before and after the operation, p<0.05, and similarly, there is no statistical difference between the four groups about these four sub-items. Regarding the Pain sub-item of QoR-40, no statistically significant differences were observed within or between the four groups, p>0.05 (Table 2).
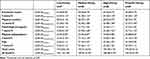 |
Table 2 Results of Preoperative and Postoperative Analysis of the Quality of Recovery-40 (QoR-40) Questionnaire |
Discussion
Remimazolam is an ultra-short-acting benzodiazepine, which can be rapidly metabolized to CNS7054 mainly by non-specific esterase [mainly carboxylesterase 1A (CES 1A)] in the human liver, with a half-life of about 6.8 minutes.9 Postoperative extubation time refers to the time after surgery that the patient is off the ventilator and the endotracheal tube is successfully extubated, which can reflect patient recovery and postoperative safety. Early identification of abnormalities during recovery can lead to further evaluation and treatment, benefiting high-risk patients.10 A shorter postoperative extubation time usually means a faster recovery for the patient and a lower risk of postoperative complications. It is widely used as an index to evaluate the quality and effect of surgery and to evaluate the effectiveness and safety of new anesthetic drugs and techniques.11 A standard post-awakening extubation strategy was used in this study, and we found a statistical difference in postoperative extubation time among the Low-group (using a constant infusion rate of 6.0 mg/kg/h for induction and 1 mg/kg/h for maintenance), the Median-group (9.0 mg/kg/h for induction, 2 mg/kg/h for maintenance), High-group (12.0 mg/kg/h for induction, 3.0 mg/kg/h for maintenance), and the Propofol group. The postoperative extubation time of the High-group (15.21±2.34 minutes) and the Median-group (13.17±1.71 minutes) was longer than that of the Low-group (12.72±1.31 minutes) and the Propofol group (12.24±1.23 minutes), which was similar to the median time of the extubation time [21 minutes, 95% confidence interval (CI) (15–28) minutes] reported previously.12 Although the statistical difference was achieved, the clinical value of the time difference remains to be explored. Similar to the average loss of consciousness (LoC) time reported in previous studies (81.7 seconds vs 97.2 seconds in two groups),13 there were also differences in the time of LoC after induction and the amount of remimazolam used among the three groups and the duration of LoC decreased gradually with increasing doses of remimazolam. The High-group had the shortest LoC time, which was 60.00±35.51 seconds, followed by the Median-group (82.08±33.28 seconds) and the Low-group (100.23±24.79 seconds). The Propofol group had the shortest LoC time of all, at 34.47±12.56 seconds. Additionally, the intraoperative norepinephrine usage and hypotension incidence rate were lower in the remimazolam group than in the Propofol group, indicating better hemodynamic stability. Nevertheless, the cost associated with the administration of remimazolam was greater compared to the Propofol group, and this cost increased notably as the dosage of remimazolam increased.
The possibility of resedation and secondary respiratory depression after using remimazolam is a major concern for clinicians, as they can adversely affect clinical quality and safety.9 Administration of high doses of remimazolam followed by antagonizing with flumazenil has resulted in reports of resedation with respiratory depression.14,15 However, in this study, the High-group, which administered the upper limit of the recommended dosage of remimazolam for anesthesia management, did not cause any more cases of postoperative respiratory depression, increased incidences of flumazenil or nalmefene use in the PACU, or re-sedation events, indicating that remimazolam may be safe for the respiratory tract. This may be due to its quick metabolism without accumulation and not affecting the level of respiratory muscle tension. Results may also be attributed to the emphasis on protecting patients’ body temperature during the operation.
Personalized sedative drug use is recommended in medical routine, and the titration method is commonly used.16 However, as a new drug for clinical use, this study did not adopt a sequential design17 or Dixon up-and-down methods17 to explore the dosage distribution of remimazolam. Instead, three dosage regimens were directly designed based on the recommended labeled induction and maintenance doses combined with standard intervention measures to reduce bias and confoundings. This methodology was based on existing reports of remimazolam’s safety and limited data on its clinical application.1 Since remimazolam is a new generation of benzodiazepines, delayed awakening or delirium during awakening in the recovery room should be considered.18 The incidence of emergence agitation did not differ significantly among the four groups and no delayed emergence occurred. This suggests that remimazolam’s application may reduce emergence agitation compared to midazolam, which needs further study. Future studies should focus on postoperative delirium in high-risk groups, such as elderly patients or patients who have been sedated with remimazolam for an extended period. The focus of this study was short laparoscopic surgery in ASA grade I–II patients; thus, extrapolation of the research findings may be limited.
According to the results of this study, the BIS value in the remimazolam group during the operation was higher in comparison to the Propofol group. However, there were no significant differences in the BIS value among the three different dosages of remimazolam administered. These findings indicate that using BIS value to accurately monitor the depth of anesthesia during maintenance with remimazolam may not be entirely reliable. This study’s conclusion is consistent with prior research13,17 and highlights the need for further calibration and exploration of the correlation between remimazolam and BIS values, and the underlying mechanisms.
The pilot experiment revealed that patients who received remimazolam for induction and maintenance were more fatigued after waking up in the PACU compared to those who received propofol. To evaluate the quality of recovery, the study employed the QoR-40 questionnaire. However, no discrepancies in the quality of recovery were found between the groups that received remimazolam and the group that received propofol. The limited sample size may have lowered the power of studying the QoR-40 questionnaire between groups. Additionally, the questionnaire was completed 1 day postoperatively instead of immediately postoperatively which may have contributed to the absence of differences between groups. Future studies should consider shortening the interval for the postoperative evaluation using the QoR-40 questionnaire.
This study has the following limitations. Firstly, the induction effect of remimazolam has not been compared with that of midazolam. Secondly, other possible adverse reactions caused by remimazolam were not given enough consideration, such as the deterioration of liver function and changes in the blood system. Lastly, the short follow-up period did not allow for the observation of potential long-term adverse events.
Conclusions
Compared to propofol, total intravenous induction and maintenance with high and median dosages of remimazolam prolonged postoperative extubation time. Remimazolam can be safely used for induction and maintenance at various doses while not increasing the likelihood of adverse events. But remimazolam has a relatively high cost of use when compared to propofol.
Institutional Review Board Statement
The study protocol has been reviewed and approved by the Ethics Committee of Suining Central Hospital [LLSNCH20200035, 2020/09/02] and conducted in compliance with the Declaration of Helsinki.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Informed Consent Statement
All patients provided informed consent for participation.
Funding
This study is funded by the Project of Sichuan International Medical Exchange & Promotion Association (No. L20200509024) and authors acknowledge the help from it.
Disclosure
The authors confirm that the PI for this paper is Fan Yang, who had direct clinical responsibility for patients. The authors declare no competing interests in this work.
References
1. Kim S-H, Fechner J. Remimazolam – current knowledge on a new intravenous benzodiazepine anesthetic agent. Korean J Anesthesiol. 2022;75(4):307–315. doi:10.4097/kja.22297
2. Sneyd JR, Rigby-Jones AE. Remimazolam for anaesthesia or sedation. Curr Opin Anaesthesiol. 2020;33(4):506–511. doi:10.1097/ACO.0000000000000877
3. Conway A, Rolley J, Sutherland JR. Midazolam for sedation before procedures. Cochrane Database Syst Rev. 2016;2016(5):CD009491. doi:10.1002/14651858.CD009491.pub2
4. Keam SJ. Remimazolam: first Approval. Drugs. 2020;80(6):625–633. doi:10.1007/s40265-020-01299-8
5. Kilpatrick GJ. Remimazolam: non-clinical and clinical profile of a new sedative/anesthetic agent. Front Pharmacol. 2021;12:690875. doi:10.3389/fphar.2021.690875
6. Lee WK, Kim MS, Kang SW, Kim S, Lee JR. Type of anaesthesia and patient quality of recovery: a randomized trial comparing propofol-remifentanil total i.v. anaesthesia with desflurane anaesthesia. Br J Anaesth. 2015;114(4):663–668. doi:10.1093/bja/aeu405
7. Sessler CN, Gosnell MS, Grap MJ, et al. The Richmond Agitation-Sedation Scale: validity and reliability in adult intensive care unit patients. Am J Respir Crit Care Med. 2002;166(10):1338–1344. doi:10.1164/rccm.2107138
8. Walker EMK, Bell M, Cook TM, et al. Patient reported outcome of adult perioperative anaesthesia in the United Kingdom: a cross-sectional observational study. Br J Anaesth. 2016;117(6):758–766. doi:10.1093/bja/aew381
9. Wang M, Zhao X, Yin P, Bao X, Tang H, Kang X. Profile of remimazolam in anesthesiology: a narrative review of clinical research progress. Drug Des Devel Ther. 2022;16:3431–3444. doi:10.2147/DDDT.S375957
10. Miao M, Xu Y, Sun M, Chang E, Cong X, Zhang J. BIS index monitoring and perioperative neurocognitive disorders in older adults: a systematic review and meta-analysis. Aging Clin Exp Res. 2020;32(12):2449–2458. doi:10.1007/s40520-019-01433-x
11. Grant MC, Isada T, Ruzankin P, et al. Results from an enhanced recovery program for cardiac surgery. J Thorac Cardiovasc Surg. 2020;159(4):1393–1402.e7. doi:10.1016/j.jtcvs.2019.05.035
12. Yang JJ, Lei L, Qiu D, et al. Effect of remimazolam on postoperative delirium in older adult patients undergoing orthopedic surgery: a prospective randomized controlled clinical trial. Drug Des Devel Ther. 2023;17:143–153. doi:10.2147/DDDT.S392569
13. Doi M, Hirata N, Suzuki T, Morisaki H, Morimatsu H, Sakamoto A. Safety and efficacy of remimazolam in induction and maintenance of general anesthesia in high-risk surgical patients (ASA Class III): results of a multicenter, randomized, double-blind, parallel-group comparative trial. J Anesth. 2020;34(4):491–501. doi:10.1007/s00540-020-02776-w
14. Masui K. Caution!! Reappearance of remimazolam effect after a flumazenil bolus: a larger bolus of flumazenil and a lower total remimazolam clearance are higher risks. J Anesth. 2023;37(1):1–5. doi:10.1007/s00540-022-03107-x
15. Yamamoto T, Kurabe M, Kamiya Y. A mechanism of re-sedation caused by remimazolam. J Anesth. 2021;35(3):467–468. doi:10.1007/s00540-021-02930-y
16. Conway A, Sutherland J. Depth of anaesthesia monitoring during procedural sedation and analgesia: a systematic review and meta-analysis. Int J Nurs Stud. 2016;63:201–212. doi:10.1016/j.ijnurstu.2016.05.004
17. Liu M, Sun Y, Zhou L, Feng K, Wang T, Feng X. The median effective dose and bispectral index of remimazolam tosilate for anesthesia induction in elderly patients: an up-and-down sequential allocation trial. Clin Interv Aging. 2022;17:837–843. doi:10.2147/CIA.S364222
18. Kassie GM, Nguyen TA, Kalisch Ellett LM, Pratt NL, Roughead EE. Preoperative medication use and postoperative delirium: a systematic review. BMC Geriatr. 2017;17(1):298. doi:10.1186/s12877-017-0695-x
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

