Back to Journals » Journal of Pain Research » Volume 12
Combined ultrasound-guided Pecs II block and general anesthesia are effective for reducing pain from modified radical mastectomy
Authors Senapathi TGA , Widnyana IMG, Aribawa IGNM , Jaya AAGPS , Junaedi IMD
Received 10 December 2018
Accepted for publication 27 February 2019
Published 26 April 2019 Volume 2019:12 Pages 1353—1358
DOI https://doi.org/10.2147/JPR.S197669
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Katherine Hanlon
Tjokorda Gde Agung Senapathi, I Made Gede Widnyana, I Gusti Ngurah Mahaalit Aribawa, A A Gde Putra Semara Jaya, I Made Darma Junaedi
Department of Anesthesiology and Intensive Care, Sanglah Hospital, Faculty of Medicine, Udayana University, Denpasar, Bali, Indonesia
Purpose: Combined regional and general anesthesia are often used for the management of breast cancer surgery. Thoracic spinal block, thoracic epidural block, thoracic paravertebral block, and multiple intercostal nerve blocks are the regional anesthesia techniques which have been used in breast surgery, but some anesthesiologists are not comfortable because of the complication and side effects. In 2012, Blanco et al introduced pectoralis nerve (Pecs) II block or modified Pecs block as a novel approach to breast surgery. This study aims to determine the effectiveness of combined ultrasound-guided Pecs II block and general anesthesia for reducing intra- and postoperative pain from modified radical mastectomy.
Patients and methods: Fifty patients undergoing modified radical mastectomy with general anesthesia were divided into two groups randomly (n=25), to either Pecs (P) group or control (C) group. Ultrasound-guided Pecs II block was done with 0.25% bupivacaine (P group) or 0.9% NaCl (C group). Patient-controlled analgesia was used to control postoperative pain. Intraoperative opioid consumption, postoperative visual analog scale (VAS) score, and postoperative opioid consumption were measured.
Results: Intraoperative opioid consumption was significantly lower in P group (P≤0.05). VAS score at 3, 6, 12, and 24 hrs postoperative were significantly lower in P group (P≤0.05). Twenty-four hours postoperative opioid consumption was significantly lower in P group (P≤0.05). There are no complications following Pecs block in both groups, including pneumothorax, vascular puncture, and hematoma.
Conclusion: Combined ultrasound-guided Pecs II block and general anesthesia are effective in reducing pain both intra- and postoperatively in patients undergoing modified radical mastectomy. Ultrasound-guided Pecs II block is a relatively safe peripheral nerve block.
Keywords: Pecs block, interfascial injection, regional anesthesia, ultrasound-guided, pain, modified radical mastectomy, breast surgery
Introduction
The effective acute postoperative pain management of breast surgery is necessary. Uncontrolled acute postoperative pain is one of the risk factors for chronic pain. Turan et al1 study reported that chronic pain was detected in 41.8% of the patients who had severe acute postoperative pain. Combined regional and general anesthesia are the common management for breast cancer surgery. Regional anesthesia provides anesthesia/analgesia during and after surgery. A regional technique continued into the postoperative period offers postoperative analgesia, attenuation of the surgical stress response, reduction in postoperative nausea and vomiting (PONV), and early mobilization. Thoracic spinal block (TSB), thoracic epidural block, thoracic paravertebral block (TPVB), and multiple intercostal nerve blocks are the regional anesthesia techniques which have been used in breast surgery. Those techniques have disadvantages including pneumothorax (1% TPVB, 2% intercostal), bleeding risk (especially epidural hematoma), dural puncture, and hypotension.2,3 In 2011, Blanco4 presented a novel interfascial plane block between the pectoralis major and minor muscles called Pecs block, which later became known as Pecs I block. In 2012, Blanco et al5 introduced Pecs II block or modified Pecs block as a novel approach to breast surgery. Pecs block are newer US-guided blocks with low risk of complication.6–8
Several randomized controlled trials (RCT) regarding Pecs II block have been done. The effectiveness of Pecs II block for breast surgery has been compared with TPVB by Wahba et al and Kulhari et al, and with TSB by ELdeen. Wahba et al9 and Kulhari et al10 concluded that Pecs II block reduces postoperative opioid consumption and provides better pain relief compared with the TPVB. ELdeen11 concluded that Pecs II block and TSB provide effective intraoperative anesthesia and postoperative pain relief, but the Pecs II block is simpler and safer. Other RCTs, ie, Bashandy et al12, El-Sheikh et al13, and Kim et al14, compared the effectiveness of combined Pecs II block and general anesthesia versus general anesthesia alone for breast surgery. Those studies concluded that Pecs block reduced pain intensity and opioid requirements when combined with general anesthesia for breast surgery. However, those studies were not double-blind and placebo-controlled.
This double-blind RCT tried to determine the effectiveness of combined Pecs II block and general anesthesia for reducing intra- and postoperative pain from modified radical mastectomy.
Patients and methods
Patients
This is an experimental study with a double-blind, randomized, placebo-controlled trial design. This study involved 50 patients with physical status American Society of Anesthesiologist (ASA) I-II, aged 16–65 years old, undergoing unilateral modified radical mastectomy with general anesthesia in the central operating theater at Sanglah Hospital (Joint Commission International – Accredited) from May through July 2018. The patient was not admitted to the study if any the following criteria were present: patient refusal, physical status ASA III or more, contraindications using local anesthetics, local infection at the site of injection, and a history of chronic analgesic use.
Subjects were randomly divided into two groups, to either Pecs (P) group or control (C) group using permuted block randomization by a research assistant with no clinical involvement in the study. The drugs were prepared by independent pharmacist and placed into envelopes according to the allocation orders. Both drugs cannot be distinguished because they contain the same colored liquid and the same volume. The detailed information was concealed in an envelope and revealed to the researchers after the study was over. The subject will be dropped out when such condition occurs: surgical duration >6 hrs, local anesthetic systemic toxicity, and discharge against medical advice before 24 hrs postoperatively. There was no loss of subject in this study.
Procedures
In the preparation room of central operating theater, intravenous (IV) access was obtained, crystalloid solutions and midazolam 0.03 mg/kg were administered intravenously. In the operating room, standard ASA monitors were placed and general anesthesia was done using IV propofol 2–2.5 mg/kg and fentanyl 2 mcg/kg as induction agents. Tracheal intubation facilitated by 0.5 mg/kg IV atracurium. General anesthesia was maintained with sevoflurane and 60% oxygen mixed with compressed air. The concentration of sevoflurane was adjusted to maintain a bispectral index between 40 and 60. Intravenous fentanyl 1 mcg/kg was administered if variations in systolic blood pressure and heart rate of ≥20% basal values.
Following induction of general anesthesia, ultrasound-guided Pecs II block was performed under complete aseptic technique using high frequency (15–6 MHz) linear array probe of SonoSite M-Turbo® ultrasound (US) system (FUJIFILM SonoSite, Bothell, WA, USA) by regional anesthesiologist staff who was blinded to the randomized intervention. The technique used was in accordance with the description by Blanco and Barrington.15 Patient in the supine position, with the arm abducted 90 degrees. The probe was placed below the clavicle, locates the coracoid process on US in the paramedian sagittal plane. The transducer was rotated slightly to allow an in-plane needle trajectory from the proximal and medial side toward the lateral side. A first injection was made between the pectoral major and minor muscles. The transducer was then moved laterally, and a second injection was made between the pectoralis minor and serratus anterior muscles.15 The block was performed by using a 22-gauge, 100 mm needle Stimuplex® Ultra (B. Braun Medical Inc., Pennsylvania, USA). Either 0.25% bupivacaine (P group) or 0.9% NaCl (C group) was administered, with volume 10 mL for the first injection and 20 mL for the second injection.
Postoperatively, patients received IV PCA morphine and IV bolus of ketorolac 30 mg every 8 hrs as analgesia. The CADD-Legacy® PCA Pump (Smiths Medical International Ltd, Kent, UK) was loaded with 1 mg/mL of morphine and set to administer an on-demand dose of 1 mL, 6 mins lockout interval, a maximum dose of 3 mg per hour, and no continuous infusion. Intraoperative opioid consumption, postoperative VAS score, and postoperative opioid consumption were measured.
Statistical analyses
All statistical analyses were performed using IBM SPSS for Windows (IBM Corporation, Armonk, NY, USA) software version 20. Numerical variable expressed as mean±SD or median (IQR). Categorical variable expressed as frequency (%). Test of normality using Shapiro–Wilk test and homogeneity test using Levene’s test. Compare mean test using independent-sample t-test if data distribution were normal or using nonparametric test Mann–Whitney U if not distributed normally. Chi-square test was used for a categorical variable. The level of significance α 0.05.
The required sample size was calculated using compare two means formula. Taking the intraoperative fentanyl consumption with a standard deviation of 37.3 mcg from previous study,12 for clinically important difference of 25 mcg, at a significance level (α) 5%, power (1-β) 90%, and a drop-out rate of 10%, then 50 patients (25 patients per group) should be sufficient.
Ethics statement
Ethical clearance of this study has been approved by the Research Ethics Committee of Faculty of Medicine Udayana University and Sanglah Hospital and in accordance with the Declaration of Helsinki. Prior to participation, all involved subjects and subject’s parents or legal guardians (for participants under the age of 18 years) gave written informed consent and were fully informed of the procedures in the studies.
Results
There were no significant differences (P>0.05) in both groups in terms of age, body mass index, ASA physical status, and duration of surgery (Table 1). The mean of age (years) in P group was 47.7±7.4 and 45.9±11.4 in C group. The median duration of surgery was 110 (18) mins in P group and 100 (23) mins in C group.
 | Table 1 Subject characteristics |
As given in Table 2, the intraoperative opioid consumption (fentanyl) was significantly different (P≤0.05). Patients in C group need more intraoperative fentanyl than patients in P group (median of 250 (75) mcg and 125 (25) mcg, respectively), with P-value <0.001.
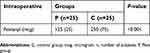 | Table 2 Comparison of intraoperative opioid consumption |
Postoperative VAS scores were significantly different at all times of evaluation (P≤0.05). As shown in Table 3 and Figure 1, postoperative VAS scores were higher in C group than P group at 3, 6, 12, and 24 hrs after surgery. The peak of the mean of postoperative pain score was at 3 hrs in C group and at 12 hrs in P group, 2.8±0.6 cm and 1.5±0.5 cm, respectively. The VAS scores in C group were high at 3 and 6 hrs (mean of 2.8±0.6 cm and 2.7±0.7 cm, respectively), then decreased at 12 and 24 hrs after surgery (mean of 1.9±0.7 cm and 1.9±0.6 cm, respectively). The VAS scores in P group were low at 3 hrs (mean of 0.7±0.6 cm), then elevated at 6 hrs (mean of 1.0±0.6 cm), and reached a peak at 12 hrs after surgery (mean of 1.5±0.5 cm).
 | Table 3 Comparison of postoperative pain score |
 | Figure 1 Visual analog scale scores (VAS) during the first 24 hrs after surgery. |
Opioid (morphine) consumption after surgery was significantly lower (P≤0.05) in P group than C group (Table 4 and Figure 2). At 24 hrs after surgery, the median of morphine consumption in P group was 3 (2) mg and 11 (4) mg in C group. No complications associated with the PECS II block such as hematoma, pneumothorax, and artery puncture were reported.
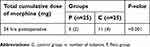 | Table 4 Comparison of postoperative opioid consumption |
 | Figure 2 Total morphine requirements 24 hrs after surgery. |
Discussion
Breast cancer is the most frequent cancer and causes the highest number of cancer-related deaths among women globally. In 2018, WHO estimates that 6,27,000 women died from breast cancer, that is approximately 15% of all cancer-related deaths among women.16 The modified radical mastectomy is one of the surgical options for breast cancer, which involves removal of the breast and axillary lymph nodes.17
Since introduced in 2012 by Blanco et al, Pecs II block gets attention as a new US-guided regional anesthesia for breast surgery. Several RCT9–14,18 and retrospective19,20 studies have been published in regard to the effectiveness of Pecs II block. This double-blind and placebo-controlled study shows that opioid requirements intra- and postoperative, and postoperative VAS score were significantly lower in Pecs group than in control (placebo) group. These findings are in accordance with the previous studies.
Pecs II block is applied in the pectoral and axillary regions to anesthetizes the whole breast and axilla. Pecs II block or modified Pecs block involves two injections. The first injection is accomplished by an injection of local anesthetic in the fascial plane between the pectoralis major and minor muscles. This injection is intended to anesthetize the medial (C8, T1) and lateral (C5–C7) pectoral nerves, which innervate the pectoralis muscles. The second injection is lateral to the first injection point in the plane between the pectoralis minor and serratus anterior muscles. This second injection is intended to anesthetize the lateral cutaneous branches of upper intercostal nerves (T2–T6), which will produce the dermatomal anesthesia to the chest wall (pectoral and axillary regions) and the long thoracic nerve (C5–C7), which innervate the serratus anterior muscle. The upper intercostal nerves are ventral rami of thoracic nerves. The intercostal nerves have lateral and anterior cutaneous branches. Each lateral cutaneous branch divides into anterior and posterior terminal branches, except the second intercostal nerve, which is called the intercostobrachial nerve. The anterior terminal branches run forward to the side and the forepart of the chest, supplying the skin and the breast. The posterior terminal branches run backward and supply the skin over the scapula and latissimus dorsi muscle. The intercostobrachial nerve innervates the axilla and medial side of the arm.3,5,14,15,21
In Pecs II block, the local anesthetics cannot reach the anterior cutaneous branches of the intercostal nerves by piercing the external and internal intercostal muscles.5,14,22 Additional block is advised for surgical with an incision in the parasternal area. Blanco et al5 advised to infiltrate between pectoralis major muscle and serratus anterior muscle, but on the medial side, close to the nipple. Ueshima and Kitamura22 advised using transverse thoracic muscle plane block, which infiltrate the plane between the transverse thoracic muscle and the internal intercostal muscle between the third and fourth ribs connecting at the sternum.
Postoperative VAS scores were significantly lower in Pecs group than control group at all times of evaluation (3, 6, 12, and 24 hrs after surgery). The VAS scores in control group were high at 3 and 6 hrs after surgery (mean of 2.8±0.6 cm and 2.7±0.7 cm, respectively). In this group, patients did not receive analgesia from the regional technique. In Pecs group, the VAS scores low at 3 hrs (mean of 0.7±0.6 cm), then elevated at 6 hrs (mean of 1.0±0.6 cm), and reached peak at 12 hrs after surgery (mean of 1.5±0.5 cm). The patients in this group received analgesia from Pecs II block. The analgesia of Pecs block lasts for approximately 8 hrs.5 A regional technique continued into the postoperative period offers postoperative analgesia, attenuation of the surgical stress response, reduction in PONV, and early mobilization.2
Postoperatively, patients received multimodal analgesia using IV PCA morphine and IV bolus of ketorolac 30 mg every 8 hrs. The underlying principle of multimodal analgesia is that the different modes of action of morphine and the non-opioid drug allow optimum analgesia to be maintained with a lower dose of morphine and consequently a lower incidence of morphine-related adverse effects.23 In this study, the median of 24 hrs postoperative morphine consumption was 3 (2) mg in Pecs group and 11 (4) mg in control group.
Conclusion
Combined ultrasound-guided Pecs II block and general anesthesia are effective in reducing pain both intra- and postoperatively in patients undergoing modified radical mastectomy. Ultrasound-guided Pecs II block is a relatively safe peripheral nerve block.
Acknowledgment
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Turan M, Karaman Y, Karaman S, Uyar M, Gonullu M. Postoperative chronic pain after breast surgery with or without cancer: follow up 6 months. Eur J Anaesthesiol. 2014;31:216. doi:10.1097/00003643-201406001-00619
2. Westbrook AJ, Buggy DJ. Anaesthesia for breast surgery. Br J Anaesth. 2003;8(5):151–154.
3. Gonzales J. PECS versus PVBS for perioperative analgesic management in breast surgery. ASRA News. 2016;16(3):41–44.
4. Blanco R. The‘pecs block’: a novel technique for providing analgesia after breast surgery. Anaesthesia. 2011;66(9):847–848. doi:10.1111/j.1365-2044.2011.06838.x
5. Blanco R, Fajardo M, Maldonado TP. Ultrasound description of Pecs II (modified Pecs I): a novel approach to breast surgery. Rev Esp Anestesiol Reanim. 2012;59(9):470–475. doi:10.1016/j.redar.2012.07.003
6. Ueshima H, Otake H. Ultrasound-guided pectoral nerves (PECS) block: complications observed in 498 consecutive cases. J Clin Anesth. 2017;42:46. doi:10.1016/j.jclinane.2017.08.006
7. Versyck B, Houwe P, Geffen GJ, Velde M, Slappendel R. A qualitative systematic review of the pectoral nerves block type I and II. Acta Anaesthesiol Belg. 2017;68(2):49–62.
8. Nair AS, Sahoo RK, Ganapathy M, Mudunuri R. Ultrasound guided blocks for surgeries/procedures involving chest wall (Pecs 1,2 and serratus plane block). Anaesth Crit Care Pain Med. 2015;19(3):348–351.
9. Wahba SS, Kamal SM. Thoracic paravertebral block versus pectoral nerve block for analgesia after breast surgery. Egypt J Anaesth. 2014;30(2):129–135. doi:10.1016/j.egja.2013.10.006
10. Kulhari S, Bharti N, Bala I, Arora S, Singh G. Efficacy of pectoral nerve block versus thoracic paravertebral block for postoperative analgesia after radical mastectomy: a randomized controlled trial. Br J Anaesth. 2016;117(3):382–386. doi:10.1093/bja/aew223
11. ELdeen HM. Ultrasound guided pectoral nerve blockade versus thoracic spinal blockade for conservative breast surgery in cancer breast: a randomized controlled trial. Egypt J Anaesth. 2016;32(1):29–35. doi:10.1016/j.egja.2015.08.005
12. Bashandy GM, Abbas DN. Pectoral nerves I and II blocks in multimodal analgesia for breast cancer surgery: a randomized clinical trial. Reg Anesth Pain Med. 2015;40(1):68–74. doi:10.1097/AAP.0000000000000163
13. El-Sheikh SM, Fouad A, Bashandy GN, Al-Azzb MA, Gamal RM. The role of modified PECs block in control of perioperative pain in breast surgeries. Med J Cairo Univ. 2017;85(3):961–966.
14. Kim D, Kim S, Kim CS, et al. Efficacy of pectoral nerve block type II for breast-conserving surgery and sentinel lymph node biopsy: a prospective randomized controlled study. Pain Res Manag. 2018;2018:1–8.
15. Blanco R, Barrington MJ. Pectoralis and serratus plane blocks. In: Hadzic A, editor. Hadzic’s Textbook of Regional Anesthesia and Acute Pain Management.
16.
17. Chassin JL. Operative Strategy in General Surgery. New York: Springer; 1984.
18. Kumar S, Goel D, Sharma SK, et al. A randomised controlled study of the post-operative analgesic efficacy of ultrasound-guided pectoral nerve block in the first 24 h after modified radical mastectomy. Indian J Anaesth. 2018;62(6):436–442.
19. Morioka H, Kamiya Y, Yoshida T, Baba H. Pectoral nerve block combined with general anesthesia for breast cancer surgery: a retrospective comparison. JA Clin Rep. 2015;1. doi:10.1186/s40981-015-0018-1
20. Yuki I, Ueshima H, Otake H, Kitamura A. PECS block provides effective postoperative pain management for breast cancer surgery—a retrospective study. Int J Clin Med. 2017;8(3):198–203. doi:10.4236/ijcm.2017.83019
21. Collin T, Cox J. Chest wall and breast. In: Standring S, editor. Gray’s Anatomy – The Anatomical Basis of Clinical Practice.
22. Ueshima H, Kitamura A. Blocking of multiple anterior branches of intercostal nerves (Th2-6) using a transversus thoracic muscle plane block. Reg Anesth Pain Med. 2015;40(4):388. doi:10.1097/AAP.0000000000000245
23. Maund E, McDaid C, Rice S, Wright K, Jenkins B, Woolacott N. Paracetamol and selective and non-selective non-steroidal anti-inflammatory drugs for the reduction in morphine-related side-effects after major surgery: a systematic review. Br J Anaesth. 2011;106(3):292–297. doi:10.1093/bja/aeq406
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
