Back to Journals » Clinical Ophthalmology » Volume 11
Combined resection–recession versus combined recession–retroequatorial myopexy of medial rectus muscles for treatment of near-distance disparity Esotropia
Authors Ghali MA
Received 13 March 2017
Accepted for publication 20 April 2017
Published 6 June 2017 Volume 2017:11 Pages 1065—1068
DOI https://doi.org/10.2147/OPTH.S136879
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Manar A Ghali
Ophthalmology Department, Faculty of Medicine, Zagazig University, Zagazig, Egypt
Purpose: To compare and evaluate the efficacy of two different surgical techniques for the treatment of near-distance disparity esotropia; combined resection–recession and recession–retroequatorial myopexy of medial rectus muscles.
Patients and methods: This prospective study included 28 patients diagnosed with convergence excess esotropia who had worn their full cycloplegic refraction and/or bifocal glasses for at least 6 months and still had near-distance disparity esotropia. The patients were divided into 2 groups; Group I underwent combined bimedial rectus muscles resection 2.5 mm from the insertion end with recession based on near-angle esotropia according to current surgical tables with 1 mm add of recession for each muscle, while Group II underwent bimedial recession based on far angle combined with retroequatorial myopexy at 13–14 mm from insertion. A satisfactory result was defined as orthophoria or esotropia <10 prism diopters (∆) at near and distance with reduction of the near-distance disparity to <10 ∆. The patients were followed up for at least 2 years for stability of correction and late onset consecutive exotropia.
Results: In Group I, all the patients had satisfactory alignments at near and far with residual near–far disparity ≤10 ∆, no cases of overcorrection at far was reported; while in Group II, all cases had orthophoria at far, but 4 cases (28.6%) showed near–far disparity >10 ∆.
Conclusion: The technique of combined resection–recession is safe, easy and more effective in the treatment of near-distance disparity esotropia regardless of the level of accommodative convergence/accommodation ratio, with stability of results though longer follow-up period is still needed.
Keywords: near-distance disparity, esotropia, Ac/A ratio, retroequatorial myopexy, slanted recession
Introduction
Convergence excess esotropia is defined as esotropia that is greater for near fixation than for distance. This was first described by Donders.1 Much confusion has been generated by its definition through the years.2 An acceptable definition of convergence excess esotropia would be a convergent squint, which is >8 prism diopter (PD) and is greater for near fixation than distance fixation after full hypermetropic correction.3
Excessive convergence in response to an accommodative demand may be the cause; and this group of patients’ accommodative convergence/accommodation (AC/A) ratio will be high. However, some patients with normal, and even low, AC/A ratio may have this type of esotropia.4
Controversy in the management of convergence excess esotropia has developed through the years; bifocals have been used to control it since the nineteenth century.5 The surgical management of near-distance disparity esotropia represents a challenging problem. Augmented medial rectus recession,6 medial rectus recession combined with retroequatorial myopexy7 and slanted rectus recession8 were modalities for surgical treatment.9
Akar et al proved that medial rectus Y-split recession is also an effective modality in the treatment of partially accommodative esotropia with convergence excess.10
Many studies advocated the technique of bilateral combined resection and recession of medial rectus muscle for the treatment of convergence excess esotropia; this procedure depends on extirpating proprioceptive impulse at the myotendineous junction.11–13
Palisade endings, which are found in myotendineous junction of medial rectus muscle is supposed to be the source of afferent feedback to the central nervous system. Therefore, their removal would, in theory, decrease centrally driven accommodative effort.14
This study aims to compare the efficacy of combined resection–recession technique and combined recession retroequatorial myopexy in the treatment of near-distance disparity esotropia.
Patients and methods
Twenty-eight patients were enrolled in this prospective study during the period January 2013 to April 2015. The study was approved by the Institutional Review Board of faculty of medicine, Zagazig University, Zagazig, Egypt. The guardians of all patients enrolled in this study signed a written consent prior to the beginning of the study.
All the patients recruited in this study were esotropic with convergence excess and had worn spectacles incorporating full cycloplegic refraction for at least 6 months. All of them had near esotropia that was greater than distance esotropia by 15 Δ or more. Patients who had satisfactory alignment but needed bifocal add for near alignment and achieved binocular vision at near were excluded. Also, patients with previous squint surgery, amblyopia at the time of surgery, oblique muscle dysfunction or neurologic problems were excluded from this study. Patients with different levels of AC/A ratio (high >5 Δ/D), (normal 2–5 Δ/D) or (low <2 Δ/D) were included.
AC/A ratio was measured for all patients by gradient method, which is the difference between angle with and without +3 lenses divided by +3 while wearing full cycloplegic refraction.
Refraction measurements were performed with cyclopentolate 1% instilled 30–40 minutes before retinoscopy and verified by autorefractometer.
The patients were randomly divided into two groups; Group I (14 patients) underwent resection 2.5 mm from the insertion end of the medial rectus muscle combined with recession according to near angle and addition of 1 mm recession for each medial rectus to compensate for effect of resection. Group II (14 patients) underwent bimedial rectus muscle recession according to distance angle combined with retroequatorial myopexy 13–14 mm from the medial rectus muscle insertion.
A satisfactory result was defined as orthophoria or esotropia of <10 Δ at near and distance fixation, with reduction of the near-distance disparity to <10 Δ.
The patients were followed up 1 week postoperatively and then at 1, 3, 6, 12, 18 and 24 months for stability of correction and incidence of consecutive exotropia. The final results were based on deviation measured at the last follow-up examination.
The collected data were coded and analyzed using SPSS, the level of significance was P<0.05, the power of study 80%–95% CI. Mean, median, standard deviation, and range for quantitative data summarization, Student’s t-test, and Mann–Whitney U-test for their analysis. For qualitative data summarization; number, percentage and Chi-square test were done.
Results
In Group I (14 patients; 8 girls and 6 boys) age (6.36±1.75) ranged from 3.5–9 years, with 7 patients with high AC/A ratio (50%), 6 patients with normal AC/A ratio (43%) and 1 patient with low AC/A ratio (7%). Preoperative near-distance disparity (22.21±6.03) ranged from 15 Δ–27 Δ. The preoperative angle at far was (8.43±7.03) and at near (30±6.79). As regards the refractive error; 8 (57%) patients were bilateral hypermetropic (2D–6.5D) and 6 patients (43%) were bilateral emmetropes with no myopic patients.
While in Group II (14 patients; 7 girls and 7 boys) age (6.43±2.09) ranged from 3.5–10 years, with 6 (43%) patients with high AC/A ratio, 7 (50%) patients with normal AC/A ratio and 1 (7%) patient with low AC/A ratio with preoperative near for disparity (20±3.86) ranging from 15 Δ to 26 Δ. The preoperative angle at far was 11.07±8.00 and at near was 31.07±7.12. Among Group II, 7 (50%) patients were bilateral hypermetropic, with error ranging from 1.5 to 5.5 D; 6 (43%) patients were bilateral emmetropic; and 1 patient (7%) was bilateral myopic with refractive error of −2D. Table 1 represents preoperative data of both groups.
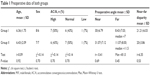  | Table 1 Preoperative data of both groups |
No significant statistical difference was found between both groups according to preoperative data.
At last visit postoperatively, the postoperative angle at far in Group I was 0±0 and at near was 3.57±2.85, with reduction of near-distance disparity to 3.57±2.85. However, in Group II, the postoperative angle at far was 0±0 and at near was 9.21±5.75, with reduction of near-distance disparity to 9.21±5.75. Table 2 presents the comparison between both groups according to postoperative results.
  | Table 2 Comparison between both groups according to postoperative angle at near and far, near–far disparity and success rate |
In Group I, all cases showed satisfactory results (100%) with orthophoria or esotropia of 10Δ at near and far with reduction of the near-distance disparity to 10Δ with no cases of latent exotropia. Also, there was result stability throughout the follow-up period.
While in Group II, 4 cases showed under-correction and near angle of deviation >10 Δ, and near–far disparity >10 Δ with satisfactory results of only 71.4%.
Discussion
Different surgical techniques have been described to reduce the near-distance disparity, including standard approach,15 augmented recession,6 slanted medial rectus recession,16 posterior fixation sutures, medial rectus pulley posterior fixation17 and marginal myotomy.18 Some authors worked on far angle of deviation, while some worked on mean angle of near and far deviations.19 Yet, others worked on the near angle of deviation but their results showed high incidence of distance exophoria.20
High AC/A ratio was reported as the cause of near-distance disparity, though this type of esotropia was found in patients with normal and even low AC/A ratio. In this study, 46.4% had high AC/A ratio, 46.4% had normal ratio and 7.2% had low ratio. These ratios were comparable with previous study of Vivian et al.3
In this study, Group II underwent recession according to far angle of deviation. Our results showed no incidence of exotropia at far but the success rate was 71.4%, with 4 cases with near-distance disparity >10 PD, which agreed with previous studies9 and was less than other studies7 in which success rate was 88%. This difference may be attributed to the very short follow-up period of the other study (3 months only) compared with our 2-year follow-up period.
The 4 cases of undercorrection in Group II were treated with bifocal glasses and 3 patients achieved binocular vision at near while the fourth case underwent 1 lateral rectus resection.
Combined resection–recession technique was first described by Bock et al11 who recommended large resections and small recessions. Thacker et al recommended that recession amount would be more than the resection amount.12 While in Ramasamy et al’s study, the amount of recession was double that of resection.13
In Group I, we did resection of 2.5 mm in all cases with recession according to near angle based on current surgical tables with 1 mm excess of recession in each muscle, we reported 100% success rate with decrease in near–far disparity from 21.21±6.03 to 3.75±2.85; there were no cases of distance exotropia throughout the follow-up period. Our results showed stability of success, though longer follow-up period still needed as consecutive exotropia could sometimes take 10 years to develop.
We believe that resection–recession technique is safe and easy with the advantage of stability of results in all patients of near–far disparity whatever their AC/A ratio. This study is limited by the number of subjects, the strict inclusion criteria, and the relatively short follow-up period. Also nearly all the patients had preoperative good alignment at distance with only 10 cases showing small distance angle ranging from 15–25 Δ. Future studies are recommended to avoid these limitations.
Conclusion
Combined resection–recession is an easy and safe technique that shows better results in the treatment of near–far disparity, though large sample size and longer follow-up periods are still needed.
Disclosure
The authors report no conflicts of interest in this work.
References
Donders FC. On The Abnormalities of Accommodation and Refraction of The Eye. London: The New Sydenham Society; 1864. | ||
Dbo TG. Convergence excess accommodative esotropia: a descriptive review of patients presenting over a period of 10 years. Br Orthopt J. 2011;8:23–28. | ||
Vivian AJ, Lyons CJ, Burka J. Controversy in the management of convergence excess esotropia. Br J Ophthalmol. 2002;86(8):923–929. | ||
Arnoldi KA. Convergence excess: characteristics and treatment. Am Orthop J. 1999;46:37–47. | ||
Javal E. Manuel ehorique et pratique du strabisme. [Manual of theoritical and practical strabismus]. Paris: Masson; 1896. French. | ||
Kushner BJ, Presian MW, Mortin GV. Treatment of partly accommodative esotropia with high accommodative convergence-accommodation ratio. Arch Ophthalmol. 1987;105(6):215–818. | ||
Stark N, Vanselow K, Stahl E, Zubcov AA. Fadenoperation mit beidseitiger Medialisrucklagerung. [Retroequatorial myopexy combined with bimedial recession for near-distance disparity esotropia]. Ophthalmologe. 1999;96(8):513–521. German. | ||
Bagarmlor H, Unlu C, Dag Y. Slanted medial rectus recession is effective in the treatment of convergence excess esotropia. J Pediatr Ophthalmol Strabismus. 2014;51(6):337–340. | ||
Khalifa YM. Augmented medial rectus recession, medial rectus recession plus faden and slanted medial rectus recession for convergence excess esotropia. Eur J Ophthalmol. 2011;21(2):119–124. | ||
Akar S, Gokyiqit B, Ayqit ED, Sabanci S, Demirok A. Is Y-split recession of the medial rectus muscle as effective as scleral retroequatorial myopexy of the medial rectus muscle for partially accommodative esotropia with convergence? A report of results in 61 cases. Binocul Vis Strabolog Q Simms Romano. 2013;28(3):167–175. | ||
Bock CJ Jr, Buckley EG, Freedman SF. Combined resection and recession of a single rectus muscle for the treatment of incomitant strabismus. J AAPOS. 1999;3(5):263–268. | ||
Thacker NM, Velez FG, Rosenbaum AL. Combined adjustable rectus muscle resection–recession for incomitant strabismus. J AAPOS. 2005;9(2):137–140. | ||
Ramasamy B, Rowe F, Whitfield K, Nayak H, Noonan CP. Bilateral combined resection and recession of the medial rectus muscle for convergence excess esotropia. J AAPOS. 2007;11(3):307–309. | ||
Lienbacher K, Mustari M, Ying HS, Buttner Ennerver JA, Horn AK. Do palisade endings in extraocular muscles arise from neurons in the motor nuclei? Invest Ophthalmol Vis Sci. 2011;52(5):2510–2519. | ||
Archer SM. The effect of medial versus lateral rectus muscle surgery on distance-near incomitance. J AAPOS. 2009;13(1):20–26. | ||
Nermet P, Stalovich C, Lowenstein A. A new operation; slanted (Reinsertion) medial rectus muscle recession surgery for convergence excess esotropia: results in 12 cases. Binocul Vis Strabismus Q. 1993;8:241–246. | ||
Mitchell L, Kowal L. Medial rectus muscle pulley posterior fixation sutures in accommodative and partially accommodative esotropia with convergence excess. J AAPOS. 2012;16(2):125–130. | ||
De Faber JT, Von Noorden GK. Medial rectus marginal myotomies for persistent esotropia. Am L Ophtalmol. 1991;112(6):702–705. | ||
Burke JP. Distance-near disparity esotropia: can we shrink the gap? Eye. 2015;29(2):206–213 | ||
Arnoldi KA, Tychsenl L. Surgery for esotropia with a high accommodative convergence/accommodation ratio: effects on accommodative vergence and binocularity. Ophthalmic Surg Lazers. 1996;27(5):342–348. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
