Back to Journals » OncoTargets and Therapy » Volume 11
Combination of carcinoembryonic antigen with the American Joint Committee on Cancer TNM staging system in rectal cancer: a real-world and large population-based study
Authors Liu Q, Lian P, Luo D , Cai S , Li Q, Li X
Received 17 April 2018
Accepted for publication 14 July 2018
Published 13 September 2018 Volume 2018:11 Pages 5827—5834
DOI https://doi.org/10.2147/OTT.S171433
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Leo Jen-Liang Su
Qi Liu,1,2,* Peng Lian,1,2,* Dakui Luo,1,2 Sanjun Cai,1,2 Qingguo Li,1,2 Xinxiang Li1,2
1Department of Colorectal Surgery, Fudan University Shanghai Cancer Center, Shanghai, China; 2Department of Oncology, Shanghai Medical College, Fudan University, Shanghai, China
*These authors contributed equally to this work
Aim: This study assessed the combination of carcinoembryonic antigen (CEA) with the American Joint Committee on Cancer (AJCC) TNM staging system, aiming to improve the AJCC TNM staging system, in terms of prognostic accuracy and clinical management of rectal cancer.
Methods: Eligible patients (N=22,132) were selected from the Surveillance, Epidemiology, and End Results database between January 1, 2004, and December 31, 2010. Patients with elevated CEA levels were designated as “C1 stage” and those with normal CEA amounts as “C0 stage”. The outcome of interest was cancer-specific survival (CSS). Cox proportional hazards regression analyses and Kaplan–Meier curves were used to identify independent prognostic factors and analyze the odds of CSS in patients with rectal cancer in different C and TNM stages, respectively.
Results: C1 stage was associated with a 61.0% risk increase in cancer-specific mortality (HR=1.610, 95% CI=1.219–1.705, P<0.001). In addition, C0-stage patients showed improved CSS compared with C1-stage counterparts. In addition, CSS was improved in stage IIB–C0 patients (HR=2.478, 95% CI=1.660–3.699) compared with stage IIIB–C1 patients (HR=2.431, 95% CI=2.021–2.924) or IIIA–C1 patients (HR=1.060, 95% CI=0.823–1.366, P=0.650) and stage IIC–C0 patients (HR=4.263, 95% CI=3.308–5.493) compared with stage IIIB–C1 or IIIA–C1 counterparts.
Conclusion: C stage is an independent prognostic factor of rectal cancer. The improved prognostic precision of the C–TNM staging system and, thus, more individualized risk-adaptive treatments support the incorporation of C stage into the AJCC TNM staging system in rectal cancer.
Keywords: C-stage, AJCC, rectal cancer, SEER
Introduction
Colorectal cancer is one of the most prevalent malignancies worldwide, and rectal cancer accounts for 40% of all colorectal cancers.1 The American Joint Committee on Cancer (AJCC) TNM staging system is the most commonly used algorithm in clinical practice. However, it is not perfect in the prognostic prediction and clinical management of rectal cancer.2
Carcinoembryonic antigen (CEA) is a protein that is normally produced during prenatal development. After birth, CEA blood levels are normally very low or undetectable. Meanwhile, elevated CEA levels are associated with many carcinomas and other health conditions. Colorectal cancer is a common cause of elevated CEA amounts, and CEA testing is recommended in assessing patients prior to surgery and for monitoring recurrence post surgery.3
In 2000, the Colorectal Working Group of AJCC recommended that TNM groups should be stratified based on the presence or absence of elevated serum levels of CEA (≥5 ng/mL) during preoperative clinical examination.2
We have focused on improving the AJCC TNM staging system and applied the previously proposed C stage in colon cancer to rectal cancer.4,5 Using the Surveillance, Epidemiology, and End Results (SEER) database, the current large population-based study was performed, aiming to assess the improvement of prognostic accuracy and clinical management of rectal cancer with the C–TNM staging system.
Patients and methods
Study design and data source
The National Cancer Institute’s SEER*Stat software, Version 8.3.5 (Surveillance Research Program, National Cancer Institute SEER*Stat software, www.seer.cancer.gov/seerstat) was used to select patients diagnosed with rectal cancer between January 1, 2004, and December 31, 2010, from the SEER-registered database, which is an authoritative source of information on cancer incidence and survival in the United States (Figure 1). The SEER database provides a comprehensive source of population-based information, including all newly diagnosed cancer cases in individuals residing in SEER-participating areas and covering ~28% of the US population.
  | Figure 1 Flow diagram of patient population selected from SEER database. |
As shown in Figure 1, among these patients with rectal cancer, individuals with known CEA test results, AJCC TNM stage, and positive histological confirmation were included in the current study. Patients with unknown race, unknown tumor size, or non-adenocarcinomatous histology and those not treated by surgery were excluded.
C–TNM stage
Considering the seventh edition of the AJCC, TNM stages were not assigned to patients diagnosed before 2010. We obtained the anatomic extent of the primary tumor using the code “CS extension” to determine the corresponding T stage in the seventh edition for each patient; based on the code “regional nodes positive (2004+),” the N stage in the seventh edition was derived; using the code “Derived AJCC M, sixth ed. (2004+)”, the M stage in the seventh edition was determined. Then, AJCC TNM stages (seventh edition) were manually assigned to each patient (I, IIA, IIB, IIC, IIIA, IIIB, IIIC, or IV). The CEA values of rectal cancer in the SEER database were recorded prior to treatment. Next, the patients with elevated CEA levels were designated as “C1 stage” and those with normal CEA as “C0 stage”. Finally, a modified AJCC TNM staging system (C–TNM stage) was assigned to each patient after the incorporation of C stage.
Statistical analyses
Several Cox proportional hazards models were built to identify independent prognostic factors. All hazard ratios were shown with 95% CIs. Variables that showed prognostic significance (log-rank test, P<0.20) in univariate analysis were entered in multivariate analysis using Cox proportional hazards models of the selected patients: tumor location, tumor grade, seventh AJCC TNM stage, tumor size, age at diagnosis, gender, and year of diagnosis. Kaplan–Meier survival curves were used to assess the prognostic values of different factors, with the log-rank test used to assess statistical significance. This study also designed a variable called N–C stage, combining N stage (N0, N1, N2a, and N2b stages) and C stage (C0 and C1, based on CEA levels), to compare the interaction between these two stages in patients with nonmetastatic rectal cancer.
Statistical analysis was performed with SPSS version 22 (IBM Corporation, Armonk, NY, USA), and two-sided P<0.05 was considered as statistically significant.
Ethics statement
The study was approved by the ethical committee and institutional review board of the Fudan University Shanghai Cancer Center. The data did not include that of human subjects or personal identifying information, and no informed consent was required for this study.
Results
C stage is a strong prognostic factor in the overall cohort
Median follow-up time for the overall cohort was 63 months. At the end of the follow-up period, 5,544 (25.0%) patients succumbed to rectal cancer. Multivariable analysis was performed to identify significant prognostic factors in the overall cohort. We found that C stage was independently associated with cancer-specific survival (CSS) in 22,132 patients with rectal cancer and caused a 61.0% increase in risk of cancer-specific mortality (HR=1.610, 95% CI=1.219–1.705, P<0.001; Table 1). In addition, other parameters were identified as prognostic factors, including tumor location, tumor grade, seventh AJCC TNM stage, tumor size, age at diagnosis, and gender. In addition, multivariable Cox analysis of all the nonmetastatic rectal cancer patients (n=19,338, 87.38% of the overall cohort) selected from the whole cohort demonstrated that C1 stage was associated with a 56.9% increase in risk of cancer-specific mortality in nonmetastatic rectal cancer, again confirming the prognostic value of C stage (HR=1.569, 95% CI=1.467–1.677, P<0.001; Table S1).
  | Table 1 Multivariable Cox regression analyses of all independent prognostic factors |
Prognostic value of C–TNM stage combining C and AJCC TNM stages
Multivariate Cox regression analysis was used to assess HRs for various AJCC TNM- and C–TNM stages. Five-year CSS rates were also assigned to various C–TNM and TNM stages. Overtly, all C0–TNM-stage patients showed higher 5-year CSS and lower HRs compared with the corresponding C1–TNM-stage patients (Table 2). In addition, HRs of stages IIA–C0 (HR=1.029, 95% CI=0.850–1.245, P=0.770) and IIIA–C0 (HR=1.060, 95% CI=0.823–1.366, P=0.650) were not significantly different from the HR of stages I–C1. Furthermore, the HRs of several stage C1–TNM patients even exceeded those of stage C0–TNM counterparts with higher conventional AJCC TNM stages. Cause-specific mortality increased in stage IIB–C1 patients (HR=2.478, 95% CI=1.660–3.699) compared with stage IIIB–C0 patients (HR=2.431, 95% CI=2.021–2.924) or IIIA–C0 patients, as well as in stage IIC–C1 patients (HR=4.263, 95% CI=3.308–5.493) compared with stage IIIB–C0 or IIIA–C0 patients. The abovementioned stage migration indicated that the C–TNM stages had a more accurate prognostic value compared with the TNM stage in rectal cancer.
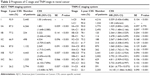  | Table 2 Prognosis of C stage and TNM stage in rectal cancer |
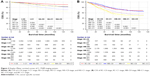
Kaplan–Meier survival curves for C–TNM stages were also used to analyze the prognostic value of C–TNM staging in the whole cohort (n=22,132; Figure 2A and B). The abovementioned phenomenon indicated that C0–TNM-stage patients showed improved CSS compared with the corresponding C1–TNM-stage patients, as illustrated in Kaplan–Meier curves.
Prognostic value of N stage combined with C stage
Multivariate Cox regression analysis was performed in patients with non-metastatic rectal cancer (stages I, II, and III) to assess HRs of various N stages (N0, N1, N2a, and N2b) before and after combination with C stage (N–C stage); 5-year CSS rates were also calculated for each stage (Table 3). The results showed that all C1-stage groups of each N stage showed higher HRs and decreased 5-year CSS compared with the corresponding C0-stage counterparts. Furthermore, all C1-stage groups of each N stage showed higher HRs and decreased 5-year CSS compared with the respective C0-stage counterparts of higher N stage. For example, stage N0–C1 (HR=1.841, 95% CI=1.681–2.017) showed higher cancer-specific mortality than stage N1a–C0 (HR=1.722, 95% CI=1.505–1.971). These findings indicated that C1-stage (elevated CEA) patients had similar prognosis to N1a-stage counterparts.
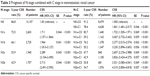  | Table 3 Prognosis of N stage combined with C stage in nonmetastatic rectal cancer |
Discussion
The current study assessed the prognosis of different AJCC TNM stages in rectal cancer after combination with C stage (C0 stage, normal CEA levels; C1 stage, elevated CEA levels). The target patients with available CEA information were identified from the large population-based SEER database. We demonstrated that C stage was an independent prognostic factor; further analysis revealed that C1 stage may be a stronger predictor of worse prognosis. Therefore, we proposed the incorporation of C stage into the AJCC TNM staging system in clinical practice for rectal cancer assessment.
Despite the wide application in clinical practice for rectal cancer assessment, the AJCC TNM staging system only considers the invasion extent of the primary tumor (T stage), lymph node status (N stage), and distant spread (M stage) without taking into account other factors that influence the prognosis of rectal cancer.6 The resulting stage is therefore not perfect in prognostic prediction, although several modifications in the past years have improved its predictive ability.
In 2000, the Colorectal Working Group of the AJCC proposed incorporating C stage as a means to further refine the TNM staging system.2 However, the lack of a uniform definition of elevated CEA level7 and other reasons hindered the incorporation of the latter parameter into the AJCC staging system until now. In an update in 2006, the ASCO expert panel concluded that data are insufficient to support the use of elevated preoperative serum CEA to determine whether to treat a patient by adjuvant therapy.8 However, based on growing evidence regarding the usefulness of CEA in further determining patients’ prognosis, we proposed that incorporation of C stage into the AJCC TNM staging system deserves further investigation.9
In the present large, representative, and population-based study, the AJCC TNM staging system was extended to include CEA test results. As shown earlier, all C1-stage patients had significantly increased mortality compared with C0-stage ones of the same TNM stage, with a 61.0% increase in HR of the whole cohort. The increased cancer-specific mortality of C1 stage was also validated in patients with nonmetastatic rectal cancer. Another finding of this study was that survival of several C0–TNM stages even exceeded C1–TNM stages with higher AJCC TNM stages. The increased cancer-specific mortality in stage IIB–C1 patients compared with stage IIIB–C0 or IIIA–C0 patients as well as in stage IIC–C1 patients compared with stage IIIB–C0 or IIIA–C0 patients indicated that CEA levels have an upstaging effect that may constitute an important complement for the AJCC TNM staging system, which could be of great clinical significance. In 2004, pooled analysis of five Phase III cooperative group trials showed local recurrence rates of 7% and 9% for the pT1-2N1 and pT3N0 groups, respectively.10 Meanwhile, increased CSS in stage IIIA–C0 patients compared with that in stage IIA–C1 counterparts also seems to explain the lack of clear rank in pT1-2N1 and pT3N0 rectal cancer cases in predicting outcomes using conventional TNM stages.
Although adjuvant chemotherapy is currently recommended by the National Comprehensive Cancer Network (NCCN) and the European Society for Medical Oncology (ESMO) in the postoperative management of stage II/III rectal cancer regardless of the fact that stage II has a significantly lower risk of recurrence, application of adjuvant chemotherapy remains controversial, and a large population-based study showed that adjuvant chemotherapy does not improve outcomes in randomly selected patients with stage II rectal cancer.11,12 Currently, it is widely accepted that patients with TNM stage II colon cancer showing any of the high-risk factors, including T4-stage, obstruction, perforation, poorly differentiated histology, <12 lymph nodes, presence of lymphovascular or perineural invasion, and positive margins, might be considered candidates for adjuvant chemotherapy.13–16 Yet, application of these high-risk features for adjuvant chemotherapy in stage II rectal cancer seems to be suboptimal.17 We suggested that C stage could play a role in selecting more appropriate patients with stage II rectal cancer who should receive adjuvant chemotherapy and highly disagree with the application of adjuvant chemotherapy in stage IIA–C0 rectal cancer.
This study showed that stage IIIA–C0 (T1–T2N1M0) had similar cancer-specific mortality with stage I (T1–T2N0M0) C1 and 5-year survival (89.5% vs 90.4%). Considering almost the same in the T stage (T1–T2), the C1 stage was once again shown to be non-inferior to the N1 stage for indicating poor prognosis. However, in clinical practice nowadays, stage IIIA patients are treated with adjuvant chemotherapy, while stage I cases are not.18,19 Therefore, this study took into account the possibility of undertreatment of TNM stage I rectal cancer cases and overtreatment of patients with TNM stage IIIA rectal cancer. Meanwhile, toxicity and adverse events caused by overtreatment in TNM stage IIIA rectal cancer should be considered. Fortunately, C stage could distinguish well between stages I–C0 and I–C1 in TNM stage I cases and between stages IIIA–C0 and IIIA–C1 in TNM stage IIIA cases, providing additional evidence to support C stage incorporation into the AJCC TNM staging system and suggesting less chemotherapy in stage IIIA–C0, which also deserves further investigation in prospective studies.
The improved prognosis of several node-positive stages (stages IIIA–C0, IIIA–C1, and IIIB–C0, respectively) compared with multiple node-negative stages (stages IIC–C0, IIB–C1, and IIC–C1, respectively) suggested that node status may not be precise enough in predicting the prognosis of patients with malignant rectal carcinoma. In addition, all C0-stage groups in each N stage showed higher HRs and decreased 5-year CSS rates compared with C0-stage counterparts in the higher N stage. Our findings suggested that C1-stage patients would have similar prognosis compared with N1a-stage counterparts, indicating that C1 stage might also be a powerful predictor of poor prognosis. Considering node-positive stages received adjuvant chemotherapy while node-negative stages not, we believe that C stage may have its role in the guidance of adjuvant chemotherapy in rectal cancer.
This study had several limitations. First, the C–TNM stage did not take into account other prognostic factors, including the DNA mismatch repair (MMR) status, chemotherapy, and radiotherapy, which could independently affect patient survival.18,20 Second, although C1 stage may be associated with poor survival, whether C1-stage rectal cancer would benefit from current conventional chemotherapy remains controversial and deserves further investigation. Next, though colorectal cancer is a common cause of elevated CEA levels, such elevation could also be caused by biliary obstruction, inflammatory digestive disorders, smoking, and so on.21 Finally, the abovementioned analyses were merely based on retrospective data. Therefore, future prospective clinical studies of C stage are required for a more sensitive risk-adaptive staging system.
Conclusion
This large population-based study demonstrated that C stage is an independent prognostic factor. We hold the belief that routine preoperative CEA testing should be conducted for all rectal cancer patients, with C stage included into the TNM staging system. However, further evaluation of C stage is required to identify optimal candidate patients who may benefit from adjuvant treatment.
Acknowledgments
We have great respect for the work that goes into compiling and maintaining the SEER Program tumor registries, including the interpretation and reporting of these data and so on. The National Natural Science Foundation of China (Grant Nos 81702353 and 81772599) supported this work.
Disclosure
The authors report no conflicts of interest in this work.
References
Siegel R, Desantis C, Jemal A, Statistics Ccancer. CA: a cancer journal for clinicians. 20142014;64(2):104–117. | ||
Compton C, Fenogliopreiser CM, Pettigrew N, et al. American Joint Committee on Cancer prognostic factors consensus conference: Colorectal working group [J]. Cancer. 1999;86(11):2436. | ||
Chen VW, Ruiz BA, Hsieh MC, Charlton ME, et al. Analysis of stage and clinical/prognostic factors for lung cancer from SEER registries: AJCC staging and collaborative stage data collection system. Cancer. 2014;120 Suppl 23(S23):3781–3792. | ||
Thirunavukarasu P, Talati C, Munjal S, Attwood K, Edge SB, Francescutti V, Carroll T. Effect of Incorporation of Pretreatment Serum Carcinoembryonic Antigen Levels Into AJCC Staging for Colon Cancer on 5-Year Survival. JAMA Surg. 2015;150(8):747. | ||
Thirunavukarasu P, Sukumar S, Sathaiah M, et al. C-stage in Colon Cancer: Implications of Carcinoembryonic Antigen Biomarker in Staging, Prognosis, and Management. JNCI: Journal of the National Cancer Institute. 2011;103(8):689–697. | ||
Yarbro JW, Page DL, Fielding LP, Partridge EE, Murphy GP. American Joint Committee on Cancer prognostic factors consensus conference. Cancer. 1999;86(11):2436–2446. | ||
Thirunavukarasu P, Sukumar S, Sathaiah M, et al. C-stage in colon cancer: implications of carcinoembryonic antigen biomarker in staging, prognosis, and management. J Natl Cancer Inst. 2011;103(8):689–697. | ||
Locker GY, Hamilton S, Harris J, et al. ASCO 2006 update of recommendations for the use of tumor markers in gastrointestinal cancer. J Clin Oncol. 2006;24(33):5313–5327. | ||
Tarantino I, Warschkow R, Schmied BM, et al. Predictive Value of CEA for Survival in Stage I Rectal Cancer: a Population-Based Propensity Score-Matched Analysis. J Gastrointest Surg. 2016;20(6):1213–1222. | ||
Gunderson LL, Sargent DJ, Tepper JE, et al. Impact of T and N stage and treatment on survival and relapse in adjuvant rectal cancer: a pooled analysis. J Clin Oncol. 2004;22(10):1785–1796. | ||
Loree JM, Kennecke HF, Renouf DJ, et al. Effect of Adjuvant Chemotherapy on Stage II Rectal Cancer Outcomes After Preoperative Short-Course Radiotherapy. Clin Colorectal Cancer. 2016;15(4):352–359. | ||
Schmoll HJ, van Cutsem E, Stein A, et al. ESMO Consensus Guidelines for management of patients with colon and rectal cancer. a personalized approach to clinical decision making. Ann Oncol. 2012;23(10):2479–2516. | ||
Casadaban L, Rauscher G, Aklilu M, Villenes D, Freels S, Maker AV. Adjuvant chemotherapy is associated with improved survival in patients with stage II colon cancer. Cancer. 2016;122(21):3277–3287. | ||
O’Connor ES, Greenblatt DY, Loconte NK, et al. Adjuvant chemotherapy for stage II colon cancer with poor prognostic features. J Clin Oncol. 2011;29(25):3381–3388. | ||
Quah HM, Chou JF, Gonen M, et al. Identification of patients with high-risk stage II colon cancer for adjuvant therapy. Dis Colon Rectum. 2008;51(5):503–507. | ||
Sargent DJ, Goldberg RM, Jacobson SD, et al. A pooled analysis of adjuvant chemotherapy for resected colon cancer in elderly patients. N Engl J Med. 2001;345(15):1091–1097. | ||
Swets M, Kuppen PJK, Blok EJ, Gelderblom H, van de Velde CJH, Nagtegaal ID. Are pathological high-risk features in locally advanced rectal cancer a useful selection tool for adjuvant chemotherapy? Eur J Cancer. 2018;89:1–8. | ||
Kim MB, Hong TS, Wo JY, Jy W. Treatment of Stage II–III Rectal Cancer Patients. Curr Oncol Rep. 2014;16(1):1–9. | ||
Veereman G, Vlayen J, Robays J, et al. Systematic review and meta-analysis of local resection or transanal endoscopic microsurgery versus radical resection in stage i rectal cancer: A real standard? Crit Rev Oncol Hematol. 2017;114:43–52. | ||
de Rosa N, Rodriguez-Bigas MA, Chang GJ, et al. DNA Mismatch Repair Deficiency in Rectal Cancer: Benchmarking Its Impact on Prognosis, Neoadjuvant Response Prediction, and Clinical Cancer Genetics. J Clin Oncol. 2016;34(25):3039–3046. | ||
Thomas P, Toth CA, Saini KS, et al. The structure, metabolism and function of the carcinoembryonic antigen gene family [J]. Biochimica et Biophysica Acta (BBA) – Reviews on Cancer. 1990;1032(2):177–189. |
Supplementary material
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.