Back to Journals » Journal of Pain Research » Volume 13
Cognitive Function During Opioid Tapering in Patients with Chronic Pain: A Prospective Cohort Study
Authors Laigaard J , Bache N, Stottmeier S, Mathiesen O, Estrup S
Received 22 July 2020
Accepted for publication 13 September 2020
Published 14 December 2020 Volume 2020:13 Pages 3385—3394
DOI https://doi.org/10.2147/JPR.S273025
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Michael A Ueberall
Jens Laigaard,1 Nina Bache,2 Stefan Stottmeier,3 Ole Mathiesen,1,4 Stine Estrup1
1Centre for Anaesthesiological Research, Department of Anesthesiology, Zealand University Hospital, Køge, Denmark; 2Multidisciplinary Pain Center, Department of Anesthesiology, Zealand University Hospital, Køge, Denmark; 3Multidisciplinary Pain Center, Department of Anesthesiology, Holbæk Hospital, Holbæk, Denmark; 4Department of Clinical Medicine, University of Copenhagen, Copenhagen, Denmark
Correspondence: Jens Laigaard
Department of Anaesthesiology, Zealand University Hospital, Lykkebækvej 1, Køge 4600, Denmark
Tel +45 4261 7377
Email [email protected]
Purpose: Evidence for efficacy and safety lacks for long-term opioid therapy in patients with chronic non-cancer pain and adverse effects, including affection of cognitive function and quality of life, is of concern. We aimed to investigate cognitive function and health-related quality of life in patients with chronic non-cancer pain during opioid reduction.
Patients and Methods: At two multidisciplinary pain centers, all patients with planned opioid reduction were screened for eligibility. Cognitive function was assessed using the Repeatable Battery for the Assessment of Neuropsychological Status (RBANS) and Trail Making Test A and B. Health-related quality of life was assessed using Short Form-36 (SF36) and Hospital Anxiety and Depression Scale (HADS).
Results: We included 51 participants and 40 participants attended follow-up of median 254 (IQR 106– 357) days. Baseline RBANS score was 82 (IQR 65– 93) with reference population norm value of 100 (SD± 15). Daily opioid consumption was reduced from median 80 (IQR 45– 161) oral morphine milligram equivalents to 19 (IQR 0– 60) mg. RBANS score estimate increased by 6.2 (95% CI 3.1– 9.3, p=0.0004) points after tapering. No differences were observed for Trail Making Test times, HADS or SF36 scores.
Conclusion: Generally, cognitive function showed minor improvement after opioid tapering with stationary health-related quality of life, depression and anxiety scores. The clinical significance is unclear, as no minimal clinically important difference in RBANS score is available.
Keywords: chronic non-cancer pain, chronic non-malignant pain, multidisciplinary pain center, memory, cognitive dysfunction, cognitive impairment
Introduction
Four to 12% of patients with chronic non-cancer pain (CNCP) conditions receive long-term treatment with opioids (>6 months), resulting in an overall prevalence of long-term opioid therapy of 1–4% in western adult populations.1–5 A recent meta-analysis of randomized controlled trials (RCTs) on opioids for patients with CNCP suggested that small benefits in pain, physical functioning and sleep quality can be achieved with short to intermediate term opioid therapy.6 Similar positive effects of long-term opioid therapy have not been demonstrated. Opioids were associated with more adverse events and their efficacy seemed to decrease over time.6 The evidence favoring long-term opioid therapy for CNCP patients is limited, considering that the longest follow-up time among most RCTs is less than six months.1,6,7
Moreover, several observational studies have linked long-term opioid use among patients with CNCP with worse outcomes, including decreased functional capacity, quality of life, and increased risk of overdose and death.7–9 These observations could be the related to the well-known adverse effects from opioid therapy, which include constipation, tolerance and physical dependence,6,10 and the lesser known adverse effects of dysfunction in immunologic and hormonal systems, altered sleep patterns and opioid-induced hyperalgesia.11–13 Also, interaction with other drugs are likely, including the frequent co-prescription with benzodiazepines.14
Consequently, tapering of opioids has been encouraged in recent guidelines, including the American Centers for Disease Control and the Canadian National Pain Centre.1,15
Studies on cognitive function during opioid therapy have presented conflicting results, with some suggesting improved cognitive function,16–18 some worsened function,19–23 and some suggesting no impact.24–29 A recent review found only significantly reduced attention among opioid users compared to non-users, but most included studies were cross-sectional and used different neuropsychological tests, thus limiting proper data synthesis into meta-analyses.23 Methodological flaws in previous, mostly observational studies, have hindered differentiation of cognitive dysfunction caused by the chronic pain condition and possible cognitive effects of long-term opioid therapy.30 The majority of published studies have examined the cognitive function during opioid dose escalation,16–18,24–26 though the current trend is towards tapering off opioids.1,15
Though desirable, RCTs on opioid tapering are difficult to conduct due to the highly individual treatment of CNCP patients and previous trials have had significant attrition rates.24,25,31 Therefore, well-designed longitudinal studies are warranted. We aimed to monitor cognitive function in patients with CNCP during opioid reduction at a multidisciplinary pain center.
Patients and Methods
We conducted a prospective cohort study with measurements of the patients’ cognitive function during opioid reduction at the multidisciplinary pain center at either Zealand University Hospital Køge or Holbæk Hospital, the Zealand Region, Denmark.
We reported in coherence with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guideline32 and registered the study on clinicaltrials.gov (NCT03036917). The study was conducted in accordance with the Declaration of Helsinki with ethical approval granted by the Biomedical Research Ethics Committee of Region Zealand (SJ-578) and data registration approved by the Danish Data Protection Agency. All patients gave informed, written and verbal consent prior to any collection of data. All individual, deidentified data are available along with the protocol by contact to the corresponding author.
Inclusion and Exclusion Criteria
From January 2018, all adult (>18 years) patients with planned opioid reduction treated at the multidisciplinary pain center at Zealand University Hospital, Køge, and from July 2018 at Holbæk Hospital, Holbæk, were screened for eligibility. Patients not able to speak and understand Danish and patients not able to provide informed consent were excluded.
Study Design
At referral to the multidisciplinary pain center, patients were asked to participate in the study as soon as possible, to achieve baseline data in a stable non-tapering phase. Patients admitted to the multidisciplinary pain centers are treated by a combination of medical doctors, nurses, psychologists, social workers and physiotherapists, which permits a range of individualized therapeutic options for each patient. As the pain centers treat the most challenging patients, various treatment modalities are used, which we neither monitored nor interfered with. The cognitive tests and questionnaires were administered at inclusion; at 50% reduction of daily opioid consumption, if achieved; and when the patient along with the multidisciplinary team decided that no further reductions were feasible.
Outcomes
Participants’ cognitive function were evaluated using the Repeatable Battery for the Assessment of Neuropsychological Status (RBANS)33 and the Trail-Making Test (TMT) A and B.34
RBANS is designed to assess and characterize cognitive function over time. The RBANS is designed to cover a broad range of difficulties as to avoid excessive flooring-effect. On five domains, scores ranging from 40 to 160 are found using age-specific tables, with a Scandinavian population cohort scoring a mean of 100 (standard deviation (SD)±15). The five domains are immediate memory, visuospatial function, language, attention and delayed memory. The RBANS tool has two editions of the test to increase repeatability. Attempts have been made to establish a minimal clinically important difference using an anchor-based approach, but with no solid results.35 Therefore, we chose not to use a specific cut-off value for clinical relevance.
The TMT is a simple connect-the-dots task in which the performance is measured by completion time.34 In the first part, TMT A, the subject sequentially connects the numbers 1–25, thereby testing motor speed. In the second part, TMT B, the subject alternates between numbers and letters (1, A, 2, B, etc.), testing both motor speed and executive functions, such as mental flexibility, something not assessed with RBANS.
We monitored anxiety and depression symptoms using the Hospital Anxiety and Depression Scale (HADS). The questionnaire consists of 14 questions and yields a total score and a separate score for anxiety and depression, respectively. It has been constructed for use in hospitalized patients but is widely used and exhibits good validity and specificity using a cut-off limit of ≥8 for both depression and anxiety, with higher score indicating worse symptoms.36
Lastly, patient-reported health-related quality of life was evaluated using the 36-Item Short Form Survey (SF36).37 Answers are transformed into a 0–100 scale, with lower scores indicating more impaired health-related quality of life. The SF36 covers both physical and mental health, with eight distinct subsections. Average scores from a Norwegian General population study were around 75–85 for the subsections and 50 for the physical and mental health summary.38
The collected time spent administering RBANS, TMT, HADS and SF36 was approximately 40–60 minutes depending on the subject. The primary outcome was the difference in RBANS overall score. Secondary outcomes were differences in the five RBANS domains, TMT, HADS and SF36 scores.
Data Collection
Data regarding opioid treatment, use of other medications, marital, educational and occupational status were reported by the patient. Opioid doses were converted to oral morphine milligram equivalents (OMEs) using CDCs 2017 conversion table.39 The type of pain was registered using electronic patient files. One of two authors (JL or SE) tested the subjects using RBANS and TMTs. The participants completed the questionnaires independently. The visits took place either at the pain center or at the patient’s home.
Statistics
No sample size analysis was performed due to the hypothesis-generating nature of the study and lack of comparable studies in this field. Thus, we planned a convenience sample of 50 participants.
Data were analyzed using the statistical software SAS 9.4. Data are presented as mean (±SD), median (interquartile range (IQR)) or absolute numbers (n (%)) as appropriate. Differences between baseline data of all participants versus both participants who did and participants who did not complete the study were examined using either unpaired t-test (age), two-samples Wilcoxon test (length of opioid use) or chi-square or Fisher’s exact test (count data). Repeated outcome measures (RBANS, TMT A and B, HADS, SF36) were analyzed using linear mixed-effects models with random effects on patient level and presented as maximum likelihood estimates (95% confidence intervals (CI)). This analysis and data presentation were planned as our data were repeated measures with limited sample size and because we anticipated a high attrition rate. We selected a level of statistical significance of 0.05.
Missing data were not imputed. From clinical experience, we knew that some patients would be lost to follow-up or end their treatment with a reduction in daily opioid use of less than 50%. These were statistically managed as having ended their tapering of opioids.
Results
Participants
Between January 2018 and May 2019, 60 patients were screened for participation. Of these, 51 patients were included and 40 completed the study. Twenty-one participants never reduced their opioid consumption by 50%, very quickly reduced their opioid consumption to the final dosage or for other reasons did not attend the halfway visit. The final dataset was collected in February 2020. The participants’ flow in the study is shown in Figure 1.
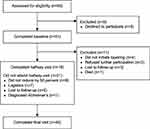 |
Figure 1 Diagram of participant flow. |
Of the 51 participants, 34 (67%) were women, the mean age was 56 (SD±13) years and 11 (22%) were employed, including five (10%) in government-funded part-time jobs (Table 1). The most frequent single pain diagnoses were lumbar back pain with radiculopathy (16 (31%)), polyarthritis (10 (20%)), and persistent pain after either lower extremity surgery (4 (8%)) or abdominal surgery (3 (6%)), though many participants had multiple pain diagnoses. Median length of opioid use was 10 (IQR 6–15) years and median opioid dose was 80 (IQR 45–161) OMEs at inclusion.39 The most commonly prescribed opioids were prolonged-release oxycodone (18 (35%)), prolonged-release morphine (11 (22%)), methadone (10 (20%)) and tramadol (6 (12%)).
 |
Table 1 Participant Demographics |
Outcomes
The halfway and final visit took place after a median of 101 and 254 days, respectively (Table 2). The median opioid dose was reduced from 80 (IQR 45–161, n=51) OMEs to 48 (IQR 30–90, n=19) OMEs at the halfway visit and 19 (IQR 0–60, n=40) OMEs at the final visit (Table 2).
 |
Table 2 Cognitive Scores and Health-Related Quality of Life Measures at Baseline and at Follow-Up Visits |
Only estimates for baseline versus final visit differences are presented, as these are more clinically relevant and due to the low number of data points from the halfway visit. Linear mixed-effects models analysis showed that the RBANS overall scores improved from baseline to final visit by 6.2 (95% CI 3.1–9.3, p=0.0004) points (Table 3). RBANS overall scores were median 82 (IQR 65–93), 81 (IQR 72–90) and 83 (IQR 72–95) points at baseline, halfway and final visit, respectively (Table 2). Of the 40 participants who completed the study, 29 improved their RBANS overall score, nine worsened and two had the same RBANS overall score at the final visit (Figure 2).
 |
Table 3 Maximum Likelihood Estimates from Linear Mixed-Effects Models |
In the RBANS domains, the participants significantly improved in four of five cognitive domains (Tables 2 and 3). The largest increase was seen for immediate memory, from 80 (IQR 68–90) points at baseline to 83 (IQR 70–95) and 85 (IQR 77–99) points at the halfway and final visit, respectively. The estimate for baseline versus final visit was an 8.8 (95% CI 4.8–12.9, p=0.0002) points increase. Lesser improvements were seen in visuospatial function, attention and delayed memory. No change was observed in the language RBANS domain. The patients’ individual development from first to final visit in the different domains are depicted in Figure 2.
TMT A times were 30 (IQR 22–44), 32 (IQR 24–40) and 29 (IQR 22–36) seconds at baseline, halfway and final visit, respectively (Table 2). The TMT A estimate for baseline versus final visit was −1.8 (95% CI −5.2–1.7 s, p=0.55) seconds (Table 3). Likewise, TMT B times were 73 (IQR 57–95), 75 (IQR 60–98) and 61.5 (IQR 51–97) seconds at baseline, halfway and final visit, respectively (Table 2). The TMT B estimate for baseline versus final visit was −4.7 (−13.1–3.8, p=0.49) seconds (Table 3).
HADS depression scores were 6 (IQR 4–10) points at baseline, 7 (IQR 3–8) points at the halfway visit and 5 (IQR 3–8) points at the final visit (Table 2). The depression score estimate for baseline versus final visit was −1.0 (95% CI −2.0–0.1, p=0.18) points (Table 3). Similarly, HADS anxiety scores were 4 (IQR 2–7) points at baseline, 3 (IQR 1–4) points at the halfway visit and 3 (IQR 2–5) points at the final visit (Table 2). The anxiety score estimate for baseline versus final visit was −0.9 (95% CI −2.0–0.3, p=0.05) points (Table 3).
Both the physical health component of SF36 (Physical Component Score (PCS)) and the mental health component of SF36 (Mental Component Score (MCS)) remained unchanged during the three visits (Tables 2 and 3). Median PCS score was 28.4 (IQR 24.2–33.7) points at baseline, 25.6 (IQR 22.8–33.4) points at the halfway visit and 28.3 (IQR 24.6–35.1) points at final visit. The PCS score estimate for baseline versus final visit was 0.6 (95% CI −1.4–2.7, p=0.81) points (Table 3).
MCS score was 46.4 (IQR 38.8–55.3) points at baseline with slight fluctuations to 50.7 (IQR 42.9–52.7) points at the halfway visit and 49.5 (IQR 43.5–55.5) points at the final visit. The MCS score estimate for baseline versus final visit was 2.5 (95% CI −1.6–6.5, p=0.42) points (Table 3).
Similar to the PCS and MCS scores, in none of the eight subsections of SF36, including bodily pain, did the scores reach statistical significance, though numerical increases were observed (Tables 2 and 3).
Discussion
In this prospective study of cognitive function during opioid reduction in patients with CNCP, we found a minor improvement of estimates in overall cognitive function, with the largest improvement seen for immediate memory. Health-related quality of life, anxiety and depression scores remained stationary during the study.
Our patients were comparable to the population of patients with CNCP in Denmark in terms of age, sex and educational level.2 However, some selection in this patient group was made. First, participants were recruited at a multidisciplinary pain center, which only treats patients who cannot be managed in a primary care unit. Secondly, only patients who consumed opioids and in whom opioid reduction was deemed beneficial could be included. Thus, our participants had a long history with multiple analgesic treatments, including high-dose opioids, high prevalence of neuropathic pain and low rate of employment. This, along with our findings of low cognitive function, is consistent with previous studies of this patient group in Denmark19,31 and internationally.14,20,21
We found minor increases in cognitive function in patients with CNCP after opioid reduction, with largest increase in the immediate memory domain. To our knowledge, despite an increasing number of tapering protocols and trials aiming to reduce opioid use,40 no previous cohort study of cognitive function during opioid reduction has been published. An abstract from the 32nd Annual Scientific Meeting of the American Pain Society in 2013 presented data on cognitive function in 12 patients with chronic pain during opioid detoxification and found results similar to ours, with improvements in most cognitive skills three months after opioid cessation and no difference in pain intensity or anxiety levels.41 The patients in that study were weaned off opioids in only one week, which is a major difference from our study. Also, proper comparison with that study is hindered as the study has not been published.
To our knowledge, no minimal clinically important differences have been suggested for longitudinal RBANS data, though attempts have been made.35 Most likely the difference needed for an individual to sense improvement or decline in cognitive function differs depending on baseline score, cognitive domain investigated, time between tests and more participant-specific factors.35,42 Hence, we are not able to verify if the improvements seen in our participants are clinically meaningful. Moreover, chronic pain causes cognitive dysfunction independent of opioid use.43,44 Distinguishing between whether the observed improvements are a result of opioid tapering or merely from being treated at the Multidisciplinary Pain Center is difficult. However, a comprehensive review found no change or even lessened pain intensity after opioid tapering in patients with chronic non-cancer pain.45
In the current study, most SF36 scores, and particularly the physical components, were low at baseline compared to the general population.38 This has previously been shown in this patient group.46 We found no significant differences in patient-reported health-related quality of life, but small numerical improvements in PCS, MCS and all subsections. This is consistent with previous studies of opioid cessation in this patient group.40
Investigating outcomes shortly after changing the opioid dose in CNCP patients may be inappropriate, as a change in opioid consumption causes symptoms and morphological changes to the brain that may resolve over time.47 In the current study, the final assessment was arranged after the patient had finished tapering off. This provided an interval of three weeks minimum, often several months, between the last change of dose and the final assessment. This is a strength, but also a limitation as we do not know how long it takes for homeostasis to occur after discontinuation of opioid consumption, why a more distinct time interval could have strengthened our study design.
Other strengths of our study included uniform data collection, with all tests administered by two trained instructors and the majority by a single instructor. Practice effects are a common problem in research of cognitive function when a test is taken more than once. We chose to use RBANS, which is designed to be repeatable, with each patient tested using the two editions alternatingly. The Trail Making Tests too have been proven reliable when repeated with sufficient time intervals.48 Finally, including patients from two separate sites and our prospective design with repeated measures increased the external validity of our data.
We converted opioid doses to morphine equivalents, though different types of opioids may differ in cognitive effects, which is a limitation in our study. Also, selection bias is possible, as nine patients did not want to participate and not all participants were followed up. This selection is inherently non-random, but difficult to avoid due to our patients’ limited resources. We did not monitor the development of concurrent comorbidities such as diabetes. Finally, a larger sample size and testing at specific time points would have given more solid results.
Conclusion
In this prospective cohort study, we found a minor improvement in estimates of cognitive function during tapering of opioids among patients with chronic non-cancer pain treated at a multidisciplinary pain center. This improvement included the cognitive domains, immediate memory, visuospatial function, attention and delayed memory. No difference after opioid reduction was observed in language, motor speed or executive functions. We found no changes in neither physical nor mental self-reported health-related quality of life, including depression and anxiety scores. The clinical relevance of the observed improvements in RBANS scores is unclear, as no minimal clinically important difference is available. Additionally, this prospective cohort study was designed to be hypothesis-generating and the results should be considered along with other studies in this field.
Acknowledgment
Preliminary results were presented at the 2019 Scandinavian Society of Anaesthesiology and Intensive Care Medicine Congress in Copenhagen (ABSSUB-202).49
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
Funding: The project received a grant from Kong Christian den Tiendes Fond (URL: Kongehuset.dk/node/5556).
Disclosure
The authors report no conflicts of interest for this work.
References
1. Dowell D, Haegerich TM, Chou R. CDC Guideline for Prescribing Opioids for Chronic Pain—United States, 2016. JAMA. 2016;315(15):1624–1645. doi:10.1001/jama.2016.1464
2. Kurita GP, Sjogren P, Juel K, Hojsted J, Ekholm O. The burden of chronic pain: A cross-sectional survey focussing on diseases, immigration, and opioid use. Pain. 2012;153(12):2332–2338. doi:10.1016/j.pain.2012.07.023
3. Marschall U, L’Hoest H, Radbruch L, Häuser W. Long-term opioid therapy for chronic non-cancer pain in Germany. Eur J Pain. 2016;20(5):767–776. doi:10.1002/ejp.802
4. Boudreau D, Von Korff M, Rutter CM, et al. Trends in long-term opioid therapy for chronic non-cancer pain. Pharmacoepidemiol Drug Saf. 2009;18(12):1166–1175. doi:10.1002/pds.1833
5. Eriksen J, Jensen MK, Sjøgren P, Ekholm O, Rasmussen NK. Epidemiology of chronic non-malignant pain in Denmark. Pain. 2003;106(3):221–228. doi:10.1016/S0304-3959(03)00225-2
6. Busse JW, Wang L, Kamaleldin M, et al. Opioids for Chronic Noncancer Pain: A Systematic Review and Meta-analysis. J Am Med Assoc. 2018;320(23):2448–2460. doi:10.1001/jama.2018.18472
7. Chou R, Turner JA, Devine EB, et al. The effectiveness and risks of long-term opioid therapy for chronic pain: A systematic review for a national institutes of health pathways to prevention workshop. Ann Intern Med. 2015;162(4):276–286. doi:10.7326/M14-2559
8. Ekholm O, Kurita GP, Hjsted J, Juel K, Sjgren P. Chronic pain, opioid prescriptions, and mortality in Denmark: A population-based cohort study. Pain. 2014;155(12):2486–2490. doi:10.1016/j.pain.2014.07.006
9. Novick TK, Surapaneni A, Shin J-I, et al. Associations of opioid prescriptions with death and hospitalization across the spectrum of estimated gfr. Clin J Am Soc Nephrol. 2019;14(11):1581–1589. doi:10.2215/CJN.00440119
10. Els C, Jackson TD, Kunyk D, et al. Adverse events associated with medium- and long-term use of opioids for chronic non-cancer pain: an overview of Cochrane Reviews. Cochrane Database Syst Rev. 2017;10(CD012509):1–44. doi:10.1002/14651858.CD012509.pub2
11. Roeckel L-A, Le Coz G-M, Gavériaux-Ruff C, Simonin F. Opioid-induced hyperalgesia: cellular and molecular mechanisms. Neuroscience. 2016;338(27):160–182. doi:10.1016/j.neuroscience.2016.06.029
12. de Vries F, Bruin M, Lobatto DJ, et al. Opioids and their endocrine effects: A systematic review and meta-analysis. J Clin Endocrinol Metab. 2020;105(4):1–10. doi:10.1210/clinem/dgz022
13. Franchi S, Moschetti G, Amodeo G, Sacerdote P. Do All Opioid Drugs Share the Same Immunomodulatory Properties? A Review From Animal and Human Studies. Front Immunol. 2019;10(2914):1–11. doi:10.3389/fimmu.2019.02914
14. Campbell G, Nielsen S, Bruno R, et al. The Pain and Opioids in Treatment study: characteristics of a cohort using opioids to manage chronic non-cancer pain. Pain. 2015;156(2):231–242. doi:10.1097/01.j.pain.0000460303.63948.8e
15. Busse JW, Craigie S, Juurlink DN, et al. Guideline for opioid therapy and chronic noncancer pain. CMAJ. 2017;189(18):E659–E666. doi:10.1503/cmaj.170363
16. Jamison RN, Schein JR, Vallow S, Ascher S, Vorsanger GJ, Katz NP. Neuropsychological effects of long-term opioid use in chronic pain patients. J Pain Symptom Manage. 2003;26(4):913–921. doi:10.1016/S0885-3924(03)00310-5
17. Rowbotham MC, Twilling L, Davies PS, Reisner L, Taylor K, Mohr D. Oral opioid therapy for chronic peripheral and central neuropathic pain. N Engl J Med. 2003;348(13):1223–1232. doi:10.1056/NEJMoa021420
18. Tassain V, Attal N, Fletcher D, et al. Long term effects of oral sustained release morphine on neuropsychological performance in patients with chronic non-cancer pain. Pain. 2003;104(1–2):389–400. doi:10.1016/S0304-3959(03)00047-2
19. Diasso PDK, Sjøgren P, Højsted J, Nielsen SD, Main KM, Kurita GP. Patient reported outcomes and neuropsychological testing in patients with chronic non-cancer pain in long-term opioid therapy: A pilot study. Scand J Pain. 2019;19(3):533–543. doi:10.1515/sjpain-2019-0007
20. Richards GC, Lluka LJ, Smith MT, et al. Effects of long-term opioid analgesics on cognitive performance and plasma cytokine concentrations in patients with chronic low back pain: A cross-sectional pilot study. Pain Reports. 2018;3(4):e669. doi:10.1097/PR9.0000000000000669
21. Schiltenwolf M, Akbar M, Hug A, et al. Evidence of specific cognitive deficits in patients with chronic low back pain under long-term substitution treatment of opioids. Pain Physician. 2014;17(1):9–20. doi:10.1016/j.spinee.2011.08.290
22. Gaertner J, Radbruch L, Giesecke T, et al. Assessing cognition and psychomotor function under long-term treatment with controlled release oxycodone in non-cancer pain patients. Acta Anaesthesiol Scand. 2006;50(6):664–672. doi:10.1111/j.1399-6576.2006.01027.x
23. Allegri N, Mennuni S, Rulli E, et al. Systematic Review and Meta-Analysis on Neuropsychological Effects of Long-Term Use of Opioids in Patients With Chronic Noncancer Pain. Pain Pract. 2019;19(3):328–343. doi:10.1111/papr.12741
24. Moulin DE, Iezzi A, Amireh R, Sharpe WKJ, Boyd D, Merskey H. Randomised trial of oral morphine for chronic non-cancer pain. Lancet. 1996;347(8995):143–147. doi:10.1016/S0140-6736(96)90339-6
25. Raja SN, Haythornthwaite JA, Pappagallo M, et al. Opioids versus antidepressants in postherpetic neuralgia: A randomized, placebo-controlled trial. Neurology. 2002;59(7):1015–1021. doi:10.1212/WNL.59.7.1015
26. Haythornthwaite JA, Menefee LA, Quatrano-Piacentini AL, Pappagallo M. Outcome of chronic opioid therapy for non-cancer pain. J Pain Symptom Manage. 1998;15(3):185–194. doi:10.1016/S0885-3924(97)00352-7
27. Guerriero F, Roberto A, Greco MT, Sgarlata C, Rollone M, Corli O. Long-term efficacy and safety of oxycodone–naloxone prolonged release in geriatric patients with moderate-to-severe chronic noncancer pain: A 52-week open-label extension phase study. Drug Des Devel Ther. 2016;19(10):1515–1523. doi:10.2147/DDDT.S106025
28. Guerriero F, Sgarlata C, Marcassa C, Ricevuti G, Rollone M. Efficacy and tolerability of low-dose oral prolonged-release oxycodone/naloxone for chronic nononcological pain in older patients. Clin Interv Aging. 2014;16(10):1–11. doi:10.2147/CIA.S72521
29. Agarwal S, Polydefkis M, Block B, Haythornthwaite J, Raja SN. Transdermal fentanyl reduces pain and improves functional activity in neuropathic pain states. Pain Med. 2007;8(7):554–562. doi:10.1111/j.1526-4637.2006.00246.x
30. Higgins DM, Martin AM, Baker DG, Vasterling JJ, Risbrough V. The relationship between chronic pain and neurocognitive function a systematic review. Clin J Pain. 2018;34(3):262–275. doi:10.1097/AJP.0000000000000536
31. Kurita GP, Højsted J, Sjøgren P. Tapering off long-term opioid therapy in chronic non-cancer pain patients: A randomized clinical trial. Eur J Pain. 2018;22(8):1528–1543. doi:10.1002/ejp.1241
32. Von Elm E, Egger M, Altman DG, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Br Med J. 2007;335(7624):806–808. doi:10.1136/bmj.39335.541782.AD
33. Randolph C, Tierney MC, Mohr E, Chase TN. The Repeatable Battery for the Assessment of Neuropsychological Status (RBANS): preliminary clinical validity. J Clin Exp Neuropsychol. 1998;20(3):310–319. doi:10.1076/jcen.20.3.310.823
34. Bowie CR, Harvey PD. Administration and interpretation of the Trail Making Test. Nat Protoc. 2006;1(5):2277–2281. doi:10.1038/nprot.2006.390
35. O’Connell ME, Gould B, Ursenbach J, Enright J, Morgan DG. Reliable change and minimum clinically important difference (MCID) of the Repeatable Battery for the Assessment of Neuropsychology Status (RBANS) in a heterogeneous dementia sample: support for reliable change methods but not the MCID. Appl Neuropsychol. 2019;26(3):268–274. doi:10.1080/23279095.2017.1413575
36. Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale: an updated literature review. J Psychosom Res. 2002;52(2):69–77. doi:10.1016/S0022-3999(01)00296-3
37. Brazier JE, Harper R, Jones NMB, et al. Validating the SF-36 health survey questionnaire: new outcome measure for primary care.. Br Med J. 1992;305(6846):160–164. doi:10.1136/bmj.305.6846.160
38. Garratt AM, Stavem K. Measurement properties and normative data for the Norwegian SF-36: results from a general population survey. Health Qual Life Outcomes. 2017;15(1). doi:10.1186/s12955-017-0625-9
39. The Centers for Medicare and Medicaid Services (CMS). Department of Health and Human Services (HHS). CDC. Opioid Oral Morphine Milligram Equivalent (MME) Conversion Factors. www.cms.gov/Medicare/Prescription-Drug-Coverage/PrescriptionDrugCovContra/Downloads/Oral-MME-CFs-vFeb-2018.pdf.
40. Frank JW, Lovejoy TI, Becker WC, et al. Patient outcomes in dose reduction or discontinuation of long-term opioid therapy: A systematic review. Ann Intern Med. 2017;167(3):181–191. doi:10.7326/M17-0598
41. Foti M, Baker K, Jastrzab L, Stringer E, Mackey S, Younger J. Improvements in cognition following opioid detoxification program. J Pain. 2013;14(4):76. doi:10.1016/j.jpain.2013.01.641
42. Phillips R, Qi G, Collinson SL, et al. The minimum clinically important difference in the repeatable battery for the assessment of neuropsychological status. Clin Neuropsychologist. 2015;29(7):905–923. doi:10.1080/13854046.2015.1107137
43. Weiner DK, Rudy TE, Morrow L, Slaboda J, Lieber S. The relationship between pain, neuropsychological performance, and physical function in community-dwelling older adults with chronic low back pain. Pain Med. 2006;7(1):60–70. doi:10.1111/j.1526-4637.2006.00091.x
44. Moriarty O, McGuire BE, Finn DP. The effect of pain on cognitive function: A review of clinical and preclinical research. Prog Neurobiol. 2011;93(3):385–404. doi:10.1016/j.pneurobio.2011.01.002
45. Berna C, Kulich RJ, Rathmell JP. Tapering long-term opioid therapy in chronic noncancer pain: evidence and recommendations for everyday practice. Mayo Clin Proc. 2015;90(6):828–842. doi:10.1016/j.mayocp.2015.04.003
46. Elliott TE, Renier CM, Palcher JA. Chronic pain, depression, and quality of life: correlations and predictive value of the SF-36. Pain Med. 2003;4(4):331–339. doi:10.1111/j.1526-4637.2003.03040.x
47. Younger JW, Chu LF, D’Arcy NT, Trott KE, Jastrzab LE, Mackey SC. Prescription opioid analgesics rapidly change the human brain. Pain. 2011;152(8):1803–1810. doi:10.1016/j.pain.2011.03.028
48. Matarazzo JD, Wiens AN, Matarazzo RG, Goldstein SG. Psychometric and clinical test-retest reliability of the halstead impairment index in a sample of healthy, young, normal men. J Nerv Ment Dis. 1974;158(1):37–49. doi:10.1097/00005053-197401000-00006
49. SSAI. Abstracts for the 2019 scandinavian society of anaesthesiology and intensive care medicine congress in copenhagen. Acta Anaesthesiol Scand. 2019;63(8):e1–e48. doi:10.1111/aas.13442
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

