Back to Journals » Journal of Pain Research » Volume 14
Cognitive Function and White Matter Lesions in Medication-Overuse Headache
Authors Xiang Y, Chen S, Lin H, Xiong W, Zheng Z
Received 8 March 2021
Accepted for publication 9 May 2021
Published 17 June 2021 Volume 2021:14 Pages 1845—1853
DOI https://doi.org/10.2147/JPR.S310064
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Alexandre F DaSilva
Yue Xiang,1 Shenggen Chen,2 Hanbin Lin,2 Wenting Xiong,2 Zhenyang Zheng2
1Department of Nursing, Fujian Health College, Fuzhou, 350101, People’s Republic of China; 2Department of Neurology, Fujian Medical University Union Hospital, Fuzhou, 350001, People’s Republic of China
Correspondence: Zhenyang Zheng
Department of Neurology, Fujian Medical University Union Hospital, Fuzhou, Fujian, People’s Republic of China
Tel +86-591-83357896
Email [email protected]
Purpose: This study was designed to investigate the cognitive function and the white matter lesions (WMLs) and the relationship between them in medication-overuse headache (MOH) patients.
Methods: Subjects were enrolled and performed Montreal Cognitive Assessment (MoCA, Chinese-Beijing Version), Hamilton Anxiety Rating Scale (HAMA), Hamilton Depression Rating Scale (HAMD-24), and Pittsburgh Sleep Quality Index (PSQI) to evaluate the general cognitive function, anxiety, depression and sleep quality, and they were divided into three groups according to the MoCA scores: healthy controls, MOH with normal cognition group and MOH with cognitive impairment group. All the participants underwent MRI scans and images were obtained for WML evaluation with Fazekas scale.
Results: One hundred thirty-four participants were enrolled into this study, 46 of them for healthy controls, and 88 for MOH patients, 40 of the MOH patients for MOH with cognitive impairment group, and 48 for MOH with normal cognition group. MOH patients had significantly lower MoCA scores, including the scores of visuospatial and executive function, attention, and orientation, while they had significantly greater HAMA scores, HAMD-24 scores, PSQI scores, and deep white matter hyperintensity scores compared to healthy controls. And in MOH patients, the age, disease duration, monthly headache days, and periventricular white matter hyperintensity scores in patients with cognitive impairment were greater than those in patients with normal cognition. Moreover, the MoCA scores were negatively related to age, disease duration, monthly headache days, and Fazekas scale scores, and disease duration and monthly headache days were significant predictors of cognitive impairment in MOH patients.
Conclusion: MOH patients showed cognitive impairment and increased WML burden. And in MOH patients, cognitive function was negatively related to WML burden, and disease duration and monthly headache days were potential predictors of cognitive impairment. Prompt and effective treatment to stop the progression of the disease may alleviate cognitive impairment in MOH patients.
Keywords: medication-overuse headache, cognitive function, white matter lesions, risk factor
Introduction
Medication-overuse headache (MOH) is defined as a chronic headache that occurs on 15 or more days per month for more than 3 months in patients with a pre-existing primary headache caused by overuse of symptomatic headache medications, and the overall prevalence of MOH in the general population is about 1–2%.1 According to the Global Burden of Disease Study 2015, MOH is the 20th cause of disability worldwide, which causes an impairment in the quality of life for sufferers and causes a heavy financial burden on society.2
As a type of common chronic headache which developed from primary headache, MOH possessed longer disease duration and more attack frequencies. Neuroimaging studies indicated an increased prevalence of brain white matter lesions (WMLs) in migraine patients,3,4 and disease duration and headache attack frequency were indicators of WMLs in migraine.5,6 Moreover, our previous study suggested that WMLs were more prevalent in MOH patients.7
Cross-sectional studies showed that cognitive impairment was frequent in patients with chronic migraine and patients with chronic tension-type headache,8–10 and migraine and tension-type headache were also associated with non-vascular dementia.11 Our recent study found that the risk of cognitive decline was elevated in MOH patients.12
WMLs were associated with impaired cognitive function,13 and the severity of WMLs at baseline was associated with the cognitive decline in the non-demented elderly over time.14 However, the relationship between cognitive function and WMLs in MOH patients was not yet clear. This study was performed to investigate the cognitive function and WMLs and the relationship between them in MOH patients.
Methods
Participants
This cross-sectional study was conducted between June 2016 and October 2019. The participants were recruited from the MOH patients attending the Department of Neurology, Fujian Medical University Union Hospital. Only patients who met all the following criteria were enrolled in the study: (a) diagnosis of MOH based on the third edition of the International Classification of Headache Disorders (beta version);15 (b) headache duration ≥ 1 year; (c) without preventive treatment or detoxification before; (d) age between 18–80; (e) absence of dementia, including Alzheimer’s disease, vascular dementia, and frontal temporal dementia, severe mental illness, neoplastic diseases, infectious diseases, rheumatic diseases or connective tissue diseases. Healthy subjects without a personal or family history of primary headache visiting our hospital for medical checkups during the study period were served as a healthy control group. All procedures performed in studies involving human participants were in accordance with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This study was approved by the Ethics Committee of Fujian Medical University Union Hospital and informed consent was obtained from all individual participants included in the study.
Baseline Information Collection
The age, sex, years of schooling, accompanied hypertension, diabetes, smoking history, underlying primary headache, disease duration, and monthly headache days of the participants were investigated. Smoking history was defined as smoking at least 3 cigarettes per day on average for more than one year.
Neuropsychology Assessment
General cognitive function, anxiety, depression, and sleep quality were assessed with Montreal Cognitive Assessment (MoCA, Chinese-Beijing Version) (www.mocatest.org), Hamilton Anxiety Rating Scale (HAMA),16 Hamilton Depression Rating Scale (HAMD-24),17 and Pittsburgh Sleep Quality Index (PSQI),18 respectively by two trained physicians (Shenggen Chen and Hanbin Lin) blind to the clinical data. MoCA scores more than 25 (of 30), HAMA scores less than 7 (of 56), HAMD-24 scores less than 8 (of 76), and PSQI scores less than 7 (of 21) were classified as normal. According to the MoCA scores, the recruited MOH patients were divided into two groups, ie, patients with MoCA scores of more than 25 were classified into MOH with normal cognition group, and patients with MoCA scores of less than 26 were classified into MOH with cognitive impairment group.
MRI Evaluation
A 3.0-tesla MRI scanner (Prisma, Siemens Medical Systems, Erlangen, Germany) was employed to acquire images. The MRI protocol consisted of axial T1-weighted images (TR/TE, 2500 ms/10 ms), axial T2-weighted images (TR/TE, 4500 ms/80 ms), and coronal FLAIR images (TR/TE, 8000 ms/100 ms). For each image series, 35 slices covering the entire brain (matrix 224 × 224; FOV 224 mm × 224 mm; slice thickness 4.0 mm without gap) were obtained.
WMLs were defined as hyperintense focal lesions on T2-weighted and FLAIR images and iso- or hypo-intense on T1-weighted images. WMLs were scored with Fazekas scale by two trained raters (Yue Xiang and Wenting Xiong) blind to the clinical data on a consensus basis. Fazekas scale scores were developed as a sum of periventricular white matter hyperintensity scores and deep white matter hyperintensity scores. Periventricular white matter hyperintensity was graded as 0 = absence, 1 = “caps” or pencil-thin lining, 2 = smooth “halo”, 3 = irregular periventricular hyperintensity extending into the deep white matter. Deep white matter hyperintensity was graded as 0 = absence, 1 = punctate foci, 2 = beginning confluence of foci, 3 = large confluent areas.19
Statistical Analysis
Normality tests were performed to reveal the distribution of age, years of schooling, disease duration, monthly headache days, MoCA scores, HAMA scores, HAMD-24 scores, PSQI scores, and Fazekas scale scores before statistical analysis. For normally distributed data, they were expressed as the mean and standard deviation (SD), and the differences between groups were tested with independent samples t-test. For non-normally distributed data, they were expressed as the median and inter-quartile range (IQR), and the differences between groups were tested with Mann–Whitney U-test. Differences in sex, accompanied hypertension, diabetes, and smoking history were tested with chi-square test. Correlations between MoCA scores and age, years of schooling, disease duration, monthly headache days, HAMA scores, HAMD-24 scores, PSQI scores, and Fazekas scale scores were analyzed using Spearman correlation analysis. Binary logistic regression models were used to estimate the risk factors for cognitive impairment in MOH patients. Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated. A two-tailed P-value < 0.05 was considered statistically significant. All statistical analyses were performed using IBM SPSS Version 26.0 for Windows (SPSS Inc., Chicago, IL, USA).
Results
Baseline Information
Forty-six healthy controls (27 women, 19 men) and eighty-eight MOH patients (49 women, 39 men) who met the inclusion criteria were enrolled into this study, 40 of the MOH patients for MOH with cognitive impairment group and 48 for MOH with normal cognition group. The drugs overused by MOH patients in our study included acetaminophen, ibuprofen, aminopyrine, phenacetin, diclofenac, loxoprofen, propyphenazone, aspirin, and combinations of simple analgesics. The age, sex, years of schooling, the incidence of hypertension, the incidence of diabetes, and the incidence of smoking history between healthy controls and MOH patients showed no significant difference (Table 1). The sex, years of schooling, the incidence of hypertension, the incidence of diabetes, the incidence of smoking history, and the incidence of migraine as primary headache between MOH patients with cognitive impairment and MOH patients with normal cognition showed no significant difference. However, the age, disease duration, and monthly headache days in MOH patients with cognitive impairment were greater than those in MOH patients with normal cognition (Table 2).
 |
Table 1 Demographic Characteristic of Study Participants |
 |
Table 2 Demographic Characteristic of MOH Patients |
Neuropsychology Assessment
MOH patients had significantly lower MoCA scores compared to healthy controls, including the scores of visuospatial and executive function, attention, and orientation, while HAMA scores, HAMD-24 scores, and PSQI scores in MOH patients were greater than those in healthy controls (Table 3). The HAMA scores, HAMD-24 scores, and PSQI scores between MOH patients with cognitive impairment and MOH patients with normal cognition showed no significant difference (Table 4).
 |
Table 3 Neuropsychology Assessment in Study Participants |
 |
Table 4 Neuropsychology Assessment in MOH Patients |
WML Evaluation
Fazekas scale showed that MOH patients had significantly greater deep white matter hyperintensity scores compared to healthy controls, while periventricular white matter hyperintensity scores between them showed no significant difference (Table 5). Periventricular white matter hyperintensity scores in MOH patients with cognitive impairment were greater than that in MOH patients with normal cognition, while deep white matter hyperintensity scores between them showed no significant difference (Table 6).
 |
Table 5 WMLs in Study Participants |
 |
Table 6 WMLs in MOH Patients |
Correlations Between MoCA Scores and Baseline Information, HAMA Scores, HAMD-24 Scores, PSQI Scores, and Fazekas Scale Scores in MOH Patients
In MOH patients, MoCA scores were negatively related to age (r = −0.315, P = 0.003), disease duration (r = −0.584, P < 0.001), monthly headache days (r = −0.494, P < 0.001), and Fazekas scale scores (r = −0.463, P < 0.001; Table 7).
 |
Table 7 Correlations Between MoCA Scores and Baseline Information, HAMA Scores, HAMD-24 Scores, PSQI Scores, and Fazekas Scale Scores in MOH Patients |
Risk Factors for Cognitive Impairment in MOH Patients
Univariate logistic regression analysis revealed that age, disease duration, monthly headache days, and Fazekas scale scores were the independent risk factors for cognitive impairment in MOH patients (P < 0.05), while years of schooling, HAMA scores, HAMD-24 scores, PSQI scores, sex, accompanied hypertension, diabetes, smoking history, and underlying primary headache were not the independent risk factors (P > 0.05; Table 8). Therefore, four covariates, including age, disease duration, monthly headache days, and Fazekas scale scores, were included in our final multivariate logistic regression model to estimate the potential risk factors for cognitive impairment in MOH patients. Disease duration and monthly headache days were found to be significant predictors of cognitive impairment in MOH patients (OR, 1.31; 95% CI, 1.11–1.55; P = 0.002 and OR, 1.42; 95% CI, 1.20–1.68; P < 0.001 respectively; Table 9).
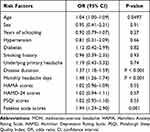 |
Table 8 Risk Factors for Cognitive Impairment in MOH Patients (Univariate Logistic Regression Analysis) |
 |
Table 9 Risk Factors for Cognitive Impairment in MOH Patients (Multivariate Logistic Regression Model) |
Discussion
Our study indicated that MOH patients had significantly lower MoCA scores, especially in the domains of visuospatial and executive function, attention, and orientation, while they had significantly greater HAMA scores, HAMD-24 scores, PSQI scores, and deep white matter hyperintensity scores compared to healthy controls. And in MOH patients, the age, disease duration, monthly headache days, and periventricular white matter hyperintensity scores in patients with cognitive impairment were greater than those in patients with normal cognition. Moreover, the MoCA scores were negatively related to age, disease duration, monthly headache days, and Fazekas scale scores, and disease duration and monthly headache days were significant predictors of cognitive impairment in MOH patients.
MOH patients demonstrated impaired general cognition as indicated by lowered MoCA scores, particularly in the domains of visuospatial and executive function, attention, and orientation. Altered volume in cerebellum and regions related to affection and cognitive processing (right lateral orbital gyrus), visual (left calcarine, bilateral middle occipital gyrus, right superior parietal lobe, optic chiasm), and auditory (right temporal transverse gyrus) perception was observed in MOH patients,20 which could be a morphological basis of cognitive impairment in MOH. Besides, MOH patients possessed prolonged P3 latency and lowered P3 amplitude, which could provide electrophysiological evidence for cognitive impairment in MOH.21
MOH was considered to be associated with psychiatric comorbidities such as depression, anxiety, and insomnia,22 and these comorbidities could be risk factors in the evolution of migraine into MOH.23,24 Increasing headache frequency was associated with risk of occurrence of anxiety, depression, and insomnia,25 and higher migraine frequency was correlated with greater symptom scores of anxiety and depression.26 MOH patients showed a high rate of depression and anxiety, which could negatively affect their headache attack,27 and depression and anxiety were found to be negative predictors in terms of treatment response in chronic migraine patients with or without medication-overuse.28–30 Moreover, lowered depression scores predicted a positive outcome of MOH detoxification.31 Furthermore, the volume of lower hippocampal subfields was negatively related to anxiety conditions in MOH patients.32
Recent studies suggested an increased prevalence of WMLs in migraine patients, especially deep WMLs,33 and our previous study showed that MOH patients had a greater prevalence of high WML load and they were at elevated risk of high deep WMLs load compared to healthy controls,7 which was in line with our finding that MOH patients possessed greater deep white matter hyperintensity scores compared to healthy controls.
We found that MoCA scores were negatively related to Fazekas scale scores in MOH patients, and periventricular white matter hyperintensity scores in patients with cognitive impairment were greater than that in patients with normal cognition. WMLs were implicated in the progression of cognitive impairment, and WMLs located at different regions, including periventricular and deep WMLs, evolved differently. A systematic review suggested that periventricular WMLs could have a significant negative impact on the cognition of older adults.34 To be more precise, frontal WMLs in the proximity of the frontal ventricles mainly affected executive function and parieto-temporal WMLs in the proximity of the posterior horns deteriorated memory.35 Moreover, the frontal component of periventricular WMLs was associated with pronounced cortical atrophy, and the dorsal component of periventricular WMLs showed associations with the cognitive decline.36 Additionally, periventricular WMLs were involved in the rate of cognitive decline.37 The underlying mechanisms of cognitive impairment caused by periventricular WMLs included impairment of nodal path length in the left opercular part of the inferior frontal gyrus,38 decreased regional cortical grey matter blood flow,39 disproportionate progressive hippocampal atrophy,40 and cortical atrophy.41
Age was associated with cognitive impairment among MOH patients. Age-related cognitive changes, including neuronal structure alterations, synapse loss, and neuronal network dysfunction result in brain structural and functional changes, and age-related diseases accelerate neuronal dysfunction, neuronal loss, and cognitive decline.42
Migraine has been linked to an increased prevalence of cognitive impairment, and the duration and frequency of migraine affect cognitive function.43 WMLs are more prevalent in migraine patients, and the disease duration and attack frequency have key roles in the formation of WMLs.6 WMLs may media the development of cognitive impairment in migraine. MOH patients had a high prevalence of cognitive impairment and WML burden,7 and the cognitive function was negatively related to WML burden. Our study indicated that the disease duration and headache frequency were the potential predictors of cognitive impairment in MOH patients. It could be assumed that longer disease duration and higher headache frequency in MOH could cause more serious WMLs, which would consequently lead to cognitive impairment. Further studies are needed to elucidate the mechanisms of the prevalence of cognitive impairment and WMLs in MOH.
Several limitations in this study should be considered when interpreting the findings. Firstly, the cross-sectional survey of this study indicates associations between cognitive impairment and some risk factors. However, this study cannot determine whether these associations are causal. Additional longitudinal cohort studies will be needed to carry out the evaluations. Secondly, due to the strict inclusion criteria, a relatively small number of participants were enrolled into this study. Additional studies with a larger sample size are required to confirm our results.
Conclusion
MOH patients showed cognitive impairment and increased WML burden. And in MOH patients, cognitive function was negatively related to WML burden, and disease duration and monthly headache days were potential predictors of cognitive impairment. Our findings indicate that prompt and effective treatment to stop the progression of the disease may alleviate cognitive impairment in MOH patients.
Acknowledgments
This work was supported by grants from the Training Project for Young and middle-aged core talents in the Health system of Fujian province (grant No. 2017-ZQN-38), Natural Science Foundation of Fujian province (grant No. 2017J05126), and Sailing Fund Project of Fujian Medical University (grant No. 2016QH022).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Headache Classification Committee of the International Headache Society (IHS). The international classification of headache disorders, 3rd edition. Cephalalgia. 2018;38(1):1–211. doi:10.1177/0333102417738202
2. Vos T, Allen C, Arora M, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1545–1602.
3. Palm-Meinders IH, Koppen H, Terwindt GM, et al. Structural brain changes in migraine. JAMA. 2012;308(18):1889–1897. doi:10.1001/jama.2012.14276
4. Kurth T, Mohamed S, Maillard P, et al. Headache, migraine, and structural brain lesions and function: population based epidemiology of vascular ageing-MRI study. BMJ. 2011;342:c7357. doi:10.1136/bmj.c7357
5. Schmitz N, Admiraal-Behloul F, Arkink EB, et al. Attack frequency and disease duration as indicators for brain damage in migraine. Headache. 2008;48(7):1044–1055. doi:10.1111/j.1526-4610.2008.01133.x
6. Trauninger A, Leel-Ossy E, Kamson DO, et al. Risk factors of migraine-related brain white matter hyperintensities: an investigation of 186 patients. J Headache Pain. 2011;12(1):97–103. doi:10.1007/s10194-011-0299-3
7. Zheng Z, Xiao Z, Shi X, et al. White matter lesions in chronic migraine with medication overuse headache: a cross-sectional MRI study. J Neurol. 2014;261(4):784–790. doi:10.1007/s00415-014-7267-1
8. Qu P, Yu JX, Xia L, Chen GH. Cognitive performance and the alteration of neuroendocrine hormones in chronic tension-type headache. Pain Pract. 2018;18(1):8–17. doi:10.1111/papr.12574
9. Latysheva N, Filatova E, Osipova D, Danilov AB. Cognitive impairment in chronic migraine: a cross-sectional study in a clinic-based sample. Arq Neuropsiquiatr. 2020;78(3):133–138. doi:10.1590/0004-282x20190159
10. Ferreira KS, Teixeira CT, Cáfaro C, et al. Chronic migraine patients show cognitive impairment in an extended neuropsychological assessment. Arq Neuro Psiquiat. 2018;76(9):582–587. doi:10.1590/0004-282x20180085
11. Tzeng NS, Chung CH, Lin FH, et al. Headaches and risk of dementia. Am J Med Sci. 2017;353(3):197–206. doi:10.1016/j.amjms.2016.12.014
12. Cai X, Xu X, Zhang A, et al. Cognitive decline in chronic migraine with nonsteroid anti-inflammation drug overuse: a cross-sectional study. Pain Res Manag. 2019;2019:7307198. doi:10.1155/2019/7307198
13. Ashrafi F, Taheri MS, Farzaneh A, Behnam B, Ahmadi MA. Cognitive functions and white matter lesions on magnetic resonance images in a sample of normal Iranian population with cardiovascular risk factors. Neuroradiol J. 2019;32(2):108–114. doi:10.1177/1971400919825862
14. Qi X, Tang H, Luo Q, et al. White matter hyperintensities predict cognitive decline: a community-based study. Can J Neurol Sci. 2019;46(4):383–388. doi:10.1017/cjn.2019.47
15. Ettlin DA. The international classification of headache disorders, 3rd edition (beta version). Cephalalgia. 2013;33(9):629–808. doi:10.1177/0333102413485658
16. Hamilton M. Development of a rating scale for primary depressive illness. Br J Soc Clin Psychol. 1967;6(4):278–296. doi:10.1111/j.2044-8260.1967.tb00530.x
17. Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi:10.1136/jnnp.23.1.56
18. Buysse DJ, Reynolds CR, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi:10.1016/0165-1781(89)90047-4
19. Fazekas F, Chawluk JB, Alavi A, Hurtig HI, Zimmerman RA. MR signal abnormalities at 1.5 T in Alzheimer’s dementia and normal aging. AJR Am J Roentgenol. 1987;149(2):351–356. doi:10.2214/ajr.149.2.351
20. Chen X, Chen Z, Dong Z, Liu M, Yu S. Morphometric changes over the whole brain in caffeine-containing combination-analgesic-overuse headache. Mol Pain. 2018;14:2070384879. doi:10.1177/1744806918778641
21. Xu C, Liu H, Wen Q, Wang R. Clinical research of the cognitive function and event-related potential P300 in patients with medication-overuse headache. Chin J Diagn. 2014;2(1):58–60.
22. Diener HC, Holle D, Solbach K, Gaul C. Medication-overuse headache: risk factors, pathophysiology and management. Nat Rev Neurol. 2016;12(10):575–583. doi:10.1038/nrneurol.2016.124
23. Radat F, Creac’H C, Swendsen JD, et al. Psychiatric comorbidity in the evolution from migraine to medication overuse headache. Cephalalgia. 2005;25(7):519–522. doi:10.1111/j.1468-2982.2005.00910.x
24. Viana M, Bottiroli S, Sances G, et al. Factors associated to chronic migraine with medication overuse: a cross-sectional study. Cephalalgia. 2018;38(14):2045–2057. doi:10.1177/0333102418761047
25. Buse DC, Reed ML, Fanning KM, et al. Comorbid and co-occurring conditions in migraine and associated risk of increasing headache pain intensity and headache frequency: results of the migraine in America symptoms and treatment (MAST) study. J Headache Pain. 2020;21(1):23. doi:10.1186/s10194-020-1084-y
26. Chu HT, Liang CS, Lee JT, et al. Associations between depression/anxiety and headache frequency in migraineurs: a cross-sectional study. Headache. 2018;58(3):407–415. doi:10.1111/head.13215
27. Migliore S, Paolucci M, Quintiliani L, et al. Psychopathological comorbidities and clinical variables in patients with medication overuse headache. Front Hum Neurosci. 2020;14:571035. doi:10.3389/fnhum.2020.571035
28. Schiano DCF, Caratozzolo S, Liberini P, Rao R, Padovani A. Response predictors in chronic migraine: medication overuse and depressive symptoms negatively impact onabotulinumtoxin-a treatment. Front Neurol. 2019;10:678. doi:10.3389/fneur.2019.00678
29. Disco C, Bellamio M, Fuccaro M, et al. O051. Chronic migraine and onabotulinumtoxin A: a prospective study on patients treated at the Headache Centre of the Padua University and analysis of possible predictors of responsivity. J Headache Pain. 2015;16(Suppl 1):A98. doi:10.1186/1129-2377-16-S1-A98
30. Probyn K, Bowers H, Caldwell F, et al. Prognostic factors for chronic headache: a systematic review. Neurology. 2017;89(3):291–301. doi:10.1212/WNL.0000000000004112
31. Bottiroli S, Allena M, Sances G, et al. Psychological, clinical, and therapeutic predictors of the outcome of detoxification in a large clinical population of medication-overuse headache: a six-month follow-up of the COMOESTAS project. Cephalalgia. 2019;39(1):135–147. doi:10.1177/0333102418783317
32. Chen Z, Chen X, Liu M, Ma L, Yu S. Lower hippocampal subfields volume in relation to anxiety in medication-overuse headache. Mol Pain. 2018;14:2070402263. doi:10.1177/1744806918761257
33. Kruit MC, van Buchem MA, Launer LJ, Terwindt GM, Ferrari MD. Migraine is associated with an increased risk of deep white matter lesions, subclinical posterior circulation infarcts and brain iron accumulation: the population-based MRI CAMERA study. Cephalalgia. 2010;30(2):129–136. doi:10.1111/j.1468-2982.2009.01904.x
34. Bolandzadeh N, Davis JC, Tam R, Handy TC, Liu-Ambrose T. The association between cognitive function and white matter lesion location in older adults: a systematic review. Bmc Neurol. 2012;12:126. doi:10.1186/1471-2377-12-126
35. Lampe L, Kharabian-Masouleh S, Kynast J, et al. Lesion location matters: the relationships between white matter hyperintensities on cognition in the healthy elderly. J Cereb Blood Flow Metab. 2019;39(1):36–43. doi:10.1177/0271678X17740501
36. Habes M, Sotiras A, Erus G, et al. White matter lesions: spatial heterogeneity, links to risk factors, cognition, genetics, and atrophy. Neurology. 2018;91(10):e964–e975. doi:10.1212/WNL.0000000000006116
37. De Groot JC, De Leeuw FE, Oudkerk M, et al. Periventricular cerebral white matter lesions predict rate of cognitive decline. Ann Neurol. 2002;52(3):335–341. doi:10.1002/ana.10294
38. Yang D, Huang L, Luo C, et al. Impaired structural network properties caused by white matter hyperintensity related to cognitive decline. Front Neurol. 2020;11:250. doi:10.3389/fneur.2020.00250
39. Bahrani AA, Powell DK, Yu G, Johnson ES, Jicha GA, Smith CD. White matter hyperintensity associations with cerebral blood flow in elderly subjects stratified by cerebrovascular risk. J Stroke Cerebrovasc Dis. 2017;26(4):779–786. doi:10.1016/j.jstrokecerebrovasdis.2016.10.017
40. Fiford CM, Manning EN, Bartlett JW, et al. White matter hyperintensities are associated with disproportionate progressive hippocampal atrophy. Hippocampus. 2017;27(3):249–262. doi:10.1002/hipo.22690
41. Zi W, Duan D, Zheng J. Cognitive impairments associated with periventricular white matter hyperintensities are mediated by cortical atrophy. Acta Neurol Scand. 2014;130(3):178–187. doi:10.1111/ane.12262
42. Murman D. The impact of age on cognition. Semin Hear. 2015;36(03):111–121. doi:10.1055/s-0035-1555115
43. Huang L, Juan DH, Wang X, Wang Y, Xiao Z. Duration and frequency of migraines affect cognitive function: evidence from neuropsychological tests and event-related potentials. J Headache Pain. 2017;18(1):54. doi:10.1186/s10194-017-0758-6
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
