Back to Journals » Cancer Management and Research » Volume 13
Clinico-Pathological Findings and Spatial Distributions of Esophageal Cancer in Arsi Zone, Oromia, Central Ethiopia
Authors Deybasso HA , Roba KT , Nega B, Belachew T
Received 22 January 2021
Accepted for publication 12 March 2021
Published 23 March 2021 Volume 2021:13 Pages 2755—2762
DOI https://doi.org/10.2147/CMAR.S301978
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Eileen O'Reilly
Haji Aman Deybasso,1 Kedir Teji Roba,2 Berhanu Nega,3 Tefera Belachew1
1Jimma University, Department of Human Nutrition and Dietetics, Jimma, Ethiopia; 2Haramaya University, College of Health and Medical Sciences, Harar, Ethiopia; 3Addis Ababa University, College of medicine and health sciences, Addis Ababa, Ethiopia
Correspondence: Haji Aman Deybasso Tel +251911386781
Email [email protected]
Purpose: Arsi Zone is one of the esophageal cancer endemic areas and is reported to have a high incidence of esophageal cancer in Ethiopia. This study assessed clinicopathological patterns and spatial distributions of esophageal cancer in Arsi Zone, Oromia, Central Ethiopia.
Methods: A cross-sectional study design was carried out by abstracting data of 403 patients treated from January 2015 to January 2019. Data were collected by using a structured data collection form and Geographical Positioning System software. The collected data were summarized in the form of tables, figures, means, and standard deviations. Statistical data analysis was done using SPSS software version 21.0 while geospatial analysis was conducted using the Arc-GIS 10.1 software.
Results: The disease was prominent among individuals aged 50 to 59 years. The mean age of females and males was 52.2 (SD± 10.41) and 56.94 (SD ± 12.27) years respectively. The vast majority (98.3%) of cases had squamous cell carcinoma. Dysphagia with weight loss accounted for 87.6% of the presenting symptoms. A large proportion (42.9%) of patients had a tumor located at the lower thorax. The majority (62%) of patients were from the eastern and north-eastern parts of the Arsi zone.
Conclusion: Dysphagia with weight loss was the major symptom during the first visit. Squamous cell carcinoma was the predominant histopathological type. Eastern and the northeastern parts of the Zone are the most affected regions. Future studies should focus on the determinants of esophageal cancer and precise areas with high incidences by using the population and/or facility-based cancer registry systems.
Keywords: esophageal cancer, clinical pattern, geographical distribution, Arsi, Ethiopia
Introduction
Esophageal cancer (EC) is a malignant tumor that develops inside the esophagus as the result of alteration in epithelial linings.1 It is the 7th cancer in incidences and the 6th cause of cancer mortality in the world.2 World Health Organization (WHO) identified Squamous Cell Carcinoma (SCC) and Adenocarcinoma (AC) as the major tissue types of esophageal cancer.3 Adenocarcinoma is more prevalent in developed countries such as in the United States, United Kingdom, Scandinavia, France, Switzerland, Denmark, Italy, Slovakia, Netherlands, Australia, and New Zealand.4
Esophageal cancer has distinct geographical distributions within the country and across the globe.5 In Canada, rural parts of the Quebec region have higher incidences of EC than other parts.6 Similarly, considerable geographical variations were seen in the northeast and Midwest regions of America.7 Corresponding variations were observed in different regions of France, Denmark, and the Netherlands.8 Squamous cell carcinoma is the predominant type of EC in developing countries.9 Eastern Turkey, northeastern Iran, Kazakhstan, and northern and central China are the hot spot areas in Asia’s EC belt.10
Projection of cancer in Africa anticipated staggering increases in cancer corresponding to 1.27 million new cases and 0.97 million deaths in 2030.11 The incidences of EC were rare until the 1930s in East, Central, and Southern Africa.12 With gradual increases over time, eastern and southern Africa became the epicenter of esophageal carcinoma.5,13–15 Concentrations of EC cases were notably observed in rural and Eastern Cape provinces of South Africa,16 western parts of Kenya,17,18 among Darfurian tribes in Sudan,19 and populations living in Kilimanjaro areas in Tanzania.20
In Ethiopia, there is no reliable data on incidences of EC so far. Cancers of different organs account for about 5.8% of total national mortality.21 Arsi Zone was one of the EC endemic areas in Africa’s esophageal cancer belt for years,22 and a constantly reported high incidence area of EC in Ethiopia.23,24 An epidemiological study in the Oromia region showed that 68% of EC patients were from Arsi and neighboring Zone.25
Identifying a cluster of cases of EC within the endemic area is crucial in highlighting high-risk populations and generating hypotheses about the potential risk factors associated with that disease.23,24 Yet, except few observational studies at country and regional levels,23,25,26 no study has ever been conducted to assess the clinicopathological patterns and spatial distributions of esophageal cancer in esophageal cancer endemic areas in Ethiopia.
Therefore, this study was conducted to determine the clinicopathological patterns and spatial distributions of esophageal cancer in Arsi Zone, Oromia, Central Ethiopia.
Materials and Methods
Setting
Arsi Zone is found in the central part of the Oromia Regional State in central Ethiopia. Asella is the capital city of Arsi Zone located 175 Kilometers South East of Addis Ababa (the capital city of Ethiopia). Data were collected from surgical, oncology, endoscopy, and pathology units of seven referral hospitals and four clinics that render diagnostic services, consultations, and cancer treatments (Additional File 1). The data collection period covers from January 1 to February 30, 2019.
Study Design
A cross-sectional study design was carried out by abstracting data of 403 patients treated from January 2015 to January 2019.
Source Population
All EC patients from Arsi Zone who visited the selected health facilities during the study period were considered as source populations.
Study Population
The study populations constituted radio-graphically diagnosed and pathologically confirmed EC patients from Arsi Zone.
Inclusion and Exclusion Criteria
Endoscopy and pathologically confirmed esophageal cancer patients with complete data were included. Records of 85 patients (78 documents with no endoscopy findings and 7 patients with incomplete address) were excluded from the study.
Data Collection Instrument and Procedures
Data were collected by five trained BSc nurses using close-ended questionnaires (checklists) that comprised demographic characteristics (age, sex, and residence), clinical, histopathological type of cancer, tumor location, degree of tumor differentiation, cancer stages, and the primary residences of the patients. The severity of dysphagia was graded as follows: grade 1: normal swallowing; grade 2: difficulty in swallowing solids; grade 3: difficulty in swallowing semisolids; grade 4: difficulty in swallowing liquids; grade 5: difficulty in swallowing own saliva. The clinical staging was performed using TNM (American Joint Committee on Cancer (AJCC) cancer staging manual); this is a staging system that is an expression of the anatomical extent of the disease based on the extent of the primary tumor (T), absence or presence of and extent of regional lymph node metastasis (N) and absence or presence of distant metastasis (M).27 The administrative units, geographical locations, and agro-climatic divisions were gathered from the Arsi Zone finance and economic development office while the topologies of the study area were collected by using Geographical Information System (GIS) obtained from the agriculture departments of Arsi Zone (Additional file1 2).
Data Processing and Analysis
Questionnaires were checked daily for accuracy, consistency, and completeness by supervisors. Furthermore, the supervisor and the principal investigator gave feedback and correction on daily basis. Patients were categorized into highland, midland, and lowland agro-climatic divisions. The information related to administrative units (Districts) was extracted from the map of Arsi Zone with a scale ratio of 1:1200. The extracted demographic information on spatial locations was geo-tagged to the database containing administrative districts from where patients came.
The categorical variables of the cases were analyzed by descriptive statistical methods and presented in the form of tables and figures. Continuous variables were summarized using means and standard deviations. Statistical data analysis was done using SPSS software version 21.0 (SPSS, Inc, Chicago, IL, USA).
Categorical attributes of the number of males and females were identified and the coordinates of the point were taken using Geographical Positioning System (GPS) at the district level. The number of EC patients per district was used for delineating and mapping the distributions of EC per district in the Arsi Zone. Arc-GIS 10.1 software was used to automatically mark out and map the burden of cancer s per districts by incorporating CSI, 2013 Ethio- GIS administrative data. Finally, different types of colors were used to indicate the burden of EC cancer per district based on the following category: Red color for the districts which had 31 and above patients, Pink color for the districts which had 21 to 30 patients yellow color for the districts which had 11 to 20 patients and Green color for the districts which have 1 to 10 patients.
Results
Patients’ Characteristics
Out of 403 patients whose cards were reviewed, 388 (96.3%) were rural residents. Two hundred nine (51.8%) patients were females. The male to female ratio was 0.93:1.0 with no statistically significant difference. The majority of patients (72.2% females vs 50.5% males) were below the age of 60 years. The overall mean age was 54.5 (SD±11.6) years. The mean age of female patients was 52.2 (SD±10.41) years which ranges from 25 to 85 years. The corresponding mean age for males was 56.94 (SD ±12.27) years with the age ranging from 19 to 88 years (Table 1).
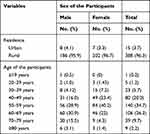 |
Table 1 Socio-Demographic Characteristics of EC Patients in Arsi Zone, Oromia, Ethiopia, 2020 |
Clinico-Pathological Characteristics
Concerning histopathological subtype, 396 (98.3%) cases had squamous cell carcinoma. The tumor was located at the lower thorax, mid thorax, and Gastroesophageal Junction (GEJ) among 42.9%, 26.1%, and 23.8% of patients, respectively. Furthermore, 168 (41.7%) of patients had moderately differentiated tumors while there were no conclusive reports on the degree of tumor differentiation for 47 (11.7%) cases. A greater number of patients (87.6%) had dysphagia and weight loss during the first visit. The majority (42.4%) of patients were at the third stage of cancer while cancer staging was not determined for 76 (18.9%) of patients (Table 2).
 |
Table 2 Clinico-Pathological Characteristics of Esophageal Cancer Patients in Arsi Zone, Oromia, Ethiopia, 2020 |
The Magnitude of Esophageal Cancer in the Arsi Zone
Cases of EC were recorded from 25 (96.2%) of the existing 26 districts of Arsi Zone. The majority of the patients were from Robe,28 Jaju,17 and Diksis29 districts followed by 21 to 30 patients being from Doddota, Sude, Zuway-Dugda, Lode-Hetosa, and Shirka districts. Seven districts (Amigna, Sire, Munessa, Merti, Chole, Lemu-Bilbilo, and Tiyo) accounted for 11 to 20 cases during the study period. The remaining ten districts (Bale, Guna, Gololcha, Honkolowabe, Hetosa, Seru, Tena, Aseko, Bekoji, and Digalu-Tijo) contributed one to 10 patients (Figure 1).
 |
Figure 1 The number of esophageal cancer patients per district in Arsi Zone, Oromia, Ethiopia, 2020. |
Spatial Distribution of Oesophageal Cancer
In this study, 141 (35%) of patients were from the Eastern parts of the Zone. The northeast, southeast, and northern parts of the zone had a total of 108 (26.8%), 47 (11.7%), and 31 (7.7%) patients respectively. Additionally, Asella town-and surrounding district (Tiyo) contributed to a total of 30 (7.4%) patients while 27 (6.7%) and 17 (4.2%) cases were found to be the residents of the western and southwest parts, in that order (Figure 2). Out of the total cases, 178 (44.2%), 137 (34.0%), and 88 (21.8%) patients were from the districts located in the highland, midland, and lowland agro-climatic divisions, respectively.
 |
Figure 2 Map showing the spatial distribution of esophageal cancer cases in Arsi Zone, Oromia, Ethiopia, 2020. |
Discussion
In this study, we attempted to review the clinicopathological patterns and spatial distributions of esophageal cancer in the Arsi Zone. Accordingly, vast proportions of the patients were rural residents similar to preceding studies that reported predominance of EC in rural areas.16,23,27,29 A high proportion of EC among rural residents may be attributed to exposure to various environmental and occupational carcinogens.17,29,30 Furthermore, Patel et.al.(2013) argued that the predominance of EC among rural populations is linked to infection from fungi and bacteria that replicate in grass-thatched houses.17 Moreover, inadequate nutrient intakes and lower socioeconomic status could be another risk factor associated with increased incidences of EC among the rural populations.31,32
In the present study, 7.1% of patients were ≤ 39 years of age and the youngest male and female patients were diagnosed at the age of 19 and 25 years, respectively. This is contradictory to the pathogenesis of EC that usually increases with age and attaining a climax after 70 years.1 Some studies in Africa also found increases in the proportion of young patients as early as 12 years of age.18,33 The proportion of youngest patients in this study is greater than the findings in Ethiopia,25 and Kenya.18 Observing EC among younger populations may indicate early childhood exposure to the carcinogens that may alter the natural pathogenesis of the disease.
Dysphagia with weight loss accounted for 87.6% of the presenting symptoms. Besides, the majority of the patients were at advanced stages of cancer. Dysphagia and late presentations became the cardinal presentations of EC patients in Ethiopia,23,25,26 Africa,16,17,30,34–36 and elsewhere.43,37,39,40 The reason could be that the esophagus has a remarkable capability to stretch until significantly blocked by a tumor.38 Besides, presenting at a late stage of cancer with dysphagia could be linked to failure to understand the early symptoms associated with esophageal carcinoma.
Squamous cell carcinoma was the dominant (98.3%) histo-pathological type similar to previous studies in Ethiopia.23,25,26,39 The finding is very conceivable since squamous cell carcinoma is the leading histopathological type of EC in developing countries.1,40,41 The lower thorax was the commonest anatomical site for a tumor followed by mid thorax and GEJ with no significant differences between male and female patients. The finding is similar to the studies that found the lower thorax as the commonest anatomical site of esophageal cancer34,39 but contrary to the studies that identified the middle thorax as a major cancer location in Ethiopia,23,26 Uganda,34 Tanzania,27 Ghana,28 and Pakistan.42 The inconsistencies in tumor locations can be explained by differences in the classification of the anatomic sites. In this study, tumor locations were based on Watanabe et.al, of five (Cervical, upper, mid, lower, and GEJ) anatomical sites for the carcinogenesis of EC3 contrary to other studies that used three (upper, mid, and lower) anatomical classifications.
The majority of the patients in this study had a moderately differentiated tumor differently from studies that found well-differentiated tumors among EC patients.23,31 The disparities might be because of lower inconclusive results in this study (11.7%) than the rate of undetermined pathological results (62.7%) in the aforementioned studies.
The geographical distribution of EC in the Arsi Zone showed asymmetrical patterns. About 62% of patients were from the eastern and north-eastern parts. The majority of the patients were from the Robe district followed by Jaju, Disksis, and Sude districts. Additionally, Doddota, Zuway-Dugda, Lode-Hetosa, and Shirka were succeeding districts in an increased number of cases. Besides, 44.2% of the cases were from the highland agro-climatic zone. The finding is in agreement with the study that reported high altitude areas as the main location of EC in the Arsi Zone.35 The predominance of EC in those areas seems to be related to the population sizes because the eastern, north-eastern, and highland agro-ecological zone are the most populated areas in Arsi Zone.43,44 In stratified analysis though, the effect of population sizes was not observed. For instance, the Robe district which had the highest number of cases encompasses equivalent population size (6.2% of the zonal population) to Munessa district that had only 4.2% of the total cases. Whereas, Jaju and Diksis districts that have lower populations had a higher number of patients than the Munessa district. Conversely, the 6th populated district (Digalu-tijo district) contributed to a single esophageal cancer patient.
Remarkably, greater numbers of patients were from contiguous districts that are located farther from the main referral hospital in the Zone. The clustering of EC at demarcated areas and the disparities between and within geographical locations are the peculiar characteristics of EC in Africa, Asia, and elsewhere.10,22,45,46 High prevalence of EC in geographically adjacent areas may signal the existence of potentially harmful factors in high burden areas than areas with a lower prevalence of esophageal cancer. Nevertheless, there is no established evidence whether the routinely reported “hot wheat porridge consumption” is widely practiced in higher burden districts of Arsi Zone. In the wake of increasing chronic diseases in developing countries like Ethiopia,11 the identified clinico-pathological findings and high-risk geographical areas can be used as the baseline for exploring the potential risk factors and designing preventive strategies.
Limitations
Being the retrospective study and absence of proper cancer registry systems influenced retrieving important sociodemographic and clinical information which might provide better perspectives to our study. Besides, identification of the patients’ residents at the district level may not exactly locate the patient’s exact agro-climatic areas due to existing overlapping in agro-ecological zones within the districts.
Conclusion
Dysphagia with weight loss was the major symptom during the first visit. Squamous cell carcinoma was the predominant histopathological type. Eastern and northeastern parts of the Arsi Zone are the most affected areas. The discrepancies in the geographical distribution of EC in the Arsi Zone may be primarily linked to differences in dietary practices, lifestyles, genetics, and exposure to environmental carcinogens. Education on early symptoms associated with EC and the benefit of timely seeking health care should be provided using various education channels. Future studies should focus mainly on the eastern and the northeastern parts of the Zone by using prospective studies through the population and/or facility-based cancer registry systems.
Abbreviations
AC, Adenocarcinoma; AJCC, American Joint Committee on Cancer; EC, Esophageal cancer; GEJ, Gastroesophageal junction; GIS, Geographical Information System; GPS, Geographical Positioning System; IRB, Institutions Research Board; REC, Research Ethical Committee; SCC, Squamous Cell Carcinoma; WHO, World Health Organization.
Data Sharing Statement
The datasets supporting the conclusions of this article are included in the article.
Ethics Approval and Consent to Participate
The study was approved by the Institutions Research Board (IRB) of Jimma University and it was conducted in accordance with the Declaration of Helsinki. The study participant’s consent was waived by the review board as the study was conducted through a review of medical records. Permission to collect data was secured from respective health facilities. Confidentiality of the information was maintained by excluding personally identifiable information on the questionnaires.
Acknowledgment
The authors are very grateful to the members of staff in the medical records, surgery, oncology, and pathology departments of each health institution for their support and cooperation during data collection.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests.
References
1. Napier KJ. Esophageal cancer: a review of epidemiology, pathogenesis, staging workup, and treatment modalities. World J Gastrointest Oncol. 2014;6(5):112. doi:10.4251/wjgo.v6.i5.112
2. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. doi:10.3322/caac.21492
3. Watanabe N, Shimizu M, Kochi T, Shirakami Y, Tanaka T. Esophageal carcinogenesis. Open J Pathol. 2014;04(04):151–170. doi:10.4236/ojpathology.2014.44021
4. Siersema PD. Esophageal Cancer. Gastroenterol Clin North Am. 2008;37(4):943–964. doi:10.1016/j.gtc.2008.09.012
5. Mudan SS, Kang J-Y. Epidemiology and clinical presentation in esophageal cancer. In Rankin SC, editor. Carcinoma of the Esophagus. Cambridge: Cambridge University Press; 2007:1–13. Available from https://www.cambridge.org/core/product/identifier/CBO9780511545443A008/type/book_part.
6. Cattelan L, Ghazawi FM, Le M, et al. Epidemiologic trends and geographic distribution of esophageal cancer in Canada: a national population‐based study. Cancer Med. 2020;9(1):401–417. doi:10.1002/cam4.2700
7. Drahos J, Wu M, Anderson WF, et al. Regional variations in esophageal cancer rates by census region in the United States, 1999–2008. PLoS One. 2013;8(7):e67913. doi:10.1371/journal.pone.0067913
8. Melhado RE, Alderson D, Tucker O. The changing face of esophageal cancer. Cancers. 2010;2(3):1379–1404. doi:10.3390/cancers2031379
9. Kamangar F, Dores GM, Anderson WF. Patterns of cancer incidence, mortality, and prevalence across five continents: defining priorities to reduce cancer disparities in different geographic regions of the world. J Clin Oncol. 2006;24(14):2137–2150. doi:10.1200/JCO.2005.05.2308
10. Zhang H-Z, Jin G-F, Shen H-B. Epidemiologic differences in esophageal cancer between Asian and Western populations. Chin J Cancer. 2012;31(6):281–286. doi:10.5732/cjc.011.10390
11. Sylla BS, Wild CP. A million Africans a year dying from cancer by 2030: what can cancer research and control offer to the continent? Int J Cancer. 2012;130(2):245–250. doi:10.1002/ijc.26333
12. Sammon AM; scoafrica.org (Organization). Squamous cancer of the esophagus in Africa. Place of publication not identified: Scoafrica.org; 2009.
13. Munishi MO, Hanisch R, Mapunda O, et al. Africa’s oesophageal cancer corridor: do hot beverages contribute? Cancer Causes Control. 2015;26(10):1477–1486. doi:10.1007/s10552-015-0646-9
14. Parkin DM, Bray F, Ferlay J, Jemal A. Cancer in Africa 2012. Cancer Epidemiol Biomarkers Prev. 2014;23(6):953–966. doi:10.1158/1055-9965.EPI-14-0281
15. Middleton DRS, Bouaoun L, Hanisch R, et al. Esophageal cancer male to female incidence ratios in Africa: a systematic review and meta-analysis of geographic, time and age trends. Cancer Epidemiol. 2018;53:119–128. doi:10.1016/j.canep.2018.01.020
16. Alaouna M, Hull R, Penny C, Dlamini Z. Esophageal cancer genetics in South Africa. Clin Exp Gastroenterol. 2019;12:157–177. doi:10.2147/CEG.S182000
17. Patel K, Wakhisi J, Mining S, Mwangi A, Patel R. Esophageal cancer, the topmost cancer at MTRH in the Rift Valley, Kenya, and its potential risk factors. ISRN Oncol. 2013;2013:1–9. doi:10.1155/2013/503249
18. Parker RK, Dawsey SM, Abnet CC, White RE. Frequent occurrence of esophageal cancer in young people in western Kenya. Dis Esophagus. 2010;23(2):128–135. doi:10.1111/j.1442-2050.2009.00977.x
19. Gasmelseed N, Abudris D, Elhaj A, et al. Patterns of esophageal cancer in the National Cancer Institute at the University of Gezira, in Gezira State, Sudan, in 1999–2012. Asian Pac J Cancer Prev. 2015;16(15):6481–6490. doi:10.7314/APJCP.2015.16.15.6481
20. Gabel JV, Chamberlain RM, Ngoma T, et al. Clinical and epidemiologic variations of esophageal cancer in Tanzania. World J Gastrointest Oncol. 2016;8(3):314. doi:10.4251/wjgo.v8.i3.314
21. FMOH. Disease prevention and control directorate national cancer control plan for 2016–2020; 2015.
22. Schaafsma T, Wakefield J, Hanisch R, et al. Africa’s oesophageal cancer corridor: geographic variations in incidence correlate with certain micronutrient deficiencies. PLoS One. 2015;10(10):e0140107. doi:10.1371/journal.pone.0140107
23. Shewaye AB, Seme A. Risk factors associated with oesophageal malignancy among Ethiopian patients: a case control study. East Cent Afr J Surg. 2016;21(2):33. doi:10.4314/ecajs.v21i2.5
24. Alebachew Woldu M, Legese DA, Abamecha FE, Beyene Berha A. The prevalence of cancer and its associated risk factors among patients visiting oncology unit, Tikur Anbessa Specialized Hospital, Addis Ababa- Ethiopia. J Cancer Sci Ther. 2017;09(04).
25. Bulcha GG, Leon ME, Gwen M, Abnet CC, Sime A, Pritchett NR. Epidemiology of Esophageal Cancer (EC) In Oromia Region, Ethiopia 2016: a 4-year medical record review. J Global Oncol. 2018;4(Supplement2):14s–14s. doi:10.1200/jgo.18.41700
26. Wondimagegnehu A, Hirpa S, Abaya SW, et al. Oesophageal Cancer Magnitude and Presentation in Ethiopia [Internet]. In Review; Aug 2019 [
27. Mchembe MD, Rambau PF, Chalya PL, Jaka H, Koy M, Mahalu W. Endoscopic and clinicopathological patterns of esophageal cancer in Tanzania: experiences from two tertiary health institutions. World J Surg Oncol. 2013;11(1):257. doi:10.1186/1477-7819-11-257
28. Tettey M, Edwin F, Aniteye E, et al. The changing epidemiology of esophageal cancer in sub-Saharan Africa – the case of Ghana. Pan African Medical Journal. 2012;13:6.
29. Al-abed AAA, Tamil AM, Al-Dubai SAR. Case control study on risk factors associated with esophageal cancer in Yemen. BMC Public Health. 2012;12(S2):
30. Mlombe Y, Rosenberg N, Wolf L, et al. Environmental risk factors for oesophageal cancer in Malawi: a case-control study. Malawi Med J. 2015;27(3):88. doi:10.4314/mmj.v27i3.3
31. Samarasam I. Esophageal cancer in India: current status and future perspectives. Int J Adv Med Health Res. 2017;4(1):5. doi:10.4103/IJAMR.IJAMR_19_17
32. Goodarzi E, Sohrabivafa M, Haddad MHF, Naemi H, Khazaei Z. Esophagus cancer geographical distribution, incidence, mortality and their world Human Development Index (HDI) relationship: an ecology study. World Cancer Research Journal. 2019;6:e 1386
33. Dawsey SP, Tonui S, Parker RK, et al. Esophageal cancer in young people: a case series of 109 cases and review of the literature. PLoS One. 2010;5(11):e14080. doi:10.1371/journal.pone.0014080
34. Alema O, Iva B. Cancer of the esophagus; histopathological sub-types in northern Uganda. Afr Health Sci. 2014;14(1):17. doi:10.4314/ahs.v14i1.4
35. McCormack V, Menya D, Munishi M, et al. Informing aetiologic research priorities for squamous cell oesophageal cancer in Africa: a review of setting-specific exposures to known and putative risk factors. Int j Cancer. 2016;140(2):259–271.
36. Huang S-H, Wu I-C, Wu D-C, et al. Occupational risks of esophageal cancer in Taiwanese men. Kaohsiung J Med Sci. 2012;28(12):654–659. doi:10.1016/j.kjms.2012.04.034
37. Hong SJ, Kim TJ, Nam KB, et al. New TNM staging system for esophageal cancer: what chest radiologists need to know. RadioGraphics. 2014;34(6):1722–1740. doi:10.1148/rg.346130079
38. Schlansky B, Dimarino AJ
39. Ahmed M. Addis Ababa University College of Health Science School Public Health; 2018:57.
40. Rastgar Jazii F, editor. Esophageal cancer - cell and molecular biology, biomarkers, nutrition and treatment [internet]. InTech; 2012 [
41. Jackson L, Evers BM. Chronic inflammation and pathogenesis of gi and pancreatic cancers. In: Dalgleish AG, Haefner B, editors. The Link Between Inflammation and Cancer [Internet]. Boston, MA: Springer US; 2006:39–65.
42. Mustafa SA, Banday SZ, Bhat MA, Patigaroo AR, Mir AW, Bhau KS. Clinico-epidemiological profile of esophageal cancer in Kashmir. Age. 2016;3(11):6.
43. Etefa Y, Dibaba K. Bureau of finance and economic development – regional data and information core process. Physical and socio-economic profile of Arsi zone and districts. Finfinne; January 2011:496.
44. CSA, Federal democratic republic of Ethiopia. Central statistical agency: population projection of Ethiopia for all regions at woreda level from 2014–2017. Ethiopia: Central Statistical Agency; 2013:118.
45. Kollarova H, Machova L, Horakova D, Janoutova G, Janout V. Epidemiology of esophageal cancer - an overview article. Biomed Pap. 2007;151(1):17–28. doi:10.5507/bp.2007.003
46. Lamine DM. Esophageal and Gastric Cancers in Sub-Saharan Africa, Epidemiological and Clinical Review. J Gastrointest Dig Syst. 2011. doi:10.4172/2161-069X.S6-007.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
