Back to Journals » Therapeutics and Clinical Risk Management » Volume 14
Clinical validation of the Cervista® high-risk human papillomavirus test in Chinese women from Fujian province: a cross-sectional study
Authors Mao X , Ruan G , Dong B, Chen L, Xu S, Lin F, Sun P
Received 6 July 2018
Accepted for publication 17 October 2018
Published 16 November 2018 Volume 2018:14 Pages 2243—2253
DOI https://doi.org/10.2147/TCRM.S179334
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Deyun Wang
Xiaodan Mao,1 Guanyu Ruan,1 Binhua Dong,1 Lihua Chen,1 Shuxia Xu,2 Fen Lin,1 Pengming Sun1,3
1Laboratory of Gynecologic Oncology, Fujian Provincial Maternity and Children’s Hospital, Affiliated Hospital of Fujian Medical University, Fuzhou, Fujian, China; 2Department of Pathology, Fujian Provincial Maternity and Children’s Hospital, Affiliated Hospital of Fujian Medical University, Fuzhou, Fujian, China; 3Department of Gynecology, Fujian Provincial Maternity and Children’s Hospital, Affiliated Hospital of Fujian Medical University, Fuzhou, Fujian, China
Purpose: To estimate the high-risk human papillomavirus (HR-HPV) prevalence in a hospital-based population using the Cervista® and to determine the clinical value and significance of Cervista for cervical cancer screening in Fujian Province, China.
Patients and methods: In a hospital-based population, a total of 10,771 women from the Fujian Province were screened for cervical cancer and precancerous lesions using the thinprep cytologic test (TCT) and/or the Cervista. Women with HR-HPV infection and/or abnormal TCT were referred for colposcopy and biopsy. Pathological diagnosis was used as the gold standard.
Results: The overall HR-HPV prevalence was 16.57%. Among 10,229 cases, 976 had abnormal cytology results, of which, the HR-HPV positivity rate was 60.35% in this opportunistic screening population. The most common HR-HPV infection style was a simple infection. The most common species was A9 which was also the most prevalent species in all age. The women with CIN2+ (high-grade squamous intraepithelial lesion [HSIL]), especially cancer, were mostly concentrated in the age from 51 to 60 years old. The peak of CIN1 (low-grade squamous intraepithelial lesion, LSIL) prevalence was in the women aged 31–40. When using CIN1+, CIN2+ and CIN3+ as observed endpoints, the sensitivities were 86.07%, 92.73%, and 93.30% and negative likelihood ratio (NPV) were 99.15%, 99.75% and 99.83%, respectively. Cervista and TCT co-testing achieved the highest sensitivity and the lowest NLR.
Conclusion: The Cervista could be easily introduced in clinical practice in combination with TCT for cervical cancer screening in China. Patients with species A9 infection require a more actively clinical intervention.
Keywords: high-risk human papillomavirus, Cervista®, cytology, pathological diagnosis, cervical cancer
Introduction
Cervical cancer is the third most frequent cancer among women globally, especially in developing countries. It is estimated that there were 528,000 newly diagnosed cases and 265,653 deaths in 2012 worldwide.1 In China, the age-standardized incidence rate (ASIR) and mortality rate (ASMR) of cervical cancer were estimated at 10.3 and 2.6 per 100,000 women, respectively, in 2013; these rates are higher than those found in other developed countries.2 Cervical cancer has become one of the major health hazards for women. Fujian Province is on the southern coast of China, and the burden of cervical cancer is heavy there. Despite the successful implementation of cytopathologic screening programs, Chen et al estimate that 98,900 women will be diagnosed with cervical cancer, and 30,500 women died from the disease in China during 2015.3
In the beginning, HPV was used to triage abnormal cytology.4 Subsequently, in 2011, the American Cancer Society (ACS), the American Society for Colposcopy and Cervical Pathology (ASCCP) and the American Society for Clinical Pathology (ASCP) stated that in most clinical settings, women aged 30–65 years should be screened with co-testing.5 Recently, the Society of Gynecologic Oncology (SGO)/ASCCP guidelines propose to use HR-HPV testing alone as a primary screening way, which also recommend to use genotyping for HPV-16 and -18 to triage HR-HPV positive women.6 The benefits of HPV testing in primary cervical cancer screening have been demonstrated in several randomized controlled trials.7,8 A plethora of evidence indicates that high-risk human papillomaviruses (HR-HPVs) are important factors in cervical cancer.9,10 At present, the detection methods for HPV include Hybrid Capture 2 (HC2, Qiagen, Gaithersburg, MD, USA), Cervista® (Hologic, Bedford, MA, USA), Aptima (Hologic), Cobas (Roche, Pleasanton, CA, USA) and others.11 Early in 2009, HPV types were classified categorically as carcinogenic (Group 1), probably carcinogenic (Group 2A), possibly carcinogenic (Group 2B), not classifiable (Group 3), or probably not carcinogenic (Group 4) by the International Agency for Research on Cancer (IARC) Monograph Working Group. Group 1 contained 13 HPV types (type 51, 56, 66, 18, 39, 45, 59, 16, 31, 33, 35, 52 and 58) and Group 2A included 68 HPV types.12 In March 2009, the Cervista HR-HPV assay, which includes three species of HR-HPV (14 HR-HPV types) that were all involved in Group 1 and Group 2A carcinogens, became the second HPV assay approved by the FDA as a triage test for women with atypical squamous cells of undetermined significance (ASC-US) and as an adjunctive test with cervical cytology for routine screening in women aged 30 years or older. This test was also approved in China by the China Food and Drug Administration (CFDA) at the end of 2011 and was clinically available in 2012. There is limited evidence in the literature on the clinical significance of Cervista, especially on its use in China. The Cervista HR-HPV test was a qualitative test for the detection of DNA from 14 HR-HPV types that were used in China for 5 years. We then presented one result regarding Cervista from Fujian Province Cervical Lesion Screening Cohorts (FCLSCs), involving several cervical screening cohorts that included more than 140,000 hospital-based and community-based patients who were tested by multiple HPV detection assays in Fujian Provincial Maternity and Children’s Health Hospital.
The purpose of this study was to estimate the HR-HPV prevalence within a hospital-based population using the Cervista high-risk human papillomavirus (HR-HPV) assay and to evaluate the clinical performance characteristics, including pathological diagnosis in different age stratification, sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of the Cervista HR-HPV test for the detection of CIN2 or worse (CIN2+), and CIN3 or worse (CIN3+) cervical lesions in women in Fujian Province, China.
Patients and methods
Study population
All specimens were collected using plastic cervical swabs from women visiting Fujian Provincial Maternity and Children’s Health Hospital. The study was approved by the Ethics Committee of Fujian Provincial Maternity and Children’s Hospital, Affiliated hospital of Fujian Medical University. All the participants were written informed consent, and that this study was conducted in accordance with the Declaration of Helsinki. The purpose was to estimate the overall HPV prevalence, species, the extent of multiple infections, and clinical significance in the detection of CIN and cervical invasive cancer. The population eligible for this study included 10,771 women, a total of 1,023 were excluded due to pregnancy (n=35), age under 21 (n=32), miss or invalid cytology test (n=395), history of histological diagnosis and treatment of CIN (n=51), lack of consistent follow-up with Cervista or other cytology test (n=29) and miss pathological results or reject biopsy (n=481). The women received HPV screening by gynecological practitioners between March 2012 and December 2016. The population consisted of hospital staff, policewomen, teachers, workers, civil servants, and retirees. The participants were required to fulfill the following criteria: 1) sexually active women aged 21 years or older, 2) no previous histological diagnosis and treatment of gynecological diseases, 3) willingness to undergo HPV testing. All patients provided informed consent.
Cervical specimen collection
Cervical cells were obtained from the cervix of all the women. Ecto- and endocervical specimens were collected by Cervex broom in two separate vials of PreservCyt® Liquid (Hologic). Subsequently, each sample was processed for cytology and HR-HPV assays, respectively.
ThinPrep liquid-based cytology
A slide for the cytologic study was made. The cervical cytologic examination was performed using the automated imaging system (Hologic, Inc., San Diego, CA, USA) and was reviewed by two experienced cytotechnologists and cytopathologists. The results were reported following the Bethesda 2001 system.13 Samples were classified as: negative for intraepithelial lesion or malignancy (NILM), atypical squamous cells of undetermined significance (ASC-US), low-grade squamous intraepithelial lesion (LSIL), atypical squamous cells, not possible to exclude high-grade squamous intraepithelial lesion (ASC-H), high-grade squamous intraepithelial lesion (HSIL), squamous cervical cancer (SCC), atypical glandular cells (AGC), and adenocarcinoma in situ (AIS). If the diagnosis differed between two cytopathologists, the cervical samples were reviewed again and a consensus diagnosis was obtained.
Cervista HR-HPV test
This is a qualitative test detecting 14 HR-HPV types. The assay uses three separate oligonucleotide mixtures: mix 1 (species A5/A6) contains probes for HPV 51, 56 and 66; mix 2 (species A7) contains probes for HPV 18, 39, 45, 59 and 68, and mix 3 (species A9) contains probes for HPV 16, 31, 33, 35, 52 and 58. In these three mixes, oligonucleotides for the human histone 2 gene (HIST2H2BE) are also present as an internal control for the presence of sufficient genomic DNA. Then, Invader Chemistry (Hologic, Inc.) was applied, consisting of two simultaneous isothermal and signal-amplification reactions to detect specific nucleic acid sequences.14
Histology
The women who were HPV-positive and/or had abnormal thinPrep liquid-based cytology (with a grade higher than ASC-US) were referred for colposcopy and biopsy. Specimens were collected from these women by punch biopsy or loop electrosurgical excision procedure cone biopsy (LEEP). Specimens were fixed in 10% formalin and were routinely processed for paraffin embedding. Then, 4 μm thick histological sections were cut and stained with hematoxylin and eosin using standard methods. Then, cervical biopsy specimens were histologically examined and classified according to the cervical intraepithelial neoplasia system. All samples with a primary histology result of CIN2+ were reviewed by an independent expert. In case of a discrepant review reading, a second histology review was performed. If two out of three diagnoses were identical, the result was considered final.
Statistical methods
The performance characteristics of the screening tests were evaluated by calculating sensitivity, specificity, PPV, NPV, PLR, and NLR according to the standard definitions for CIN1, CIN2, CIN3, and invasive cervical cancer. All confidence intervals (CIs) were exact binomial confidence intervals. In addition, an analysis exploring test characteristics at different cut points for Cervista was undertaken by Fisher’s exact test. These results were then plotted. All data analyses were performed using SPSS 20.0 (IBM, Chicago, IL, USA).
Results
Prevalence of HR-HPV infection
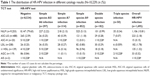
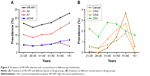
In this study, 10,771 women underwent the Cervista HR-HPV test. A flowchart describing the selection of the study cohort with inclusion/exclusion criteria can be found in Figure 1. The overall HR-HPV infection rate in this population was 16.57% (1,695/10,229, CI: 15.85%–17.31%) when excluding 1,023 cases who did not conform to the standard criteria or displayed invalid or missing information. The positivity of simple species was 14.30% (1,463/10,229), including 2.90% (297/10,229) of species A5/A6, 3.07% (314/10,229) of species A7 and 8.33% (852/10,229) of species A9. The positivity of multiple species was 2.27% (232/10,624), including double species positivity of 1.78% (182/10,229) and triple species positivity of 0.49% (50/10,229) (Figure 2A). The HR-HPV positive rate was 11.95% (1,106/9,253) in women with NILM and 60.35% (589/976) in women with abnormal cytological results. The HR-HPV prevalence was 45.69% (223/488) in patients diagnosed with ASC-US, 75% (15/20) in patients with ASC-H, 87.50% (182/208) in patients with LSIL, 97.12% (135/139) in patients with ≥ HSIL, and 27.73% (33/119) in patients with AGC. In the HR-HPV infected population, species A9 was detected in 1,064 cases, accounting for 62.78% (1,064/1,695) of all positive specimens (including mixed infection). (Table 1).
Prevalence of cytological abnormality
The patients with abnormal cytology and/or HR-HPV infection were referred for colposcopy and biopsy. The prevalence of cytological results with diagnosis of ASC-US or worse was 9.54% (976/10,229, 95% CI: 8.98%–10.13%), including 45.90% ASC-US (448/976), 2.05% ASC-H (20/976), 21.31% LSIL (208/976), 14.24% ≥ HSIL (139/976), 12.19% AGC (119/976). In this study, there was 23.57% (70/297) abnormal cytology in the simple species A5/A6 positive, 30.57% (96/314) in the simple species A7 positive, 38.38% (327/852) in the simple species A9 positive. Simple A9 species was the most prevalent in the population with different cytology. The simple species A9 infection was the most prevalent with a rate of 47.47% (525/1,106) in patients with NILM, 54.26% (121/223) in patients with ASC-US, 80.00% (12/15) in patients with ASC-H, 45.05% (82/182) in patients with LSIL, 71.11% (96/135) in patients with ≥ HSIL and 45.45% (15/33) in patients with AGC, respectively. (Table 1).
Triage of HR-HPV in the patients with a different pathological diagnosis
In general, 8,147 patients were negative for both cytology and HR-HPV infection while 1,601 cases with HR-HPV positive and/or abnormal cytology were referred for colposcopy and biopsy whose pathological results was used as a final diagnosis standard. HR-HPV infection rate was 9.06% (837/9,242) in patients with cervicitis or NILM, 77.63% (177/228) in patients with CIN1, 91.25% (73/80) in patients with CIN2, 91.41% (117/128) in patients with CIN3 and 97.12% (68/70) in patients with cancer, respectively. According to the pathological results, simple species A9 infection rates in patients with CIN1, CIN2, CIN3, and cancer were 36.40% (83/228), 62.50% (50/80), 66.41% (85/128) and 55.71% (39/70), respectively. (Figure 2B–F). Overall, the detection rate of CIN2+ and CIN3+ lesions in the HPV-positive species was significantly higher than that of the HR-HPV-negative species (CIN2+=7,290.07, P<0.001; CIN3+=2,528.13, P<0.001). The detection rate of CIN2+ or CIN3+ lesions in the HR-HPV-positive species was significantly higher than that of the HR-HPV-negative species in patients with cervicitis or NILM, ASC-US and AGC. However, the detection rate of CIN2+ lesions in the HR-HPV-positive species was significantly higher than that of the HR-HPV-negative species in the patients with LSIL, however, the detection rate of CIN3+ lesions in HR-HPV-positive species and HR-HPV-negative species showed no significant difference. Moreover, the detection rates of CIN2+ or CIN3+ lesions in the HR-HPV-positive species and HR-HPV-negative species in the patients with ASC-H and ≥ HISL were not significantly different (Table 2).
Age-specific proportions for HR-HPV infection and high-grade cervical lesion
The HR-HPV infection rates in different age groups were 16.93% (21–25 years), 14.55% (26–30 years), 16.18% (31–40 years), 17.33% (41–50 years), 20.23% (51–60 years) and 22.80% (>61 years), respectively. The trend of A9 species and A5/A6 species infection rates was similar to the HR-HPV infection rate. But A7 species infection rate significantly dropped in the >61 years old group. Obviously, the prevalence of A9 species was the highest in the HR-HPV infection (Figure 3A). According to the pathological diagnosis, the women with CIN2+ (HSIL) were mostly concentrated in the age from 51 to 60 years old. Notably, the prevalence of cervical cancer was the highest in the patients aged 51–60. The peak of CIN1 (LSIL) prevalence was in the women aged 31–40 (Figure 3B).
Diagnostic efficiency of Cervista HR-HPV, thinprep cytologic test (TCT), and co-testing (TCT combined with Cervista HR-HPV) in cervical cancer
The sensitivity, specificity, PPV, NPV, PLR, and NLR were analyzed for different screening methods by HR-HPV, TCT, or co-testing (TCT+ HR-HPV) when used to predict CIN1+, CIN2+, and CIN3+ as critical endpoints (Table 3). The results show that the sensitivity of co-testing and HR-HPV was higher than that of TCT, especially in CIN2+ and CIN3+. With the increase in cervical lesions, the sensitivity of the HPV, TCT, and co-testing rose, but the specificity was reduced. The sensitivity and NPV were the highest and NLR was the lowest in the method of HR-HPV+ TCT sequential screening. Moreover, as listed in Figure 4, the co-test as primary screening could detect 239 cases with CIN2+ at the baseline, 35 cases in the 1-year recall, and five cases in the follow-up. As for CIN3+, 174 cases were detected at the baseline, 23 cases in the 1-year recall, and two cases in the follow-up.
Discussion
A retrospective evaluation of cervical screening data from 56,501 specimens subjected to both cytologic examination and HR-HPV DNA testing suggested the rate of abnormal cytology with ASC-US or worse was 11.7% and the HR-HPV infection rate was 15.9% by Cervista HR-HPV assay in USA.14 In China, there are not sufficient data on the national infection rates of HR-HPV. Based on opportunistic screenings in a population of 19,018 women in Beijing, the rate of abnormal cytology was 6.48% and the rate of HPV infection was 19.1% by high-risk HPV genotyping real-time PCR kit (Shanghai ZJ Bio-Tech Co., Ltd., Shanghai, China).15 A multicenter study including 30,207 women from 17 population-based studies throughout China reported an HR-HPV infection rate of 17.7% and age-standardized HR-HPV prevalence was 16.8% by HC2 (Qiagen) in 2012.16 In our study, based on a local center hospital population, the HR-HPV overall infection rate was 16.57% when detected by Cervista, and the rate of abnormal cervical cytology was 9.54%, consistent with the data from single-center or multicenter studies in China.
According to the IARC Monograph Working Group, the HR-HPV gene types of species A7 and A9 were included in Group 1 and Group 2A.12 Most studies indicated women who were HR-HPV negative were at lower risk of CIN3, cancer, and cancer death over a 10-year period.17,18 There is profound importance in detecting the species A7 and A9 in China, in which cervical cancer screening has not yet been universally adopted. In this study, the most common style of HR-HPV infection was simple HR-HPV species, among which the most common species was A9 followed by A7. Moreover, women with abnormal cytology were mostly infected with species A9 or A7, especially in ≥ HSIL. Previously, our team reported the most common HR-HPV types were HPV-16, -52, -58, -18, -53, -33, and -51, ranked from highest to lowest, and HPV-16, -18, -58, -59, and -33 were the top five prevalent genotypes in cervical cancer; however, HPV-16, -18, -59, -45, and -33 were the top five highest risk factors for cancer in Fujian Province.19 The risk of species A9 has been confirmed in many studies and Cervista A9 even replaced the full Cervista assay as the primary screening modality.20 Our recent research also showed Cervista A9 was a good primary screening strategy.21 This study also suggested that simple species A9 infection was overwhelming in women with CIN2, CIN3 and cancer, and all the infection rates were higher than 50%. Therefore, species A9 could be used to triage patients who were HPV-positive but who without substantial abnormal cytology. The benefits are not only that patients could obtain better precise screening and avoid overtreatment but also that the psychological burden regarding cervical cancer could be reduced sharply.
When squamous intraepithelial lesions of cervix occurred, the detection of CIN2+ by TCT was 87.46% (244/279); in particular, the detection rate of CIN2+ was 10.71% (44/411) in patients with ASC-US, 55.56% (10/18) in patients with ASC-H, 24.73% (46/186) in patients with LSIL and 95.52% (128/134) in patients with ≥ HSIL. A similar trend was observed in the detection of CIN3+ by TCT. While the detection of CIN2+ was only 12.17% (14/115) in patients with AGC. Due to the only two patients with AIS detected by TCT, we did not calculate the percentage (Table 2). Thus, the diagnostic specificity of cytology aimed at high-grade squamous intraepithelial lesions of the cervix showed significant advantage but not in AGC lesions. Several studies suggested that abnormal cytological findings in the normal population can lead to an erroneous diagnosis of ASC-US, AGC, or even LSIL.11,22–24 Therefore, co-testing showed particularly important in cervical cancer screen. Then, how effective was the clinical application of the Cervista test in China, especially in Fujian province?
As seen in Table 2, the detection rate of CIN2+ by HR-HPV was 92.83 (259/279); in particular, the detection rate of CIN2+ was 88.64% (39/44) in patients with ASC-US, 90.00% (9/10) in patients with ASC-H, 95.65% (44/46) in patients with LSIL, and 96.88% (124/128) in patients with ≥ HSIL in the squamous intraepithelial lesions of the cervix. Moreover, a similar trend was revealed for the detection of CIN3+ by HR-HPV. Nevertheless, the HR-HPV-positive women had a higher incidence of CIN2+ and CIN3+ cervical lesions than the HR-HPV-negative in the patients with NILM, ASC-US when the squamous intraepithelial lesions of the cervix happened. It was worth noting that the HR-HPV-positive women had a higher incidence of CIN2+ but not CIN3+ cervical lesions than the HR-HPV-negative in the patients with LSIL. However, the incidence of CIN2+ and CIN3+ cervical lesions between HR-HPV-positive and HR-HPV-negative women showed no significant difference when their cytology diagnoses were ≥ HSIL. This evidence reconfirmed that HR-HPV showed no large advantage when triaging high-grade cervical lesions and cytology could triage patients directly. This observation has also been confirmed in many other studies.25–28
Similarly, the detection rate of CIN2+ and CIN3+ was 85.71% (12/14) and 78.57% (11/14), respectively, in patients with AGC. The HR-HPV-positive women had a higher incidence of CIN2+ and CIN3+ cervical lesions than the HR-HPV-negative in the patients with AGC. Therefore, HR-HPV showed advantages compared with TCT when screening AGC of the cervix. On one hand, HR-HPV triaged patients with NILM or ASC effectively. On the other hand, patients with CIN2+ and CIN3+ cervical lesions when their cytology diagnosis was AGC could be distinguished by HR-HPV. Liu et al29 collected a total of 169 paraffin-embedded specimens of cervical adenocarcinoma from nine hospitals in seven regions across China. They detected 14 types of HR-HPV in whole tissue sections (WTSs). HPV16 was the most common type, and the second most common were HPV18 and HPV52. The HPV positive rate was 50.8% and 66.7% for the simple infection and multiple infections, respectively, after laser capture microdissection (LCM). That was a better proof that HR-HPV could reliably identify AGC and cervical adenocarcinoma.
After age stratification, there were two peaks of HR-HPV prevalence in the women who were 21–25 years and >60 years, respectively. The result was consistent with the data of cervical cancer screening in Zhejiang Province.30 While the prevalence of A7 and A5/A6 infection was similar. A9 species infection was the most popular. The prevalence of HSIL (CIN2+) was increasing with age. There was a same peak of HSIL (CIN2+) in the women aged 51–60 years, which was consistent with the time-dependent carcinogenesis of HPV. However, the peak of LSIL (CIN1) was in the population aged 31–40 years. But the prevalence of LSIL (CIN1) showed a downward trend with age after 40 years. Thereout, we need to pay more attention to the elderly women with A9 species infection in clinical.
Our study showed that the Cervista HR-HPV assay and cervical tissue pathology were positively correlated, indicating that the Cervista technology can accurately detect HR-HPV infection in cervical lesions. In particular, the species A9 and A7 HR-HPV infection would be more detected. The success of HR-HPV testing in clinical practice is largely dependent on its high sensitivity, NPV, and lowest NLR. Therefore, false-negative results should be particularly worrying. A combination of HPV detection and cytology can improve the sensitivity and the NPV of the screening for cervical cancer and CIN. In this study, the use of TCT cytology combined with the Cervista HR-HPV test was evaluated. When the detection endpoint was CIN1+, CIN2+ and CIN3+ lesions, the PPV and specificity of both tests combined were higher than either test alone. Boers et al31 claimed that both the clinical sensitivity and specificity of the Cervista HPV HR test for high-risk human papillomavirus (HPV) detection were not inferior to those of the Hybrid Capture 2 (HC2) test. Moreover, we missed 14.34% (40/279) women with CIN2+ and 12.56% (25/199) women with CIN3+ in the first round co-testing. When 1-year recall, we missed 1.79% (5/279) women with CIN2+ and 1.01% (2/199) women with CIN3+. Thus, Cervista could be used in co-testing to screen cervical lesion.
There are limited data in the literature regarding the clinical use of Cervista in China. Our results showed that the Cervista HR-HPV test was sensitive, specificity, and reliable screening method. It not only could screen out the cervical lesion of squamous epithelium cell but also of gland cell. Gynecologists should take active clinical intervention when the patient infected with species A9.
Conclusion
The Cervista could be easily introduced in clinical practice in combination with TCT for cervical cancer screening in China. Patients with species A9 infection require a more actively clinical intervention.
Acknowledgments
This work was supported by grants from the Fujian Provincial Health and Family Planning Commission Innovation Project (grant no. 2009-CXB-33) and the Natural Science Foundation of Fujian Province (grant no. 2017J01232).
Author contributions
Conceptualization: P Sun, X Mao. Methodology: P Sun, X Mao, G Ruan. Software: X Mao, B Dong, L Che.n Validation: P Sun, X Mao, G Ruan, S X.u Formal analysis: P Sun, X Mao, L Chen. Data curation: X Mao, G Ruan, B Dong, S Xu, F Lin. Writing – original draft: X Mao. Writing – review and editing: P Sun. Funding acquisition: P Sun, B Dong. All authors contributed toward data analysis, drafting and revising the paper, gave final approval of the version to be published and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136(5):e359–e386. | ||
Jiang X, Tang H, Chen T. Epidemiology of gynecologic cancers in China. J Gynecol Oncol. 2018;29(1):e7. | ||
Chen W, Zheng R, Baade PD, et al. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66(2):115–132. | ||
US Preventive Services Task Force, Curry SJ, Krist AH, et al. Screening for cervical cancer: US Preventive Services Task Force Recommendation Statement. JAMA. 2018;320(7):674–686. | ||
Chelmow D. Cervical cancer screening and prevention. Am Coll Obstet Gynecol. 2016;128:923–925. | ||
Saslow D, Solomon D, Lawson HW, et al. American Cancer Society, American Society for Colposcopy and Cervical Pathology, and American Society for Clinical Pathology screening guidelines for the prevention and early detection of cervical cancer. CA Cancer J Clin. 2012;62(3):147–172. | ||
Ronco G, Dillner J, Elfström KM, et al. Efficacy of HPV-based screening for prevention of invasive cervical cancer: follow-up of four European randomised controlled trials. Lancet. 2014;383(9916):524–532. | ||
Meijer CJ, Berkhof J, Castle PE, et al. Guidelines for human papillomavirus DNA test requirements for primary cervical cancer screening in women 30 years and older. Int J Cancer. 2009;124(3):516–520. | ||
Walboomers JM, Jacobs MV, Manos MM, et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol. 1999;189(1):12–19. | ||
Meijer CJ, Snijders PJ, Castle PE. Clinical utility of HPV genotyping. Gynecol Oncol. 2006;103(1):12–17. | ||
Guan P, Howell-Jones R, Li N, et al. Human papillomavirus types in 115,789 HPV-positive women: a meta-analysis from cervical infection to cancer. Int J Cancer. 2012;131(10):2349–2359. | ||
Bouvard V, Baan R, Straif K, et al. A review of human carcinogens–Part B: biological agents. Lancet Oncol. 2009;10(4):321–322. | ||
Diane Solomon DD, Kurman R, Moriarty A. The 2001 Bethesda System. JAMA. 2002;287:2114–2119. | ||
Youens KE, Hosler GA, Washington PJ, Jenevein EP, Murphy KM. Clinical experience with the Cervista HPV HR assay: correlation of cytology and HPV status from 56,501 specimens. J Mol Diagn. 2011;13(2):160–166. | ||
Li Y, Huang K, Ji PL, Song L, Liu HT, Pl J. Cervical infection of oncogenic human papillomavirus (HPV) types in Beijing, China. Biomed Environ Sci. 2016;29(10):734–741. | ||
Zhao FH, Lewkowitz AK, Hu SY, et al. Prevalence of human papillomavirus and cervical intraepithelial neoplasia in China: a pooled analysis of 17 population-based studies. Int J Cancer. 2012;131(12):2929–2938. | ||
Mulindi Mwanahamuntu HH, Parham GP. HPV screening for cervical cancer in rural India. N Engl J Med. 2009;361(3):305–306. | ||
Schiffman M, Wacholder S, Mark Schiffman SW. From India to the world-a better way to prevent cervical cancer. N Engl J Med. 2009;360(14):1453–1455. | ||
Sun P, Song Y, Ruan G, et al. Clinical validation of the PCR-reverse dot blot human papillomavirus genotyping test in cervical lesions from Chinese women in the Fujian province: a hospital-based population study. J Gynecol Oncol. 2017;28(5):e50. | ||
Zhao J, du H, Belinson JL, et al. Evaluation of The Cervista HPV A9 group in screening patients for cervical cancer. J Med Screen. 2016;23(1):38–43. | ||
Ruan G, Song Y, Dong B, et al. Cervical cancer screening using the Cervista high-risk human papillomavirus test: opportunistic screening of a hospital-based population in Fujian province, China. Cancer Manag Res. 2018;10:3227–3235. | ||
Kennedy AW, Salmieri SS, Wirth SL, Biscotti CV, Tuason LJ, Travarca MJ. Results of the clinical evaluation of atypical glandular cells of undetermined significance (AGCUS) detected on cervical cytology screening. Gynecol Oncol. 1996;63(1):14–18. | ||
Stoler MH, Schiffman M; Atypical Squamous Cells of Undetermined Significance-Low-grade Squamous Intraepithelial Lesion Triage Study (ALTS) Group. Interobserver reproducibility of cervical cytologic and histologic interpretations: realistic estimates from the ASCUS-LSIL Triage Study. JAMA. 2001;285(11):1500–1505. | ||
Scheungraber C, Kleekamp N, Schneider A. Management of low-grade squamous intraepithelial lesions of the uterine cervix. Br J Cancer. 2004;90(5):975–978. | ||
Tracht JM, Davis AD, Fasciano DN, Eltoum IA. Discrepant HPV/cytology co-testing results: Are there differences between cytology-negative versus HPV-negative cervical intraepithelial neoplasia? Cancer Cytopathol. 2017;125(10):795–805. | ||
Sideri M, Igidbashian S, Boveri S, et al. Age distribution of HPV genotypes in cervical intraepithelial neoplasia. Gynecol Oncol. 2011;121(3):510–513. | ||
Li ZM, Zeng LQ, Peng XH, et al. Analysis of clinical and pathological characteristics of high-risk HPV-negative carcinoma of the uterine cervix. Zhonghua Fu Chan Ke Za Zhi. 2016;51(9):683–687. | ||
Liu HF, Liu M, Xu YL, Yl X. Analysis of high-risk HPV infection and cervical cytologic screening in HIV positive women. Zhonghua Fu Chan Ke Za Zhi. 2016;51(10):734–738. | ||
Liu B, Wu ZN, Liu XY, et al. Distribution of human papillomavirus (HPV) among HPV positive cervical adenocarcinoma cases detected by laser capture microdissection (LCM). Zhonghua Zhong Liu Za Zhi. 2016;38(4):277–282. | ||
Wu Q, Zhao X, Fu Y, et al. A cross-sectional study on HPV testing with type 16/18 genotyping for cervical cancer screening in 11,064 Chinese women. Cancer Med. 2017;6(5):1091–1101. | ||
Boers A, Slagter-Menkema L, van Hemel BM, et al. Comparing the Cervista HPV HR test and Hybrid Capture 2 assay in a Dutch screening population: improved specificity of the Cervista HPV HR test by changing the cut-off. PLoS One. 2014;9(7):e101930. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.