Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 14
Clinical Significance of Bronchodilator Responsiveness Evaluated by Forced Vital Capacity in COPD: SPIROMICS Cohort Analysis
Authors Barjaktarevic IZ , Buhr RG , Wang X, Hu S, Couper D , Anderson W, Kanner RE , Paine III R, Bhatt SP , Bhakta NR , Arjomandi M , Kaner RJ , Pirozzi CS , Curtis JL , O'Neal WK, Woodruff PG, Han MK, Martinez FJ , Hansel N, Wells JM, Ortega VE, Hoffman EA , Doerschuk CM, Kim V , Dransfield MT, Drummond MB , Bowler R, Criner G, Christenson SA, Ronish B, Peters SP , Krishnan JA , Tashkin DP, Cooper CB
Received 23 June 2019
Accepted for publication 31 October 2019
Published 20 December 2019 Volume 2019:14 Pages 2927—2938
DOI https://doi.org/10.2147/COPD.S220164
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Igor Z Barjaktarevic, 1 Russell G Buhr, 1, 2 Xiaoyan Wang, 3 Scott Hu, 1 David Couper, 4 Wayne Anderson, 4 Richard E Kanner, 5 Robert Paine III, 5 Surya P Bhatt, 6 Nirav R Bhakta, 7 Mehrdad Arjomandi, 7 Robert J Kaner, 8 Cheryl S Pirozzi, 5 Jeffrey L Curtis, 9, 10 Wanda K O’Neal, 4 Prescott G Woodruff, 7 MeiLan K Han, 9 Fernando J Martinez, 8 Nadia Hansel, 11 James Michael Wells, 6 Victor E Ortega, 12 Eric A Hoffman, 13 Claire M Doerschuk, 4 Victor Kim, 14 Mark T Dransfield, 6 M Bradley Drummond, 4 Russell Bowler, 15 Gerard Criner, 14 Stephanie A Christenson, 7 Bonnie Ronish, 5 Stephen P Peters, 12 Jerry A Krishnan, 16 Donald P Tashkin, 1 Christopher B Cooper 1 On behalf of the NHLBI SubPopulations and InteRmediate Outcome Measures In COPD Study (SPIROMICS)
1Department of Medicine, University of California, Los Angeles, Los Angeles, CA, USA; 2Department of Health Policy and Management, Fielding School of Public Health, University of California, Los Angeles, Los Angeles, CA, USA; 3Department of General Internal Medicine and Health Services Research, University of California, Los Angeles, Los Angeles, CA, USA; 4Department of Medicine, University of North Carolina, Chapel Hill, NC, USA; 5Department of Medicine, University of Utah, Salt Lake City, UT, USA; 6Division of Pulmonary, Allergy and Critical Care Medicine, University of Alabama at Birmingham, Birmingham, AL, USA; 7Department of Medicine, University of California, San Francisco, San Francisco, CA, USA; 8Department of Medicine, Weill Cornell Weill Cornell Medical Center, New York, NY, USA; 9Department of Medicine, University of Michigan, Ann Arbor, MI, USA; 10Medicine Service, VA Ann Arbor Healthcare System, Ann Arbor, MI, USA; 11Department of Medicine, John Hopkins University, Baltimore, MD, USA; 12Department of Medicine, Wake Forest School of Medicine, Winston-Salem, NC, USA; 13Department of Medicine, University of Iowa, Iowa City, IA, USA; 14Department of Thoracic Medicine and Surgery, Lewis Katz School of Medicine at Temple University, Philadelphia, PA, USA; 15Department of Medicine, National Jewish Health Systems, Denver, CO, USA; 16Department of Medicine, University of Illinois at Chicago, Chicago, IL, USA
Correspondence: Christopher B Cooper
Departments of Medicine and Physiology, David Geffen School of Medicine, University of California Los Angeles, 10833 Le Conte Avenue, 37-131 CHS, Los Angeles, CA 90095, USA
Email [email protected]
Objective: Bronchodilator responsiveness (BDR) is prevalent in COPD, but its clinical implications remain unclear. We explored the significance of BDR, defined by post-bronchodilator change in FEV 1 (BDRFEV1) as a measure reflecting the change in flow and in FVC (BDRFVC) reflecting the change in volume.
Methods: We analyzed 2974 participants from a multicenter observational study designed to identify varying COPD phenotypes (SPIROMICS). We evaluated the association of BDR with baseline clinical characteristics, rate of prospective exacerbations and mortality using negative binomial regression and Cox proportional hazards models.
Results: A majority of COPD participants exhibited BDR (52.7%). BDRFEV1 occurred more often in earlier stages of COPD, while BDRFVC occurred more frequently in more advanced disease. When defined by increases in either FEV 1 or FVC, BDR was associated with a self-reported history of asthma, but not with blood eosinophil counts. BDRFVC was more prevalent in subjects with greater emphysema and small airway disease on CT. In a univariate analysis, BDRFVC was associated with increased exacerbations and mortality, although no significance was found in a model adjusted for post-bronchodilator FEV 1.
Conclusion: With advanced airflow obstruction in COPD, BDRFVC is more prevalent in comparison to BDRFEV1 and correlates with the extent of emphysema and degree of small airway disease. Since these associations appear to be related to the impairment of FEV 1, BDRFVC itself does not define a distinct phenotype nor can it be more predictive of outcomes, but it can offer additional insights into the pathophysiologic mechanism in advanced COPD.
Clinical trials registration: ClinicalTrials.gov: NCT01969344T4.
Keywords: bronchodilator responsiveness, inspiratory capacity, FVC, FEV 1, SPIROMICS
Corrigendum for this paper has been published
Introduction
Chronic obstructive pulmonary disease (COPD) is characterized by airflow limitation that persists after bronchodilator (BD) administration and is defined by the ratio of forced expiratory volume in one second (FEV1) to forced vital capacity (FVC) (FEV1/FVC) <0.70.1 Widely accepted guidelines define bronchodilator responsiveness (BDR) by the increase in FEV1 or FVC of ≥200 mL and ≥12% relative to pre-BD values.2,3 BDR is common in COPD patients,4,5 but whether it defines a unique phenotype is incompletely understood. In contrast to BDRFEV1, which represents a flow-based, time-limited response to bronchodilators, BDRFVC evaluates the volumetric response and, together with other spirometry-measured capacities (slow vital capacity [SVC] and inspiratory capacity [IC]), evaluates a BD effect that is neither flow-dependent nor time-limited.6 Studies of the response patterns to BD administration in COPD suggest that reduction in hyperinflation and air trapping, as reflected by increases in lung volumes, leads to improvement in symptoms.6,7 Nevertheless, with conflicting data about the clinical relevance of BDRFVC in the assessment of COPD8–11 and the lack of recommendations about the interpretability of BDR assessed by FVC and FEV1,12 a clear understanding of the clinical relevance of BDR in COPD has been largely missing.
Using data from a large cohort of longitudinally followed individuals, we evaluated the clinical significance of BDR in COPD and its relationship to the frequency of COPD exacerbations, which are associated with increased morbidity and mortality.13,14 We compared flow- and volume-based responsiveness to BD administration and analyzed distinct clinical implications of FEV1BDR and FVCBDR and their association with various outcomes.
Methods
Study Design and Participants
Subpopulations and Intermediate Outcome Measures in COPD (SPIROMICS) is a multi-center observational study designed to identify different COPD phenotypes. SPIROMICS enrolled 2,974 participants, ages 40–80 years into four strata (non-smokers; current and former smokers without airflow obstruction; and current and former smokers with either mild/moderate COPD, or severe/very severe COPD).15 Of these, 1,831 participants had COPD based on GOLD criteria.12 Subjects with a current diagnosis of asthma or pulmonary comorbidities not related to COPD were excluded from participation in the study, although those with a prior history of asthma that was no longer active were eligible. Participants completed a baseline examination that comprised a detailed medical history; blood and sputum biomarker analysis; assessment of dyspnea by modified Medical Research Council (mMRC) scale, of symptoms by COPD assessment test (CAT), and of health status by St. George’s Respiratory Questionnaire (SGRQ); spirometry before and after inhaled BD; and high resolution chest CT scan (HRCT). Enrolled subjects were classified using GOLD guidelines.12,16
Spirometry
Spirometry was performed using a centrally supplied pneumotachograph following current ATS/ERS recommendations and using reference values calculated from the Hankinson equation.3 COPD was defined by a post-BD FEV1/FVC<0.70. Prior to the testing, participants were asked to withhold bronchodilators for at least a period equal to twice the usual dosing frequency. BDR was tested 30 mins after four inhalations each of albuterol sulfate HFA (90 µg/actuation) and ipratropium bromide HFA (17 µg/actuation). We defined BDR as an increase in FEV1, FVC, or IC of ≥12% and ≥200 mL.2
Chest CT Acquisition and Analysis
All SPIROMICS participants underwent HRCT on 64- or 128-slice helical scanners. Images were obtained at suspended full inhalation and on exhalation and data were analyzed by Apollo software (VIDA Diagnostics, Coralville, IA).17 Emphysema scores were derived using percentages of low attenuation area below and including −950 Hounsfield units (HU). Parametric response mapping (PRM), a dynamic image registration technique that links inspiratory and expiratory features of CT lung scans, was used to assess functional small airway disease (fSAD) and emphysema.18 PRM was performed on all CT data automatically using Lung Density Analysis (LDA™) software application (Imbio, LLC, Minneapolis, MN). The adopted nomenclature for these measures for normal lung parenchyma and fSAD is PRMNormal and PRMfSAD, respectively.
Statistical Analysis
Demographic and clinical characteristics were tabulated, using mean and standard deviation for continuous variables, and frequency and percentages for categorical variables. We compared the clinical differences in clinical characteristics between BD responders and BD nonresponders using a two-sample t-test (or Wilcoxon rank sum test, if normality was not met) for continuous variables and a Chi-square test for categorical variables. PRMfSAD scores between BD responders and nonresponders were compared by Wilcoxon rank sum test. To assess BDR repeatability measured by FEV1, FVC, and IC, we calculated percentages of positive, negative, and total agreement, as well as Cohen’s kappa.
We investigated if BDRFVC was associated with exacerbations using univariate and multivariate negative binomial models and tested associations of BDRFVC with 3-year survival by univariate and multivariate Cox proportional hazards models and Kaplan–Meier survival functions. For all multivariate modeling, stepwise model selections were performed to obtain the final parsimonious model. All tests for significance were two-tailed, using P-value less than 0.05 as the threshold for significance. All statistical analyses were conducted using SAS version 9.4 (SAS Institute Inc. 2013).
Ethics Statement
All investigations were conducted according to the principles of the Declaration of Helsinki. Protocols were reviewed and approved by institutional review boards in each participating site (detailed list of all approving ethics committees provided in the Supplemental data). All participants understood the purpose of the study, and all gave written informed consent before any procedures.
Results
Demographic Data
Of 2,974 participants, 202 (6.8%) were healthy never-smokers, 941 (31.6%) were current or former smokers without airflow obstruction, and 1,831 (61.6%) had COPD with one-third of those having severe or very severe disease defined by GOLD spirometric staging (Table 1). Mean smoking history among ever-smokers was 46 pack-years, and current smokers comprised 37% of the overall population.
 |
Table 1 Demographic Data in SPIROMICS Cohort |
Repeatability of BDR Measured by FEV1, FVC, and IC
To assess BDR repeatability of flow-based versus volume-based measurements, we analyzed results of a published substudy of 98 participants who replicated their entire baseline evaluation (including spirometry) 2–6 weeks after their initial visit.19 BDRFVC had greatest repeatability (76.5%, k=0.53), in comparison to BDRFEV1 (72.4%, k=0.43) or BDRIC (64.2%, k=0.27), Supplemental Table 1.
BDR in SPIROMICS Cohort
BDR was observed across all participant groups (Figure 1) and was similar for flow-based (FEV1, 29.0%) and volume-based metrics, including FVC (26.3%) and SVC (26.5%) or IC (32.1%). Among participants without COPD, 7.1% of never-smokers and 13.7% of ever-smokers without obstruction demonstrated BDR defined by either FEV1 or FVC. Among those with BDR, a response was detected more often by BDRFEV1 than by BDRFVC (7.1% vs 2% never smokers; 13% vs 4.5% ever-smokers without obstruction). Comparing BDR for FVC to BDR for SVC and IC, a lower prevalence of BDRFVC was evident in both healthy never-smokers (BDRFVC 2% vs BDRSVC 5.0% and BDRIC 13.4%) and ever-smokers without obstruction (BDRFVC 4.5% vs BDRSVC 11.6% and BDRIC 22.5%), suggesting greater ability of BDRFVC parameter to discriminate between healthy and diseased airways.
 |
Figure 1 Overall BDR defined by different spirometric measures in the SPIROMICS cohort. |
Over half of the subjects with COPD displayed FEV1- or FVC-defined BDR (52.7%) with similar overall frequencies of BDRFEV1 (39.7%) and BDRFVC (40.2%). In contrast to other groups, COPD subjects showed a greater prevalence of BDRFVC than BDRIC or BDRSVC (39.1% and 36.7%, respectively). Accepting categorization of subjects as BD responsive if any of the these four metrics indicated BDR, we found 67.1% of the participants with COPD to be BD responders.
BDR Relates to a Reported History of Asthma but Not to Blood Eosinophil Counts
Although individuals with currently active non-COPD obstructive lung disease were not included in SPIROMICS cohort, participants with COPD had a self-reported previous history of asthma more frequently than healthy nonsmokers or former/current smokers (Table 1). A self-reported history of asthma was significantly more common in participants who were FEV1- or FVC-BD responders (Table 2). Neither BDRFVC nor BDRFEV1 was associated with blood eosinophil counts (BEC), relative to nonresponders (Table 2).
 |
Table 2 Baseline Clinical Characteristics of FVC-BD Responders and FVC-BD Nonresponders |
Volume Responsiveness Increases as COPD Progresses
Mild COPD (spirometric GOLD grade 1) was characterized by greater BDRFEV1 than BDRFVC (35.6% vs 19.2%), a difference that was less marked in GOLD grades 2 and 3 (Figure 2A). In very severe COPD (spirometric GOLD grade 4), BDRFEV1 was infrequent (11.3%). By contrast, BDRFVC prevalence increased with advanced obstruction and was observed most frequently (54.3%) in spirometric GOLD grade 4.
To investigate whether the observed low frequency of BDRFEV1 in very severe disease was simply a consequence of low (<30% predicted) baseline FEV1, we performed sensitivity analyses of BDRFEV1 and BDRFVC by dividing subjects with COPD into four GOLD groups (A through D), defined by either combining spirometric grades with exacerbation frequency and symptoms (GOLD revision 2011), (Figure 2B) or by only exacerbation frequency and symptoms without spirometry (GOLD revision 2019) (Figure 2C). In both classification systems, advanced disease (Group D) was characterized by a greater prevalence of BDRFVC (50.8% and 41.4%, respectively) than BDRFEV1 (33.9% and 28.7%, respectively).
To assess the relationship of BDR to radiographic emphysema (CT density ≤−950 HU), we divided COPD subjects into quartiles by quantity of emphysema observed on HRCT (Figure 2D). Subject age did not differ significantly across the quartiles. BDRFVC was more prevalent in those with more emphysema (Quartile 4, 49.8 versus 33.7%), in contrast to those with less emphysema (Quartiles 1 and 2) where BDRFEV1 was more prevalent.
Volume Responsiveness Correlates with PRM Analysis of Small Airway Disease and Emphysema
To evaluate whether BD responders have more small airway disease in comparison to BD nonresponders, we analyzed parametric response mapping (PRM) in relationship to FVC and FEV1 BDR status. PRM analysis demonstrated significantly more functional small airway disease (PRMfSAD) which is equivalent to air trapping in FVC-BD responders compared with FVC-BD nonresponders, but showed no difference between FEV1-BD responders and nonresponders (Figure 3).
Clinical relevance of BDRFVC
FVC-BD responders had lower post-BD FEV1, more emphysema, more small airway disease, and poorer health-related quality of life measured by SGRQ compared to nonresponders. FVC-BD responders also had more self-reported use of inhaled bronchodilators and inhaled steroids relative to FVC-BD nonresponders. By contrast, FEV1 BD-responders were associated with current smoking status and fewer exacerbations reported at baseline (Table 2).
Over the 3-year study period, FVC-BD responders had reduced survival in comparison to FVC-BD nonresponders (88.1% vs 91.7%, P<0.05) (Figure 4). This difference was significant in a univariable Cox proportional hazards model (HR=1.46, CI: 1.02–2.08). In an univariable negative binomial model, BDRFVC was associated with an increased incidence rate ratio (RR) for exacerbations, relative to FVC-BD nonresponders (RR=1.30, CI:1.12–1.52). However, in multivariate models adjusted for known risk factors, including post-BD FEV1, these associations were no longer significant for either exacerbation (RR=1.12, CI: 0.96–1.31) or mortality (HR=1.03, CI=0.71–1.47), Supplemental Table 2.
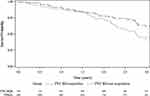 |
Figure 4 Kaplan–Meier plot of overall survival up to 3 years: FVC-BD responders (88.1%) vs FVC-BD nonresponders (91.7%) (P<0.05). |
Finally, to understand the diverging proportions of flow-based versus volume-based BDR in advanced COPD, we analyzed subjects who demonstrated BDRFVC but not BDRFEV1. These subjects represented 32% of all FVC-BD responders (N=238), and in comparison to individuals who demonstrated both BDRFEV1 and BDRFVC (N=496), they had more emphysema (Figure 5A) and more exacerbations during the follow-up period (Figure 5B). A higher risk of exacerbations was observed in isolated BDRFVC relative to other COPD subjects who were not isolated FVC-BD responders (HR 1.71, CI: 1.09–2.67) (Supplemental Table 3). Isolated BDRFVC was characterized by a higher 3-year mortality relative to other COPD participants. Nevertheless, stratified by post-BD FEV1 in a multivariate model, there was no association between isolated BDRFVC and exacerbations or mortality risk (Supplemental Figure 1).
Discussion
In a longitudinal analysis of 2,974 individuals with and without COPD, we evaluated the prevalence and clinical implications of BDR. Focused on distinctions between BDRFEV1 and BDRFVC, our study revealed several interesting observations.
As reported previously,4,6,11,20 BDR is present in a majority of participants with COPD. Despite being a common feature of this disease, it is still often misinterpreted as a hallmark of asthma, a misconception originating in part by COPD being defined by “persistent airflow limitation”.12 Reversibility of airflow obstruction or, normalization of FEV1/FVC ratio after BD administration, is absent in COPD, but BDR, a measure of BD-induced change in lung volumes rather than ratios, is frequent and does not necessarily imply the coexistence of asthma.21 While the self-reported history of asthma in our cohort was associated with BDR, this parameter cannot be used to differentiate between or define asthma or COPD, since it is frequently observed in both conditions.22 Analyzing BDR among healthy never-smokers without an asthma history showed that a significant proportion of these individuals showed either flow-based or volume-based BDR with frequencies similar to reported values,23 indicating that BDR also poorly discriminates diseased from healthy airways.24 Our data add to the evidence of the lack of association of BDR with blood eosinophils,25 and we show that average blood eosinophil counts (BEC) were similar among BD responders and BD nonresponders, with both FEV1 and FVC-BD responders having similar BEC compared to FEV1 and FVC nonresponders, respectively.
Despite such limitations, the clinical significance of BDR increases when its pattern is analyzed with regard to changes in both FEV1 and FVC. This is particularly important in advanced COPD, where distal airway remodeling and emphysema with loss of alveolar attachments may lead to an early expiratory collapse of small airways with subsequent air trapping and dynamic hyperinflation,26,27 resulting in a less significant impact on the post-bronchodilator change in FEV1 in comparison to the change in FVC. The increase in the prevalence of BDRFVC closely reflected the progression of emphysema and small airway disease, as demonstrated in the present study by quantitative HRCT and PRM. Small airway disease, one of the key features of COPD, may lead to air-trapping and hyperinflation with an increase in functional residual capacity (FRC) and a corresponding decrease in IC. BD administration can induce significant reductions in lung hyperinflation, manifested by a response in FVC or IC even in the absence of significant improvement in FEV1 in a majority of individuals with advanced emphysema, and the benefit may be greatest in those with the most severe disease. These findings suggest that BDRFVC offers an insight into pathophysiologic processes in advanced airway disease, which have been previously described.10,11
The distribution pattern of BDRFVC was, in agreement with that reported previously,10,28 infrequent in healthy subjects and ever-smokers without COPD. In early COPD, BDRFVC was uncommon relative to BDRFEV1, but became more prevalent as the disease progressed, being highest in the most advanced disease, whether defined spirometrically or by the GOLD grading system.12 In contrast, BDRFEV1 was rare in subjects with spirometrically very severe COPD, thus failing to identify the actual prevalence of BD responsiveness in these individuals. This observation can also explain why FVC-BD responsiveness in the absence of BDRFEV1 is associated with a higher risk of exacerbations in univariate analysis while this effect is lost in a model adjusted for FEV1.
Does BDRFVC have other relevant clinical implications in COPD management? We found that FVC-BD responders with COPD had lower post-BD FEV1% predicted, more often used steroids and inhaled BD, and had more respiratory symptoms than FVC-BD nonresponders, despite similar age, sex, smoking history and BMI, all results suggesting more advanced or active disease. Although our FVC-BD responsive participants reported the same frequency of exacerbations in the year before enrollment as nonresponders, they were more likely to exacerbate during the 3-year follow-up period and their mortality was significantly worse than FVC-BD nonresponders. However, these findings were no longer significant in a multivariate model adjusted for post-BD FEV1% predicted. Similar findings were reported in a study where BDR was tested using salbutamol only,9 in which BDR identified frequent exacerbators, with the lack of statistical significance after the inclusion of pre-BD FEV1 as a covariate. In a different COPD cohort,29 baseline BDR was predictive of a greater mean rate of FEV1 decline over 3 years than observed in the entire cohort (33 mL/year vs 17 mL/year); however, the mean baseline FEV1 was substantially higher among BD responders compared to BD nonresponders. In small randomized controlled trials, BDR correlated with lower exercise capacity and worse quality-of-life scores.30
While this study is in agreement with other studies that failed to demonstrate that BDR represents a distinct clinical phenotype predictive of outcomes,4,8,9 our findings suggest that, in appropriate clinical settings, analyzing BDRFVC and BDRFEV1 status may offer treating physicians additional insights about their patients, particularly with regard to the presence of hyperinflation.
Our study has several limitations. We did not analyze the actual values of post-BD changes in FEV1 or FVC, but instead followed the accepted practice of a categorical classification of BD responsiveness versus and BD nonresponsiveness.3 We applied one among several existing criteria proposed to define BDR4 and thus cannot extend our findings to universal clinical settings or other definitions. Since the current diagnosis of asthma represented one of the exclusion criteria for the enrollment in the study, the possible presence of asthma–COPD overlap syndrome cannot be precisely analyzed in this report.31 We have also analyzed only currently available data for subjects who continue to be followed through the SPIROMICS study cohort, so that the reported associations with outcomes cannot be considered final. These limitations are balanced by our goal to relate a common use of spirometry to clinical management.
Several strengths merit emphasis. One is our large cohort of ever-smokers without and with COPD, whose clinical characteristics were well described at baseline and longitudinally, allowing for the adequate association of BDR with multiple clinical outcomes. We analyzed several metrics that reflect BDR, including comprehensive imaging assessment and novel biometric measures such as PRM, which offered additional insight into pathophysiologic processes in COPD. Unlike other studies evaluating BDR in COPD,9 we attempted optimal BDR testing, via higher doses of both a short-acting beta-agonist and a short-acting muscarinic antagonist, and allowed sufficient time for the nearly full medication effect. Using different classes of short-acting inhaled agents at twice their usual recommended dose is supported by established evidence of their additive effect.32
Conclusion
BDR was highly prevalent among COPD subjects in the SPIROMICS cohort. Defined using standard criteria, BDRFEV1 was observed more often in subpopulations of healthy subjects and ever-smokers either without airflow obstruction or with early stages of COPD. In contrast, BDRFVC was more prevalent in advanced COPD and associated with increases in emphysema and small airway disease measured by HRCT. BDRFVC status correlated with increased exacerbations and mortality, although this association may partly be a consequence of the markedly reduced FEV1 in individuals with advanced COPD.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Acknowledgements
Participants: The authors thank the SPIROMICS participants and participating physicians, investigators, and staff for making this research possible. More information about the study and how to access SPIROMICS data is at www.spiromics.org. In addition to coauthors of this manuscript, we would like to acknowledge the following current and former investigators of the SPIROMICS sites and reading centers: Neil E Alexis, PhD, Eugene R Bleecker, MD, Richard C Boucher, MD, Alejandro P Cornellas, MD, Ronald G Crystal, MD, Brett Dolezal, PhD, Freeman, PhD, Annette T Hastie, PhD, Eric C Kleerup, MD, Lisa M LaVange, PhD, Stephen C Lazarus, MD, Deborah A Meyers, PhD, John D Newell Jr, MD, Elizabeth C Oelsner, MD, MPH, Nirupama Putcha, MD, MHS, Mary Beth Scholand, MD, and Robert A Wise, MD. The project officers from the Lung Division of the National Heart, Lung, and Blood Institute were Lisa Postow, PhD, and Thomas Croxton, PhD, MD.
Author Contributions
IB and CBC had full access to all of the data in the study and take responsibility for the integrity of the data and accuracy of the analysis. IB, CBC, SH, XW, RGB, DT contributed to the conception and design of the study. All authors contributed to data analysis, drafting and revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
IB has received research grants from AMGEN and GE Healthcare; and reports personal fees from Astra Zeneca, GSK, Boehringer Ingelheim, GE Healthcare, Theravance, Mylan, GRIFOLS, CSL Behring, Verona Pharma and Fisher & Pykel Healthcare. SPB is supported by NIH Grant K23HL133438 and he has served on an advisory board for Sunovion and reports grants from NIH, personal fees from Sunovion, personal fees from GlaxoSmithKline, outside the submitted work. JLC is supported by Merit Review award I01 CX000911 from the Department of Veterans Affairs, and reports grants the Department of Defense, the National Institutes of Health, and from MedImmune Corporation, Ltd., and reports grants from NIH/NHLBI, during the conduct of the study; grants from NIH/NIAID, grants from Department of Veterans Affairs, grants from Department of Defense, outside the submitted work. MKH has consulted for GSK, Boehringer Ingelheim and AstraZeneca, has received research support from Novartis and Sunovion and reports grants from NIH, during the conduct of the study; and Consulting for GSK, BI, Mylan and AstraZeneca, research support from Sunovion and Novartis. FJM reports grants from NHLBI, National Institutes of Health, personal fees from Continuing Education, personal fees from Forest Laboratories, Janssen, GlaxoSmithKline, Nycomed/Takeda, AstraZeneca, Boehringer Ingelheim, Bellerophon (formerly Ikaria), Genentech, Novartis, Pearl, Roche, Sunovion, Theravance, CME Incite, Annenberg Center for Health Sciences at Eisenhower, Integritas, InThought, National Association for Continuing Education, Paradigm Medical Communications, LLC, PeerVoice, UpToDate, Haymarket Communications, Western Society of Allergy and Immunology, Proterixbio (formerly Bioscale), Unity Biotechnology, ConCert Pharmaceuticals, Lucid, Methodist Hospital, Columbia University, Prime Healthcare Ltd, WebMD, PeerView Network, California Society of Allergy and Immunology, Chiesi, Puerto Rico Thoracic Society, outside the submitted work, and reports personal fees from Afferent/Merck, personal fees from American Thoracic Society, grants, personal fees, non-financial support from AstraZeneca, personal fees from Bayer, non-financial support from Boehringer Ingelehim, personal fees from ProTerrix Bio, personal fees from Bridge Biotherapeutics, personal fees, non-financial support from Chiesi, personal fees from Gala, personal fees, non-financial support, personal fees from Genentech, grants, personal fees, non-financial support from GlaxoSmithKline, grants, personal fees from Nitto, personal fees from ProMedior, personal fees from ProMetic, personal fees from Patara/Respivant, personal fees from Biogen, personal fees, non-financial support from Sunovion, personal fees, non-financial support from Teva, personal fees from Veracyte, during the conduct of the study. NH reports grants and personal fees from AstraZeneca, GSK, Boehringer Ingelheim, grants from NIH, COPD Foundation, outside the submitted work. GB has grants from the NIH, Foundation for the NIH, COPD Foundation and Alpha-1 Foundation, and reports grants, personal fees from AstraZeneca, grants from Boehringer Ingelheim, grants from NIH, grants from COPD Foundation, personal fees from Mylan, outside the submitted work. JMW has received grant support from the NIH, contracts to conduct research from GSK, Bayer, MereoBioPharma,Quintiles, and reports grants from NIH/NHLBI, during the conduct of the study; grants from NIH/NCATS, grants from Bayer, grants, personal fees from GSK, personal fees from Boehringer Ingelheim, grants, personal fees from Mereo BioPharma, personal fees from Quintiles, outside the submitted work. EAH a founder and shareholder of VIDA Diagnostics, a company commercializing lung image analysis software developed, and reports personal fees from VIDA Diagnostics, during the conduct of the study. VK has consulted for Boehringer Ingelheim, Gala Therapeutics and AstraZeneca and received personal fees from ABIM, and reports personal fees from Medscape, personal fees from Gala Therapeutics, personal fees from ABIM Critical Care Testwriting Committee, personal fees from AstraZeneca, personal fees from Boehringer Ingelheim, outside the submitted work. MTD reports receiving grants from the NIH, the Department of Defense, and the American Heart Association; consulting fees from Boehringer Ingelheim, GlaxoSmithKline, Novartis, Astra Zeneca, Yungjin, PneumRx/BTG, Pulmonx, Genentech, Boston Scientific, Quark Pharmaceuticals, Mereo and received grants from American Lung Association and NIH, and reports grants from NIH, during the conduct of the study; personal fees from Boehringer Ingelheim, personal fees from AstraZeneca, personal fees from GlaxoSmithKline, personal fees from Boston Scientific, grants from American Lung Association, grants from Department of Defense, grants from Department of Veterans Affairs, personal fees from Mereo, personal fees from Quark, outside the submitted work. MBD has received research grants from the NIH and reports personal fees from Boehringer-Ingelheim, GlaxoSmithKline, AstraZeneca, and Mylan-Theravance, outside the submitted work, and reports grants from NIH-NHLBI, during the conduct of the study; grants, personal fees from Boehringer-Ingelheim, personal fees from GlaxoSmithKline, personal fees from AstraZeneca, personal fees from Mylan-Theravance, grants from Department of Defense, personal fees from Novavax, personal fees from Parion, personal fees from Midmark, personal fees from Philips, outside the submitted work. SAC reports personal fees from AstraZeneca, GSK, Amgen, Glenmark, Sunovion, UpToDate, and received personal fees and non-financial support from Genentech, grants from MedImmune, outside the submitted work, and reports personal fees from AstraZeneca, personal fees from GlaxoSmithKline, personal fees from Amgen, personal fees from Glenmark, personal fees from Sunovion, personal fees from Genentech, non-financial support from Medimmune, outside the submitted work. JAK has received research grants from NIH and the Patient Centered Outcomes Research Institute. DPT reports personal fees from Boehringer-Ingelheim, AstraZeneca, Sunovion, Theravance/Innoviva, Mylan, outside the submitted work, and reports personal fees from AstraZeneca, personal fees from Sunovion, during the conduct of the study; personal fees from AstraZeneca, personal fees from Sunovion, personal fees from Boehringer-Ingelheim, personal fees from Mylan, outside the submitted work. CBC has consulted with PulmonX, has received research funding from Equinox Fitness Clubs, Amgen and is employed part-time by the GlaxoSmithKline Global Respiratory Franchise, and reports personal fees from GlaxoSmithKline, outside the submitted work. DC has grants from the NIH, reports grants from NHLBI, grants from COPD Foundation, during the conduct of the study and no other conflicts. RB served on the advisory boards (GlaxoSmithKline, Boehringer Ingelheim, and Mylan Pharmaceuticals) and received research grants from GlaxoSmithKline and Boehringer Ingelheim, and reports personal fees from GlaxoSmithKline, personal fees from Boehringer Ingelheim, personal fees from Mylan Pharmaceuticals, grants from GlaxoSmithKline, grants from Boehringer Ingelheim, outside the submitted work. RP reports grants from NHLBI, grants from COPD Foundation, NHLBI and Department of Veterans Affairs, outside the submitted work. RGB received personal fees from GlaxoSmithKline, grants from NIH/National Center for Advancing Translational Sciences, grants from NIH/NHLBI, and reports grants from NIH/NCATS, during the conduct of the study; personal fees from GlaxoSmithKline, grants from NIH/NHLBI, outside the submitted work; and Dr. Buhr is employed part-time by the Veterans Health Administration; the content of this manuscript does not necessarily reflect the views of the US Department of Veterans Affairs. RJK received grants and personal fees from Genentech, Boehringer Ingelheim, Medimmune/Astra Zeneca, and Gilead and reports grants from NIH, during the conduct of the study; grants, personal fees from Boehringer Ingelheim, grants, personal fees from Roche/Genentech, outside the submitted work. GC reports grants from Boehringer- Ingelheim, Novartis, Astra Zeneca, Respironics, MedImmune, Actelion, Forest, Pearl, Ikaria, Aeris, PneumRx, Pulmonx, personal fees from HGE Health Care Solutions, Inc, Amirall, Boehringer- Ingelheim, Holaira. NB reports grants from NIH, outside the submitted work. PW reports personal fees from Glenmark Pharmaceuticals, personal fees from GSK, personal fees from NGM Pharma, personal fees from Amgen, nothing from Regeneron, nothing from 23andMe, nothing from Theravance, nothing from AstraZeneca, outside the submitted work. CMD reports grants from NIH, during the conduct of the study. SP reports grants from MIH, HNLBI, during the conduct of the study. The authors report no other conflicts of interest in this work.
References
1. Celli BR, MacNee W, Force AET. Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. Eur Respir J. 2004;23(6):932–946.
2. Pellegrino R, Viegi G, Brusasco V, et al. Interpretative strategies for lung function tests. Eur Respir J. 2005;26(5):948–968.
3. Miller MR, Hankinson JA, Brusasco V, et al. Standardisation of spirometry. Eur Respir J. 2005;26(2):319–338. doi:10.1183/09031936.05.00034805
4. Hanania NA, Sharafkhaneh A, Celli B, et al. Acute bronchodilator responsiveness and health outcomes in COPD patients in the UPLIFT trial. Respir Res. 2011;12:6. doi:10.1186/1465-9921-12-6
5. Tashkin DP, Celli B, Decramer M, et al. Bronchodilator responsiveness in patients with COPD. Eur Respir J. 2008;31(4):742–750. doi:10.1183/09031936.00129607
6. Walker PP, Calverley PM. The volumetric response to bronchodilators in stable chronic obstructive pulmonary disease. COPD. 2008;5(3):147–152. doi:10.1080/15412550802092928
7. O’Donnell DE, Webb KA. Exertional breathlessness in patients with chronic airflow limitation. The role of lung hyperinflation. Am Rev Respir Dis. 1993;148(5):1351–1357. doi:10.1164/ajrccm/148.5.1351
8. Calverley PM, Burge PS, Spencer S, et al. Bronchodilator reversibility testing in chronic obstructive pulmonary disease. Thorax. 2003;58(8):659–664. doi:10.1136/thorax.58.8.659
9. Albert P, Agusti A, Edwards L, et al. Bronchodilator responsiveness as a phenotypic characteristic of established chronic obstructive pulmonary disease. Thorax. 2012;67(8):701–708. doi:10.1136/thoraxjnl-2011-201458
10. Quanjer PH, Ruppel GL, Langhammer A, et al. Bronchodilator response in FVC is larger and more relevant than in FEV1 in severe airflow obstruction. Chest. 2017;151(5):1088–1098.
11. Ben Saad H, Préfaut C, Tabka Z, Zbidi A, Hayot M. The forgotten message from gold: FVC is a primary clinical outcome measure of bronchodilator reversibility in COPD. Pulm Pharmacol Ther. 2008;21(5):767–773.
12. Singh D, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease: the GOLD science committee report 2019. Eur Respir J. 2019;53(5):1900164.
13. Gunen H, et al. Factors affecting survival of hospitalised patients with COPD. Eur Respir J. 2005;26(2):234–241.
14. Cote CG, Dordelly LJ, Celli BR. Impact of COPD exacerbations on patient-centered outcomes. Chest. 2007;131(3):696–704.
15. Couper D, LaVange LM, Han M. Design of the subpopulations and intermediate outcomes in COPD study (SPIROMICS). Thorax. 2014;69(5):491–494.
16. Vestbo J, Hurd S, Anzueto A, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2013;187(4):347–365.
17. Sieren JP, Newell JD
18. Boes JL, Hoff BA, Bule M, et al. Parametric response mapping monitors temporal changes on lung CT scans in the subpopulations and intermediate outcome measures in COPD study (SPIROMICS). Acad Radiol. 2015;22(2):186–194.
19. Anderson WH, Ha JW, Couper DJ, et al. Variability in objective and subjective measures affects baseline values in studies of patients with COPD. PLoS One. 2017;12(9):e0184606.
20. Celli BR, Tashkin DP, Rennard SI, et al. Bronchodilator responsiveness and onset of effect with budesonide/formoterol pMDI in COPD. Respir Med. 2011;105(8):1176–1188.
21. Barjaktarevic I, Kaner R, Buhr RG, et al. Bronchodilator responsiveness or reversibility in asthma and COPD - a need for clarity. Int J Chron Obstruct Pulmon Dis. 2018;13:3511–3513.
22. Muller V, Gálffy G, Orosz M, et al. Characteristics of reversible and nonreversible COPD and asthma and COPD overlap syndrome patients: an analysis of salbutamol easyhaler data. Int J Chron Obstruct Pulmon Dis. 2016;11:93–101.
23. Toren K, Bake B, Olin AC, et al. Measures of bronchodilator response of FEV1, FVC and SVC in a Swedish general population sample aged 50–64 years, the SCAPIS pilot study. Int J Chron Obstruct Pulmon Dis. 2017;12:973–980.
24. Fingleton J, Weatherall M, Beasley R. Bronchodilator responsiveness: interpret with caution. Thorax. 2012;67(8):667–668.
25. Hastie AT, Martinez FJ, Curtis JL, et al. Association of sputum and blood eosinophil concentrations with clinical measures of COPD severity: an analysis of the SPIROMICS cohort. Lancet Respir Med. 2017;5(12):956–967.
26. Celli B, ZuWallack R, Wang S, et al. Improvement in resting inspiratory capacity and hyperinflation with tiotropium in COPD patients with increased static lung volumes. Chest. 2003;124(5):1743–1748.
27. Sutherland ER, Cherniack RM. Management of chronic obstructive pulmonary disease. N Engl J Med. 2004;350(26):2689–2697.
28. Tan WC, Vollmer WM, Lamprecht B, et al. Worldwide patterns of bronchodilator responsiveness: results from the burden of obstructive lung disease study. Thorax. 2012;67(8):718–726. doi:10.1136/thoraxjnl-2011-201445
29. Vestbo J, Edwards LD, Scanlon PD, et al. Changes in forced expiratory volume in 1 second over time in COPD. N Engl J Med. 2011;365(13):1184–1192. doi:10.1056/NEJMoa1105482
30. Ortega F, Marquez-Martin E, Valencia B, et al. Impact of bronchodilator responsiveness on quality of life and exercise capacity in patients with COPD. Respir Care. 2014;59(1):81–89. doi:10.4187/respcare.02399
31. Tashkin DP. Is it asthma, COPD, or something in between, and does it matter?. Respir Care. 2012;57(8):1354–1356. doi:10.4187/respcare.01970
32. Dorinsky PM, Reisner C, Ferguson GT, et al. The combination of ipratropium and albuterol optimizes pulmonary function reversibility testing in patients with COPD. Chest. 1999;115(4):966–971. doi:10.1378/chest.115.4.966
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



