Back to Journals » Research and Reports in Urology » Volume 14
Clinical Profile and Outcome of Patients Operated on for Renal Cell Carcinoma: Experience from a Tertiary Care Center in a Developing Country
Authors Adem RY, Hassen SM, Abdulaziz M, Ahmed AI , Jemberie AM, Gebeyehu YT, Sedeta AM, Gebrehiwot FG , Abebe E, Berhe T
Received 31 May 2022
Accepted for publication 8 November 2022
Published 10 November 2022 Volume 2022:14 Pages 389—397
DOI https://doi.org/10.2147/RRU.S376720
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Guglielmo Mantica
Ramzi Yessuf Adem,1 Seid Mohammed Hassen,1 Mohammed Abdulaziz,1 Ahmed Ibrahim Ahmed,2 Atinkut Mengesha Jemberie,1 Yonatan Tedla Gebeyehu,1 Assefa Mekonnen Sedeta,1 Fitsum Gebreegziabher Gebrehiwot,1 Engida Abebe,1 Teklebirhan Berhe1
1Urology Unit, Department of Surgery, Saint Paul’s Hospital Millennium Medical College (SPHMMC), Addis Ababa, Ethiopia; 2Houston Methodist DeBakey Heart and Vascular Center, Houston, TX, USA
Correspondence: Ramzi Yessuf Adem, Urology Unit, Department of Surgery, Saint Paul’s Hospital Millennium Medical College (SPHMMC), 1271 Swaziland St, Addis Ababa, Ethiopia, Tel +251 911 242421, Email [email protected]
Purpose: With nearly 500,000 new cases and over 150,000 deaths worldwide in 2020, renal cancers remain a significant component of the global burden of cancer. The aim of this study is to describe the clinical presentation, peri-operative condition and short-term outcome of patients operated with the primary diagnosis of renal cell carcinoma (RCC) at a large tertiary care referral center.
Patients and Methods: A retrospective institution-based study was done. The study population consisted of all patients who were operated for a primary diagnosis of renal cell carcinoma from January 1st, 2015, to December 31st, 2020, at the Urology Unit of St Paul’s Hospital Millennium Medical College.
Results: The final cohort consisted of 107 patients (mean (standard deviation) age 49 (± 14) years, 48% male, 46% residence in Addis Ababa). The most common presenting complaint was flank pain (65%), followed by hematuria (34%) and abdominal mass (6%). One patient had the classic triad of RCC. The median (IQR) duration of illness was 9(7– 11) months. Fourteen (13%) patients were asymptomatic and diagnosed incidentally. Over half (57%) of the cohort were clinical TNM stage II, with the remaining 17%, 18% and 8% being stage I, III and IV, respectively. Nearly all patients (94%) underwent open radical nephrectomy with a transabdominal approach. Most patients (61%) had no Clavien-Dindo grade complications, and a minority (11%) experienced post-operative complications (7% postoperative bleeding, 6% hospital acquired pneumonia, 3% surgical site infection). The median (IQR) length of stay was 6 (5– 7.6) days. Nearly all patients (94%) were discharged and improved.
Conclusion: In this retrospective study, we have shown that patients operated for RCC are a low-risk cohort with few comorbidities, have a relatively short symptomatic course and good discharge outcome. Further prospective studies are needed to show the long-term outcome and factors associated with such outcomes in this patient population.
Keywords: renal cell carcinoma, nephrectomy, outcomes research, developing country
Introduction
Renal Cell Carcinoma (RCC) accounts for 80–90% of all renal malignancies, making it the 6th most frequently diagnosed cancer in men and 10th in women.1,2 Similar to most other malignancies of the urologic system, RCC’s predominantly present in men (with a 3:2 ratio) and in those >60 years of age.3 Several risk factors, such as obesity, smoking, urinary stones, and analgesics, such as non-steroidal anti-inflammatory drugs (NSAID), have been identified.3 Although historical studies found that the most common presentation was a triad of hematuria, abdominal mass and flank pain, as high as 50% of cases in developed countries are now incidental findings diagnosed on imaging performed for other indications.4–6
The treatment of RCC is challenging and requires a multidisciplinary approach. The mainstay of management for localized disease (American Joint Committee on Cancer stage I–II) is surgery, with systemic therapies reserved for metastatic diseases.7 Radical nephrectomy (RN), which involves the en-bloc removal of the kidney along with perinephric fat within Gerota’s fascia, has long been the cornerstone of management.8 More recently, studies have shown that kidney-sparing techniques such as partial nephrectomy (PN) yield comparable oncological outcomes with significantly improved perioperative morbidity and mortality. Indeed, guidelines from the American Urological Association (AUA), the National Comprehensive Cancer Network (NCCN) and the European Association of Urology (EUA) set PN as the standard of care for a majority of early-stage RCC.9–11
Most published studies on RCC are from developed countries (based on the definition by the World Bank Country and Lending Groups) with few from developing regions such as Sub-Saharan Africa. Thus, epidemiologic estimates show that a predominant number of cases of RCC occur in developing countries. The few studies that have been done in developing countries have shown patients present with advanced disease with poor prognosis.12,13 Ethiopia, an east African nation with an estimated incidence of over 2000 cases of renal malignancies in 2020 is one such country.1 The country has a three-tiered healthcare system funded by the government, consisting of the primary level of care (which includes primary hospitals, health centers and health posts), secondary level of care (consisting of general hospitals that serve 1 to 1.5 million people), and tertiary level of health care (with specialized hospitals that serve 3.5 to 5.0 million people). The aim of this study is to describe the clinical presentation, peri-operative condition and discharge outcome of patients operated with the primary diagnosis of RCC at a large tertiary care referral center in a developing country.
Materials and Methods
Cohort
An institution-based retrospective cohort study was done of patients who had undergone surgical intervention for RCC from January 1st, 2015, to December 31st, 2020, at St Paul’s Hospital Millennium Medical College (SPHMMC) which is in Addis Ababa, Ethiopia. SPHMMC is the second largest tertiary teaching hospital funded by the government, with a total of 500 beds. The hospital provides health service for 16,000 inpatients and 200,000 outpatients and 5000 surgeries annually with a catchment population of more than five million. Ethical clearance was obtained from SPHMMC ethical review board. Consent was waived due to the retrospective nature of the study as the research involved no more than minimal risk to the patients, waiver would not adversely affect the rights and welfare of subjects, and the study could not possibly be carried out without waiver. This study was in full compliance with the Declaration of Helsinki on principles for medical research involving human subjects.
Data
Information on sociodemographic variables (age, gender, educational and occupational status), comorbidities (hypertension, diabetes, dyslipidemia), smoking history, chief complaint, duration of illness, laboratory investigations (hemoglobin and creatinine), operative details (type of surgery, intra and post-op complications) and outcome at discharge were obtained using chart review of all patient records.
Comorbidities were recorded as absent if not documented in patient records. Clinical staging was done using the American Joint Committee on Cancer (AJCC) TNM staging.14 Peri-operative complications were graded using the Clavien-Dindo classification system.15
Continuous variables were presented as mean with standard deviation/medians with interquartile range, and categorical variables were presented as the number with percent. Comparisons were made using Student’s t-test, median testing, or chi-square test as appropriate. All analyses were done using Stata 17.0 (StataCorp, College Station, Texas), and a p-value of 0.05 was considered statistically significant.
Results
A total of 160 patients who were operated for renal cell carcinoma in the study period. Medical records could not be found for 36(22.5%) patients, 7(4.4%) patients had incorrect medical record numbers in operating room logbook and 10(6.3%) patients had incomplete medical records. Thus, the final cohort consisted of 107 patients.
Baseline Characteristics
Table 1 summarizes baseline characteristics of the study population. The mean (SD) age was 49(±14) years and 48% were men. A majority (46%) resided in Addis Ababa, with the remaining 28% 15% and 8% residing in Oromia, Amhara and Southern Nations and Nationalities state respectively. Educational status was unknown for over half (65%) of the cohort. The remaining 10%, 9% and 3% had completed secondary, primary and college education, respectively.
 |
Table 1 Baseline Characteristics of Patients |
Comorbidities were documented in a quarter of the patients (27% hypertension, 10% asthma and 2% heart disease). Of the comorbidities, there was a statistically significant difference in prevalence of hypertension across categories of TNM staging (p = 0.029).
Presenting Complaint
The most common presenting complaint was flank pain (65%), followed by hematuria (34%) and abdominal mass (6%). Twenty (19%) of patients had at least 2 symptoms and 1 (1%) patient had the classic RCC triad of abdominal mass, flank pain, and hematuria. The median (IQR) duration of illness was 9(7–11) months with a minority (10%) having symptoms for more than 2 years. There was no appreciable difference in duration across TNM stage (p = 0.72.) In contrast, 13% of patients were asymptomatic and diagnosed incidentally.
Investigations
Nearly all patients had both ultrasound and computed tomography (CT) imaging done. Right side tumors were slightly more prevalent than the left (51% vs 49%, respectively.) There were no patients with bilateral mass. Serum creatinine was elevated in 10% of patients and the mean(SD) hemoglobin was 13.8(±2.4).
Surgical Intervention and Peri-Operative Condition
Table 2 and Figures 1 summarize the peri-operative variables of patients. Most patients were TNM stage II (57%). Nearly all patients underwent open radical nephrectomy with a transabdominal approach. Two patients had partial nephrectomy and five had exploratory surgery for equivocal clinical and/or imaging findings.
 |
Table 2 Perioperative Condition and Outcome of Patients |
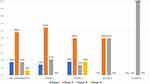 |
Figure 1 Clavien-Dindo classification by clinical stage of patients those with higher clinical stage were more likely to experience higher grade Clavien-Dindo complication. |
Most patients (61%) had no Clavien-Dindo complications while 14% and 22% of patients had Grade 1 and 2 respectively. There was no statistically significant difference in complications by clinical stage (p = 0.54.) Intra-operative bleeding and organ injury occurred in 6% and 5% of patients, with mesentery being the most commonly injured organ. One patient had an inferior vena-caval injury. A minority (11%) of patients experienced post-operative complications, with 6%, 3% and 1% experiencing hospital acquired infection, surgical site infection and acute kidney injury respectively. Thirteen patients had peri-operative bleeding (6 intra-operative and 7 post-operative) and 9(9%) ultimately required transfusion. There was no statistically significant difference in intra-operative or post-operative complications by clinical stage.
Outcome
The median (IQR) length of stay was 6 (5–7.6) days, with a minority (10%) staying beyond 10 days. The longest and shortest length of stays were 24 and 3 days, respectively. Nearly all patients (94%) were discharged and improved. There was a statistically significant difference in discharge disposition by clinical stage (p < 0.001).
Discussion
In this retrospective study of 107 patients, we have observed that patients operated for RCC at our institution were younger with few comorbidities, more likely to present with flank pain or hematuria, have symptomatic disease of less than one year, and have a relatively uncomplicated peri-operative and post-operative course with a high likelihood of short-term uncomplicated course.
There are several important observations that can be made from this study, all with implications to clinical practice.
First, the sociodemographic characteristics and comorbidity profile show our patients were a low-risk cohort. Our study population was of younger age and a balanced sex ratio with fewer than a third having had some known risk factor. Although this is in contrast to the epidemiology of RCC in developed countries which have shown patients with RCC are more often older age men with at least one of several identified risk factors, it is in agreement with a recent review of cases from western Africa.2,3,12 Although failure of documentation could account for the discrepancy in risk factors, this could not explain the younger age and near equal sex ratio of our patients. This indicates the risk factor profile for RCC is dependent on setting. One possibility, especially in light of the predominantly urban residence of patients would be an environmental exposure. Several studies have shown an increased risk with industrial agents such as Trichloroethylene and inorganic compounds such as arsenic and cadmium.16–20 A second possibility may be healthcare seeking behavior and access to care of urban vs rural residents. Further studies are needed to explain these findings.
Secondly, a small but significant (13%) number of our patients were incidental diagnoses. This is comparable from other studies done in sub-Saharan Africa where rates have ranged form 2.7%–11.8%.21,22 These numbers are dwarfed by those from developing countries, where as high as 50% of cases are detected when patients undergo clinically indicated imaging for an unrelated complaint.5,6 Although the relatively high proportion of patients presenting with incidental diagnosis would support the role for screening in early detection of RCC, patient safety (such as with radiation exposure), cost and low disease prevalence do not support such a strategy.23 However, these findings do support the thorough and comprehensive evaluation and reporting of patients undergoing abdominal imaging for any indication.
Thirdly, the most common operative technique used in our center was RN. Nephron sparing PN continues to increase in popularity in developed settings. The role of RN in such settings is limited to three scenarios’: management of large complex tumors, cytoreduction in metastatic RCC and in those with inferior vena-cava extension.24 Although the clinical efficacy of PN has been proven in a developed country setting, studies show that RN continues to be popular in developing countries and particularly in Sub-Saharan Africa.12 Suggested reasons have been the novelty PN and the need for intense and costly follow-up, both of which are difficult in resource limited settings. The peri-procedural cost is also high, particularly in developed countries as more and more laparoscopic PN (LPN) and robotic PN (RPN) are done.25 However, both LPN and RPN are associated with significantly lower operative time, estimated blood loss and post-procedural change in GFR.26 Patients treated with RPN also had lower rates of conversion to open/laparoscopic techniques, Calvin-Dindo complication rates, likelihood of positive margins and warm ischemia time.26 As an increasing proportion of asymptomatic cases at early stages are detected in developing countries, consideration should be made to address barriers in experience and resources that limit the use of PN.
Most of our patients had good peri-operative course and disposition at discharge. This is not surprising considering how a majority of the patients were TNM stage I or II. Prior studies have shown that TNM staging is the strongest predictor of short- and long-term prognosis and has recommendations in major guidelines to tailor subsequent management.2,9,10 However, the encouraging outcomes in this study might be biased considering how as high as 30% patients in some studies eventually develop recurrence.27
Minimally invasive nephrectomy (either laparoscopic or robotic assisted) has replaced open nephrectomy as standard of care in developed countries. This is because of improved operative success, lower length of stay as well as overall lower morbidity/mortality and readmission rate associated with minimally invasive nephrectomies.28–30 Thus, it is difficult to make a contemporary comparison of our findings with those of developed countries as patients are benefitting from a superior treatment modality, in addition to differences in sociodemographic factors (such as race and region) and healthcare access (such as availability of screening services and access to insurance). In contrast, our findings in terms of the sociodemographic presentation (younger age with balanced sex ratio),2,3,12 presentation (small but significant proportion with incidental diagnosis),21,22 option of treatment (open radical nephrectomy)24 and peri-operative outcomes are comparable to those from studies published in other developing countries.
Strengths
We used a large retrospective cohort of patients presenting to one of the only two major referral centers in the capital. Furthermore, we have described in detail the presenting features and peri-operative course of our patient population.
Limitations
Our study is not without limitations. Nearly a third of patient records could either not be retrieved or were mis-recorded. The extent and quality of data collected was limited by the retrospective nature of the study and reliance on patient records. However, care was taken to ensure data quality and data from patient records were cross-referenced with operating room logbook to ensure concordance. The single-center nature of our study may limit the generalizability of our findings. However, our institution is a tertiary care center with a broad referral catchment area. Thus, our results are representative of a patient population typical to tertiary care centers within the country. Details on final histologic diagnosis and detailed TNM staging were not available. We also did not have detailed information on post-surgical staging, which is an important factor in the use of adjuvant therapy. Similarly, laboratory values (such as LDH, calcium, CRP) and perioperative findings (such as operative time and estimated blood loss) were not available. Patient outcomes were ascertained at discharge, with no data on long-term prognosis. There is an inherent inclusion bias as these were patients deemed by the operating team to be fit for surgery. Hence, disposition at discharge would largely account for operative procedure and peri-operative period, the highest risk period for such patients.
Conclusion
In the current study, we have shown how patients operated for RCC are a low-risk cohort with few comorbidities, a short symptomatic course and good disposition at discharge. Our results are consistent with others in developing settings on the presentation and outcome of such patients. More importantly, our results show how radical nephrectomy is the predominant treatment provided for patients with RCC. This highlights how management of patients with RCC in Ethiopia still trails behind current recommendations which advocate for less aggressive management strategies that have similar short- and long-term prognosis. As one of a handful of studies showing the clinical profile and outcome of such patients in a developing country setting, our study fills an important gap in existing literature on the topic. Further prospective studies are needed to show the long-term outcome and factors associated with such outcomes in this patient population.
Acknowledgments
We would like to extend our gratitude to the St. Paul’s Hospital Millennium Medical College Department of Surgery and SPHMMC research office for the support to develop and finalize this research.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Sung H, Ferlay J, Siegel RL., et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–249. doi:10.3322/caac.21660
2. Ljungberg B, Campbell SC, Choi HY, et al. The epidemiology of renal cell carcinoma. Eur Urol. 2011;60(4):615–621. doi:10.1016/j.eururo.2011.06.049
3. Capitanio U, Bensalah K, Bex A, et al. Epidemiology of renal cell carcinoma. Eur Urol. 2019;75(1):74–84. doi:10.1016/j.eururo.2018.08.036
4. Skinner DG, Colvin RB, Vermillion CD, Pfister RC, Leadbetter WF. Diagnosis and management of renal cell carcinoma. A clinical and pathologic study of 309 cases. Cancer. 1971;28(5):1165–1177. doi:10.1002/1097-0142(1971)28:5<1165::AID-CNCR2820280513>3.0.CO;2-G
5. Sun M, Thuret R, Abdollah F, et al. Age-adjusted incidence, mortality, and survival rates of stage-specific renal cell carcinoma in North America: a trend analysis. Eur Urol. 2011;59(1):135–141. doi:10.1016/j.eururo.2010.10.029
6. Hollingsworth JM, Miller DC, Daignault S, Hollenbeck BK. Rising incidence of small renal masses: a need to reassess treatment effect. J Natl Cancer Inst. 2006;98(18):1331–1334.
7. Bamias A, Escudier B, Sternberg CN, et al. Current clinical practice guidelines for the treatment of renal cell carcinoma: a systematic review and critical evaluation. Oncologist. 2017;22(6):667–679. doi:10.1634/theoncologist.2016-0435
8. Kalapara AA, Frydenberg M. The role of open radical nephrectomy in contemporary management of renal cell carcinoma. Transl Androl Urol. 2020;9(6):3123–3139. doi:10.21037/tau-19-327
9. Campbell S, Uzzo RG, Allaf ME, et al. Renal mass and localized renal cancer: AUA guideline. J Urol. 2017;198(3):520–529. doi:10.1016/j.juro.2017.04.100
10. Motzer RJ, Jonasch E, Agarwal N, et al. Kidney cancer, version 2.2017, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2017;15(6):804–834. doi:10.6004/jnccn.2017.0100
11. Ljungberg B, Albiges L, Abu-Ghanem Y, et al. European Association of Urology guidelines on renal cell carcinoma: the 2019 update. Eur Urol. 2019;75(5):799–810. doi:10.1016/j.eururo.2019.02.011
12. Cassell A, Jalloh M, Yunusa B, et al. Management of renal cell carcinoma-current practice in sub-saharan Africa. J Kidney Cancer VHL. 2019;6(2):1–9. doi:10.15586/jkcvhl.2019.122
13. Zekri J, Dreosti LM, Ghosn M, et al. Multidisciplinary management of clear-cell renal cell carcinoma in Africa and the Middle East: current practice and recommendations for improvement. J Multidiscip Healthc. 2015;8:335–344. doi:10.2147/JMDH.S85538
14. Ficarra V, Galfano A, Mancini M, Martignoni G, Artibani W. TNM staging system for renal-cell carcinoma: current status and future perspectives. Lancet Oncol. 2007;8(6):554–558. doi:10.1016/S1470-2045(07)70173-0
15. Clavien PA, Barkun J, de Oliveira ML, et al. The clavien-dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250(2):187–196. doi:10.1097/SLA.0b013e3181b13ca2
16. Song J, Luo H, Yin X, et al. Association between cadmium exposure and renal cancer risk: a meta-analysis of observational studies. Sci Rep. 2015;5:17976. doi:10.1038/srep17976
17. Abdul KSM, Jayasinghe SS, Chandana EPS, Jayasumana C, De Silva P, Mangala CS. Arsenic and human health effects: a review. Environ Toxicol Pharmacol. 2015;40(3):828–846. doi:10.1016/j.etap.2015.09.016
18. DeSimone MC, Rathmell WK, Threadgill DW. Pleiotropic effects of the trichloroethylene-associated P81S VHL mutation on metabolism, apoptosis, and ATM-mediated DNA damage response. J Natl Cancer Inst. 2013;105(18):1355–1364. doi:10.1093/jnci/djt226
19. Kabat GC, Silvera SAN, Miller AB, Rohan TE. A cohort study of reproductive and hormonal factors and renal cell cancer risk in women. Br J Cancer. 2007;96(5):845–849. doi:10.1038/sj.bjc.6603629
20. Lambe M, Lindblad P, Wuu J, Remler R, Hsieh C. Pregnancy and risk of renal cell cancer: a population-based study in Sweden. Br J Cancer. 2002;86(9):1425–1429. doi:10.1038/sj.bjc.6600263
21. Muhammed A, Ahmad B, Yusuf MH, Almustapha LA, Abdullahi S, Tijjani LA. Pathologic characteristics and management of renal cell carcinoma in Zaria, Nigeria. Sub Saharan Af J Med. 2015;2(1):1. doi:10.4103/2384-5147.151559
22. Fall B, Diao B, Sow Y, et al. Adult renal cancer in Senegal: current epidemiological, clinical features, profile’s evolution over the two past decades. Prog Urol. 2011;21(8):521–526. doi:10.1016/j.purol.2011.02.013
23. Rossi SH, Klatte T, Usher-Smith J, Stewart GD. Epidemiology and screening for renal cancer. World J Urol. 2018;36(9):1341–1353. doi:10.1007/s00345-018-2286-7
24. Kalapara AA, Frydenberg M. The role of open radical nephrectomy in contemporary management of renal cell carcinoma. Transl Androl Urol. 2020;9(6):3123–3139.
25. Wu Z, Li M, Liu B, et al. Robotic versus open partial nephrectomy: a systematic review and meta-analysis. PLoS One. 2014;9(4):e94878. doi:10.1371/journal.pone.0094878
26. Leow JJ, Heah NH, Chang SL, Chong YL, Png KS. Outcomes of robotic versus laparoscopic partial nephrectomy: an updated meta-analysis of 4919 patients. J Urol. 2016;196(5):1371–1377. doi:10.1016/j.juro.2016.06.011
27. Klatte T, Rossi SH, Stewart GD. Prognostic factors and prognostic models for renal cell carcinoma: a literature review. World J Urol. 2018;36(12):1943–1952. doi:10.1007/s00345-018-2309-4
28. Dursun F, Elshabrawy A, Wang H, et al. Survival after minimally invasive vs. open radical nephrectomy for stage I and II renal cell carcinoma. Int J Clin Oncol. 2022;27(6):1068–1076. doi:10.1007/s10147-022-02153-5
29. Pereira J, Renzulli J, Pareek G, et al. Perioperative morbidity of open versus minimally invasive partial nephrectomy: a contemporary analysis of the National Surgical Quality Improvement Program. J Endourol. 2018;32(2):116–123. doi:10.1089/end.2017.0609
30. Khalil MI, Ubeda J, Soehner T, et al. Contemporary Perioperative Morbidity and Mortality Rates of Minimally Invasive vs Open Partial Nephrectomy in Obese Patients with Kidney Cancer. J Endourol. 2019;33(11):920–927. doi:10.1089/end.2019.0310
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
