Back to Journals » Clinical Ophthalmology » Volume 17
Clinical Outcomes of a Monofocal, Optimized, Aspheric, Hydrophobic Acrylic Intraocular Lens Implant
Authors García-Tomás B, Marín-Sánchez JM , García-Elskamp C, Alcon-Ruiz E, Montesinos-López L, García Martínez-Lozano B
Received 4 September 2023
Accepted for publication 2 October 2023
Published 27 October 2023 Volume 2023:17 Pages 3215—3224
DOI https://doi.org/10.2147/OPTH.S434378
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Scott Fraser
Berta García-Tomás, José María Marín-Sánchez, Christian García-Elskamp, Encarnación Alcon-Ruiz, Laura Montesinos-López, Beatriz García Martínez-Lozano
Cataract and Refractive Surgery Department, Murcia, 30009, Spain
Correspondence: Berta García-Tomás, Cataract and Refractive Surgery Department, Oftalvist Murcia, Ronda Norte 21, Murcia, 30009, Spain, Tel +968 281 060, Email [email protected]
Purpose: To evaluate the refractive and visual outcomes of eyes implanted with monofocal, optimized, aspheric, hydrophobic acrylic intraocular lenses (IOL) following cataract surgery.
Methods: The study assessed 55 eyes implanted with CT LUCIA® 621P IOLs (Carl Zeiss Meditec AG, Jena, Germany) at 3-months postsurgery. The main outcome measures were refractive error, monocular corrected distance visual acuity (CDVA), monocular uncorrected distance visual acuity (UDVA), photopic and mesopic contrast sensitivity, and wavefront aberrations. Patients were asked to complete the Catquest-9SF questionnaire.
Results: At 3 months, the cumulative Snellen visual acuity was 20/20 in 94.55% of eyes and 20/25 or better in 100%. The difference between the UDVA and CDVA was either the same (70.91%) or better (29.09%) in all eyes. The mean Snellen decimal UDVA and DCVA were 1.07 ± 0.15 and 1.13 ± 0.11, respectively. The safety and efficacy indexes were 1.48 and 1.40, respectively. 47.27% of eyes showed a spherical equivalent ± 0.13 D, with 92.73% of the eyes were within ± 0.50 D and all eyes were within ± 1.00 D. The mean spherical equivalent was − 0.03 ± 0.30 D and the mean refractive cylinder − 0.36 ± 0.34 D. The log photopic and mesopic contrast sensitivity functions were good and similar for all spatial frequencies. All patients reported being either fairly satisfied (score 3) or very satisfied (score 4) with their vision (mean = 3.64 ± 0.49). No intra- and postoperative complications were reported during the 3 months of follow-up.
Conclusion: The current study demonstrates that excellent visual and refractive outcomes, as well as patient satisfaction, can be achieved after cataract surgery with optimized, aspheric CT LUCIA 621P monofocal IOLs.
Keywords: cataract, intraocular lens, aspheric, aberrations, contrast sensitivity, phacoemulsification
Introduction
Thanks to recent advances in optical technology, cataract and refractive surgery has entered a new era in terms of the design of intraocular lenses (IOLs). Until now, the goal of cataract surgery was not only to restore visual acuity but also to obtain spectacle-free distance vision with the patient’s best visual performance. One major development was the introduction of aspheric IOLs, which have a negative aspheric optical design. Aspheric IOLs correct the corneal spherical aberration to improve postimplant vision,1,2 especially the patient’s contrast sensitivity under low-light conditions.3,4 In negative aspheric IOLs, it should be pointed out that higher-order wavefront aberrations can be induced with significant tilt or decentration of the IOL. This is because the central and peripheral areas of the IOL might have different optical powers.5,6 However, aberration-free IOLs are less affected by misalignment.7,8
A new optical design that combines the advantages of both types of IOL has recently been proposed. They are called non-constant aberration aspheric IOLs and were launched on the market as CT LUCIA IOLs (Carl Zeiss Meditec AG, Jena, Germany). There are currently three models of lens available: CT LUCIA 601P,9–14 611P,14–21 and the latest 621P.22–24 Compared to previous CT LUCIA Models 601P and 611P, the 621P/PY has an optimized Zeiss optic aspheric profile, with an improved haptic design. The negative spherical aberration of the central zone of the CT LUCIA 621P is designed to balance the corneal positive spherical aberration for improved image quality. The positive spherical aberration in the peripheral zone is designed to increase tolerance to lens misalignment. Combined, the optical design has been developed to create balance between correcting and neutral effects on the asphericity of the eye.
To the best of our knowledge, only three studies have assessed the most recent model (621P); two were in vitro computed tomography studies to assess the lens’ geometry22 and its dynamics with the capsular bag,23 and the third was a retrospective clinical study to assess its performance.24 Accordingly, the main aim of our study was to analyze the refractive error, visual acuity, photopic and mesopic contrast sensitivity functions, wavefront aberrations, and, finally, the visual function scores with the Catquest-9SF questionnaire to assess the clinical outcomes obtained with this new model in cataract patients at 3-months postimplant.
Methods
This prospective study was approved by the Ethics Committee of the Hospital Clínico San Carlos, Madrid, Spain, and was conducted following the tenets of the Declaration of Helsinki. The study was also registered at the DRKS German Clinical Trials Register with the clinical registration number DRKS00029169. All patients recruited in our study gave their informed consent to participate in the clinical study. The inclusion criteria were patients with cataracts, aged ≥50 years, and regular corneal astigmatism up to 1.00 D. Exclusion criteria were irregular corneal astigmatism (ie, keratoconus), a history of corneal refractive surgery, and ocular abnormalities or diseases that could reduce visual function or postoperative IOL stability (eg, severe amblyopia or macular degeneration).
Intraocular Lenses and the Surgical Procedure
All eyes were implanted with monofocal CT LUCIA 621P IOLs, supplied fully preloaded in BLUESERT injectors. The 621P is a hydrophobic acrylic lens with C-loop platform haptics and an optimized ZEISS optic non-constant aberration aspheric design. It has a heparin-coated surface for smoother injection and unfolding, step-vaulted haptics to translate the optic posteriorly for better contact with the posterior capsule, and a 360° square edge design. The model has an optical zone of 6.0 mm, overall diameter of 13.0 mm, and a refractive index of 1.49 (Abbe number of 51). The lenses have a diopter range of 0.00 D to +34.00 D in 0.50 D increments. Standard cataract surgery was performed by three experienced surgeons (BGT, JMMS and CGE) using phacoemulsification with a 2.2 mm incision, targeting a 5.5 mm diameter capsulorhexis.
Pre- and Postoperative Assessment
All patients included in the study underwent slit-lamp and fundoscopic examinations before surgery to assess their ocular health and measure the Snellen decimal uncorrected distance visual acuity (UDVA), corrected distance visual acuity (CDVA), manifest refraction (sphere, cylinder and axis), intraocular pressure, corneal topography using a Pentacam® device (Oculus, Wetzlar, Germany), and biometry with an IOLMaster 700 device (Carl Zeiss Meditec AG, Jena, Germany). In all cases, the Barrett formula was used to calculate the IOL power and the target refraction was emmetropia.
Follow-up examinations were performed at 1- and 3-months postimplant, and included a standard eye exam with refraction tests, intraocular pressure measurements, and a slit-lamp exam. Monocular UDVA, CDVA and monocular photopic and mesopic contrast sensitivity functions were measured in each patient. Higher-order wavefront aberrations were measured in each eye using a Hartmann–Shack aberrometer (VAO, Voptica SL, Murcia, Spain) at a pupil diameter of 4.5 mm. Patients were also asked to complete the Catquest-9SF patient outcomes questionnaire, whose value in determining patient limitations in certain activities of daily living due to reduced vision has been well reported and recommended.25–29 Any surgical complications or postoperative adverse events were also recorded up to the last follow-up visit. The results were analyzed after the 3-month follow-up visit.
Statistical Analysis and Sample Size
The results were analyzed using Excel (2019, version 16.43, Microsoft Corporation, Redmond, WA, USA). Quantitative data are presented as ranges, means, and standard deviations (SD). Student’s t-test was used to make comparisons and the statistical significance was set to a p-value of <0.05. Assuming a sample size of 50 eyes, a 95% confidence interval, and a standard deviation of 0.12 logMAR (based on the study by Liu et al),14 then the primary estimate will have a precision of 0.0335 logMAR. We considered this to be adequate for the aim of this study, and therefore recruited 55 eyes in total, factoring in a possible drop-out rate of 10%.
Results
This prospective clinical study assessed the results of 55 eyes in 45 patients implanted with CT LUCIA 621P IOLs. The sample included 30 females and 15 males, with a mean age of 70.64 ± 6.73 years (range: 55–83 years). Table 1 shows the subjects’ preoperative demographics. Cataract surgery went well in all cases and no intra- or postoperative complications or IOL-related adverse events were reported either during surgery or up to the final follow-up visit.
 |
Table 1 Preoperative Demographics of Participants Implanted with CT LUCIA 621P IOLs Shown as Means, Standard Deviations (SD), and Ranges |
Figures 1 and 2 show the monocular visual acuity results obtained at 3-months postsurgery. Specifically, Figure 1 gives the cumulative proportion of eyes with given UDVA and CDVA values (20/x or better) and Figure 2 shows the change in visual acuity lines between UDVA and CDVA. Figure 1 demonstrates that 94.55% and 100% of eyes showed a cumulative Snellen visual acuity 20/20 and 20/25 or better, respectively, at 3-months postsurgery. From Figure 2, it is clear that the difference between UDVA and CDVA was the same (70.91%) or better (29.09%) in all eyes analyzed in our sample. At 3-months postimplant, the mean monocular Snellen decimal UDVA and CDVA were 1.07 ± 0.15 (0.70–1.20) and 1.13 ± 0.11 (0.90–1.20), respectively. At the 3-months visit, the safety index (calculated by dividing the mean postoperative CDVA by the mean preoperative CDVA) was 1.48 and the efficacy index (calculated by dividing the mean postoperative UDVA divided by the mean preoperative CDVA) was 1.40.
 |
Figure 1 Cumulative proportion of eyes with a certain level of uncorrected distance visual acuity (UDVA) and best-corrected distance visual acuity (CDVA) (20/x or better) at 3-months postsurgery. |
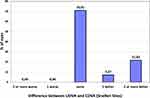 |
Figure 2 Change in visual acuity lines between the 3-months postoperative uncorrected distance visual acuity (UDVA) and [preoperative] best-corrected distance visual acuity (CDVA). |
Regarding the refractive outcomes, Figure 3 shows the distributions of postoperative spherical equivalent refraction and refractive cylinder (astigmatism). Nearly half of all implanted eyes, 47.27%, had a spherical equivalent of ±0.13 D, while 29.09% fell in the range between −0.50 D and −0.14 D. Looking at the accumulative results, 92.73% of the eyes were within ±0.50 D and all eyes were within ±1.00 D. The mean spherical equivalent at this follow-up (3 months) was close to emmetropia: −0.03 ± 0.30 D (range: –0.75 to 0.75 D). Figure 3 also presents the distribution of postoperative refractive cylinder: 80% of the eyes had a refractive astigmatism within ≤0.50 D and 96.36% were ≤1.00 D, while the mean postoperative refractive cylinder was −0.36 ± 0.34 D. The double-angle plots of preoperative corneal astigmatism and postoperative refractive astigmatism given in Figure 4 evidence a mean preoperative corneal astigmatism of 0.52 ± 0.22 D and a mean postoperative refractive astigmatism of 0.36 ± 0.34 D. The centroid decreased from 0.20 ± 0.54 D at 94° to 0.17 ± 0.47 D at 9° following cataract surgery.
 |
Figure 3 Distribution of postoperative spherical equivalent refraction (in D) and refractive cylinder (in D) at 3-months postsurgery. |
Figure 5 shows the log contrast sensitivity determined under photopic and mesopic conditions. The results obtained under both conditions were similar for all spatial frequencies (p > 0.05). The mean root mean square (RMS) of higher-order aberrations was 0.26 ± 0.07 µm, the mean spherical aberration was 0.06 ± 0.04 µm, and the mean coma was 0.12 ± 0.07 µm at a pupil diameter of 4.5 mm. Table 2 summarizes the patient-reported difficulties with their vision as determined per the Catquest-9SF patient outcomes questionnaire.
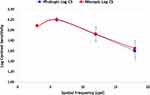 |
Figure 5 Contrast sensitivity function determined under photopic and mesopic conditions. |
Discussion
As mentioned in the introduction, three peer-reviewed publications have previously studied the new CT LUCIA 621P IOL.22–24 Two were in vitro studies22,23 and one was a retrospective clinical study.24 However, to the best of our knowledge, there are no prospective clinical studies that have fully assessed the postoperative outcomes with this lens in terms of refraction, visual acuity, contrast sensitivity, wavefront aberrations, and patient satisfaction. Hence, this study aimed to provide some information in this regard.
We obtained good visual acuity results; the cumulative Snellen visual acuity was 20/20 and 20/25 or better in 94.55% and 100% of eyes, respectively (see Figure 1), and the difference between the UDVA and CDVA was either the same (70.91%) or better (29.09%) in all eyes. In a retrospective clinical study of 90 eyes implanted with the same IOL and examined at 1-month postsurgery,24 the authors reported a postoperative CDVA of ≥20/25 in 80% of eyes and the difference between UDVA and CDVA was the same or better in all eyes. Our outcomes at 3 months corresponded to a mean Snellen decimal UDVA and CDVA of 1.07 ± 0.15 and 1.13 ± 0.11, respectively, while at 1 month, Hernández-Martínez et al24 found a mean monocular CDVA of 0.89 ± 0.13. So, the values obtained in our study were higher than those reported in the retrospective study. In fact, our standard safety and efficacy indexes were also higher than Martínez et al24 ≥1.40. For predictability, Figure 3 plots the distribution of postoperative spherical equivalent refraction (relative to the intended target refraction) and refractive cylinder in our series. The highest proportion of eyes, 47.27%, was in the ±0.13 D range followed by 29.09% in the range between −0.50 D and −0.14 D. The good accuracy results were reflected in the fact that 92.73% of the eyes were within ±0.50 D and all eyes within ±1.00 D, with a mean spherical equivalent of −0.03 ± 0.30 D (close to emmetropia). This is in contrast to results published previously,24 where 73.33% of eyes had an accuracy within ±0.50 D and 90% within ±1.00 D, and with a slightly myopic postoperative mean spherical equivalent: −0.18 ± 0.55 D. This is because their sample contained a higher percentage of eyes with a postoperative refractive cylinder >0.75 D compared to our series: 41.11%24 versus 7.28% (see Figure 3, bottom). In fact, Hernández-Martínez et al24 found a mean postoperative refractive cylinder of −0.81 ± 0.50 D, whereas out value was −0.36 ± 0.34D. Note that 31.11% of the eyes in their sample had preoperative corneal astigmatism >1.00 D. However, despite this, the authors concluded that the lens provided satisfactory postoperative visual acuity results.24
We also obtained good contrast sensitivity results under both high- and low-light conditions, with mean values ranging from 1.60 to 2.08 for low and high spatial frequencies with no significant differences between photopic and mesopic values (p > 0.05). This suggests that there was limited light scattering and that the lens is independent of pupil size. As for the optical quality of the eye once the lens was implanted, the RMS of higher-order aberrations was 0.26 ± 0.07 µm for pupils at 4.5 mm. Liu et al14 also measured wavefront aberration in 77 eyes implanted with a LUCIA lens (the 601P model) and recorded slightly higher mean values than ours: between approximately 0.35 and 0.45 µm for pupils at 4–5 mm. They also reported marginally higher values of spherical aberration and coma. The authors compared the 601P LUCIA lens against the CT ASPHINA 509M (spherical aberration: −0.18 µm) and AMO TECNIS® ZBV00 (spherical aberration: −0.27 µm) and found that the total RMS for ocular coma was significantly lower in the LUCIA group (p = 0.03). They also found no statistically significant differences between the three lenses in higher-order aberration (p = 0.85) and contrast sensitivity under both photopic and mesopic light conditions (p ≥ 0.05). Our results examining the new model with an optimized optical aspheric profile fully agree with these conclusions. It should be noted that the optimized ZEISS optic may be more resistant to decentering and tilting, and the thicker optic–haptic junction is expected to provide better centering and alignment, thus improving refractive predictability and stability, as reported for the CT LUCIA 611P model.15 Our results, coupled with those of Hernández-Martínez et al24 who implanted the new 621P model (which uses the same C-loop haptic design as the 611P), appear to endorse this notion considering the excellent predictability of the outcomes. Both studies reported a mean spherical equivalent of less than one-quarter of a diopter: −0.18 ± 0.55 D (current study) and −0.18 ± 0.55 D (Hernández-Martínez et al).24 According to the manufacturer, the optic was engineered around the realistic Liou–Brennan eye model, which is optimized for pupil sizes that are typically found in cataract patients. The central zone induces negative spherical aberration to balance any corneal aberration and improve image quality, whereas the peripheral zone induces positive spherical aberration to increase the tolerance to decentration. Thus, the 621P model creates an ideal balance between aberration correction and neutral effects.
An in vitro study by Borkenstein and Borkenstein22 analyzed the geometry of five commercially available one-piece, hydrophobic acrylic monofocal lenses (AcrySof SN60WF, Alcon Labs, USA; CT LUCIA 621PY; enVista MX60, Bausch&Lomb, USA; TECNIS ZCB00, Johnson&Johnson, USA; and Vivinex XY1, Hoya Surgical GmbH, Germany) and the subsequent changes in the haptic–capsular bag relationship as a function of different compression well diameters. They found that all haptic dimensions (length, thickness, surface area, and volume) and all optic–haptic junction dimensions (surface area and volume) were greatest for the CT LUCIA 621PY lens. They reported differences between the lenses with respect to the haptic angle of contact and capsular bag contact studied at all well sizes, but the CT LUCIA 621PY lens consistently had the highest angles for both parameters and the lowest percentage change between the smallest and largest diameter wells. The authors pointed out that IOLs with a design that maintains a consistent relationship and contact with the capsular bag, independent of native size, can be expected to confer good intraocular positional stability, limit the onset of posterior capsule opacification, and provide predictable visual outcomes after cataract surgery. Our results fully support these conclusions based on the refractive and visual acuity results.
In another experimental study, Zhang et al23 assessed different models of IOLs (including the CT LUCIA 621P) and capsular bags in human cadaver eyes using the Miyake–Apple posterior technique. The authors implanted the lenses into different sized capsular bags then assessed and compared the posterior capsule striae among the different models of lens. Specifically, they studied the arc of contact between the capsular equator and the lenses, the correlation between the capsular bag diameter with and without the IOL, and the correlation between the arc of contact and the empty capsular bag diameter. They found that the CT LUCIA 621P had a longer arc of contact than the RayOne (Rayner, United Kingdom) and Avansee 3P (Simonvision BV, Belgium) IOLs, but a shorter one than the CT ASPHINA (Carl Zeiss Meditec, Germany) and Avansee 1P (Simonvision BV, Belgium). In relation to the posterior capsule striae distribution, striae were found in all eyes implanted with the Avansee 3P lens, whereas not a single stria was observed with the CT LUCIA 621P and CT ASPHINA IOLs. It should be noted that the presence of two or more striae may indicate a greater disparity between the size of the capsular bag and the size of the lens.30,31 It has also been reported that the presence of striae in the posterior capsule may cause the third-order aberrations.32 The authors concluded that the RayOne, AcrySof (Alcon Labs, USA), and the CT LUCIA 621P lenses showed similar capsular stretching and sufficient arc of contact. It has been suggested that a longer arc of contact between the capsular equator and the haptic provides more stable lens fixation in the capsular bag when implanted.33 In terms of refractive stability up to the last postimplant visit, our results also support the in vitro dynamics study.
Furthermore, with respect to patient difficulties in daily activities related to vision and their postoperative visual satisfaction, we found that all patients in our series reported being fairly satisfied (a score of 3) or very satisfied (4) with their postimplant vision (mean 3.64 ± 0.49), while 54.54% did not report any difficulty in their daily activities (mean 3.55 ± 0.50, Table 2). With regard to difficulty carrying out various tasks, the results for distance activities were good (eg, 100% reported no difficulty recognizing faces). As was expected, some patients, although most had no problems, reported difficulty performing the near vision tasks defined in Catquest-9SF (ie, reading newspapers or subtitles on TV) because the lens was not designed to correct near vision. Consequently, we should consider that once implanted this lens achieved a wide range of satisfaction and quality of vision among our sample.
Study limitations were that the follow-up time was relatively short, then, the long-term effect of this lens implantation remains to be further analyzed. Also, there is no control group with other monofocal lenses available in the market in order to make direct comparisons, and it would be also interesting to assess the effect of different amounts of corneal spherical aberration in the final visual outcomes.
Conclusions
In conclusion, our results show that CT LUCIA 621P IOLs implanted in patients during cataract surgery offer excellent visual and optical performance in terms of visual acuity, contrast sensitivity, and wavefront aberrations, with good refractive outcomes. Patient-reported outcomes concerning visual satisfaction and the results of the Catquest-9SF quality of vision questionnaire were also good. According to our results, the IOL studied here can be considered an excellent choice for cataract patients. Future studies should consider a larger sample of eyes in order to confirm our results in eyes with different amounts of corneal spherical aberration.
Data Sharing Statement
The data are not available for sharing.
Funding
This study was funded by an investigator-sponsored study from Carl Zeiss Meditec, Inc. Carl Zeiss did not have any role in the study design, data collection and analysis, decision to publish, and preparation of the manuscript.
Disclosure
Dr Berta García-Tomás reports grants from Carl Zeiss Meditec, Inc., outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Packer M, Fine IH, Hoffman RS. Aspheric intraocular lens selection: the evolution of refractive cataract surgery. Curr Opin Ophthalmol. 2008;19(1):1–4. doi:10.1097/ICU.0b013e3282f2d791
2. Dick HB. Recent developments in aspheric intraocular lenses. Curr Opin Ophthalmol. 2009;20(1):25–32. doi:10.1097/ICU.0b013e32831b8bb3
3. Schuster AK, Tesarz J, Vossmerbaeumer U. The impact on vision of aspheric to spherical monofocal intraocular lenses in cataract surgery: a systematic review with meta-analysis. Ophthalmology. 2013;120(11):2166–2175. doi:10.1016/j.ophtha.2013.04.011
4. Schuster AK, Tesarz J, Vossmerbaeumer U. Ocular wavefront analysis of aspheric compared with spherical monofocal intraocular lenses in cataract surgery: systematic review with metaanalysis. J Cataract Refract Surg. 2015;41(5):1088–1097. doi:10.1016/j.jcrs.2015.04.005
5. Lawu T, Mukai K, Matsushima H, Senoo T. Effects of decentration and tilt on the optical performance of 6 aspheric intraocular lens designs in a model eye. J Cataract Refract Surg. 2019;45(5):662–668. doi:10.1016/j.jcrs.2018.10.049
6. Barbero S, Marcos S, Jiménez-Alfaro I. Optical aberrations of intraocular lenses measured in vivo and in vitro. J Opt Soc Am a Opt Image Sci Vis. 2003;20(10):1841–1851. doi:10.1364/JOSAA.20.001841
7. Shentu XC, Tang XJ, Yao K. Spherical aberration, visual performance and pseudoaccommodation of eyes implanted with different aspheric intraocular lens. Clin Exp Ophthalmol. 2008;36(7):620–624. doi:10.1111/j.1442-9071.2008.01856.x
8. Pieh S, Fiala W, Malz A, Stork W. In vitro strehl ratios with spherical, aberration-free, average, and customized spherical aberration-correcting intraocular lenses. Invest Ophthalmol Vis Sci. 2009;50(3):1264–1270. doi:10.1167/iovs.08-2187
9. Borkenstein AF, Borkenstein EM. Patient and surgeon satisfaction levels after using an acrylic, hydrophobic, monofocal IOL and the malyugin ring in pseudoexfoliation syndrome patients. J Ophthalmol. 2018;2018:3843098. doi:10.1155/2018/3843098
10. Nguyen J, Werner L, Ludlow J, et al. Intraocular lens power adjustment by a femtosecond laser: in vitro evaluation of power change, modulation transfer function, light transmission, and light scattering in a blue light-filtering lens. J Cataract Refract Surg. 2018;44(2):226–230. doi:10.1016/j.jcrs.2017.09.036
11. Labuz G, Knebel D, Auffarth GU, et al. Glistening formation and light scattering in six hydrophobic-acrylic intraocular lenses. Am J Ophthalmol. 2018;196:112–120. doi:10.1016/j.ajo.2018.08.032
12. De Giacinto C, Porrelli D, Turco G, Pastore MR, D’Aloisio R, Tognetto D. Surface properties of commercially available hydrophobic acrylic intraocular lenses: comparative study. J Cataract Refract Surg. 2019;45(9):1330–1334. doi:10.1016/j.jcrs.2019.04.011
13. Tandogan T, Auffarth GU, Son HS, Merz P, Choi CY, Khoramnia R. In-vitro glistening formation in six different foldable hydrophobic intraocular lenses. BMC Ophthalmol. 2021;21(1):126. doi:10.1186/s12886-021-01879-6
14. Liu Y, Zhao J, Hu Y, Li B, Wang J, Zhang J. Comparison of the visual performance after implantation of three aberration-correcting aspherical intraocular lens. Curr Eye Res. 2021;46(3):333–340. doi:10.1080/02713683.2020.1798467
15. Borkenstein AF, Borkenstein EM. Long-term clinical results and scanning electron microscopic analysis of the aspheric, hydrophobic, acrylic intraocular lens CT LUCIA 611P(Y). Clin Ophthalmol. 2018;12:1219–1227. doi:10.2147/OPTH.S167895
16. Borkenstein AF, Borkenstein EM. Surgical experience with a redesigned, fully preloaded, hydrophobic acrylic intraocular lens in challenging cases of pseudoexfoliation syndrome, phacodonesis, and small pupils. Clin Ophthalmol. 2019;13:199–206. doi:10.2147/OPTH.S194420
17. Ling R, Borkenstein EM, Borkenstein AF. Evaluation of Nd:YAG laser capsulotomy rates in a real-life population. Clin Ophthalmol. 2020;14:3249–3257. doi:10.2147/OPTH.S276329
18. Wormstone IM, Damm NB, Kelp M, Eldred JA. Assessment of intraocular lens/capsular bag biomechanical interactions following cataract surgery in a human in vitro graded culture capsular bag model. Exp Eye Res. 2021;205:108487. doi:10.1016/j.exer.2021.108487
19. Yildirim TM, Schickhardt SK, Wang Q, Friedmann E, Khoramnia R, Auffarth GU. Quantitative evaluation of microvacuole formation in five intraocular lens models made of different hydrophobic materials. PLoS One. 2021;16(4):e0250860. doi:10.1371/journal.pone.0250860
20. Hienert J, Hirnschall N, Ruiss M, Ullrich M, Zwickl H, Findl O. Prospective study to compare axial position stability after fellow-eye implantation of 2 distinct intraocular lens designs. J Cataract Refract Surg. 2021;47(8):999–1005. doi:10.1097/j.jcrs.0000000000000557
21. Schallhorn SC, Bonilla M, Pantanelli SM. Outcomes of a multicenter U.S. clinical trial of a new monofocal single-piece hydrophobic acrylic IOL. J Cataract Refract Surg. 2022;48(10):1126–1133. doi:10.1097/j.jcrs.0000000000000943
22. Borkenstein AF, Borkenstein EM. Geometry of acrylic, hydrophobic IOLs and changes in haptic-capsular bag relationship according to compression and different well diameters: a bench study using computed tomography. Ophthalmol Ther. 2022;11(2):711–727. doi:10.1007/s40123-022-00469-z
23. Zhang L, Schickhardt S, Auffarth GU. An experimental laboratory study using the miyake-apple posterior view technique to investigate the dynamics between capsular bags and different IOL models. J Refract Surg. 2022;38(10):654–660. doi:10.3928/1081597X-20220825-01
24. Hernández-Martínez A, Díaz-Del-Rio MA, Ruiz-Santos M, Ruiz-Mesa R, Tañá-Rivero P. Refractive and visual outcomes of a monofocal non-constant aberration aspheric intraocular lens. Clin Ophthalmol. 2022;16:2521–2530. doi:10.2147/OPTH.S373587
25. McAlinden C, Gothwal VK, Khadka J, Wright TA, Lamoureux EL, Pesudovs K. A head-to-head comparison of 16 cataract surgery outcome questionnaires. Ophthalmology. 2011;118(12):2374–2381. doi:10.1016/j.ophtha.2011.06.008
26. Khadka J, McAlinden C, Pesudovs K. Quality assessment of ophthalmic questionnaires: review and recommendations. Optom Vis Sci. 2013;90(8):720–744. doi:10.1097/OPX.0000000000000001
27. Kabanovski A, Hatch W, Chaudhary V, et al. Validation and application of Catquest-9SF in various populations: a systematic review. Surv Ophthalmol. 2020;65(3):348–360. doi:10.1016/j.survophthal.2019.12.002
28. Mahmud I, Kelley T, Stowell C, et al. A proposed minimum set of outcome measures for cataract surgery. JAMA Ophthalmol. 2015;133(11):1247–1252. doi:10.1001/jamaophthalmol.2015.2810
29. Lundström M, Barry P, Brocato L, et al. European registry for quality improvement in cataract surgery. Int J Health Care Qual Assur. 2014;27(2):140–151. doi:10.1108/IJHCQA-10-2012-0101
30. Vasavada AR, Trivedi RH. Posterior capsule striae. J Cataract Refract Surg. 1999;25(11):1527–1531. doi:10.1016/S0886-3350(99)00197-2
31. Joshi RS. Postoperative posterior capsular striae and the posterior capsular opacification in patients implanted with two types of intraocular lens material. Indian J Ophthalmol. 2017;65(6):466–471. doi:10.4103/ijo.IJO_344_16
32. Ashena Z, Gallagher S, Nanavaty M Maddox rod effect due to aberrations from posterior capsule striae in a pseudophakic patient. Presented at the European Society of Cataract & Refractive Surgeons annual meeting; 2020. Available from: https://www.escrs.org/amsterdam2020/Programme/interactive-casereports-details.asp?id=37691.
33. Bozukova D, Werner L, Mamalis N, et al. Double-C loop platform in combination with hydrophobic and hydrophilic acrylic intraocular lens materials. J Cataract Refract Surg. 2015;41(7):1490–1502. doi:10.1016/j.jcrs.2014.10.042
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


