Back to Journals » Open Access Emergency Medicine » Volume 8
Clinical outcomes of 3-year experience of targeted temperature management in patients with out-of-hospital cardiac arrest at Songklanagarind Hospital in Southern Thailand: an analysis of the MICU-TTM registry
Authors Vattanavanit V , Bhurayanontachai R
Received 20 May 2016
Accepted for publication 2 August 2016
Published 6 September 2016 Volume 2016:8 Pages 67—72
DOI https://doi.org/10.2147/OAEM.S113214
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Hans-Christoph Pape
Veerapong Vattanavanit, Rungsun Bhurayanontachai
Division of Critical Care Medicine, Department of Internal Medicine, Faculty of Medicine, Prince of Songkla University, Hat Yai, Songkhla, Thailand
Background: Out-of-hospital cardiac arrest (OHCA) is one of the leading causes of intensive care unit admission, which results in high hospital mortality. Targeted temperature management (TTM) was introduced several years ago and is considered to improve neurological and mortality outcomes. This management process was implemented in our hospital in 2012, which was expected to improve the standard of care in OHCA patients.
Purpose: We aimed to report the clinical and mortality outcomes after TTM was introduced to our hospital in 2012.
Patients and methods: An analysis of data from the Medical Intensive Care Unit-TTM registry between 2012 and 2015 was performed. After successful cardiopulmonary resuscitation, TTM was applied to all OHCA patients regardless of causes if there was no contraindication. The Cerebral Performance Category scale score and other clinical outcomes were recorded and analyzed.
Results: Out of 23 patients, 87% were male and the mean age was 54.5±18.1 years. The causes of OHCA from cardiac etiology comprised 52.2%. The most common initial cardiac rhythm was ventricular fibrillation (47.8%). The survival rate to hospital discharge was 47.8% (11/23), but neurological outcomes were in a persistent vegetative state (8/11, 72.7%). The group with poor neurological outcomes had a significantly higher Acute Physiologic Assessment and Chronic Health Evaluation II score than the group with good neurological outcomes (22.9±4.2 vs 16.0±3.6, P=0.01). In the multivariate analysis, initial shockable rhythm was associated with survival at hospital discharge (odds ratio 10.1, 95% confidence interval 1.1–94.3, P=0.04).
Conclusion: TTM in OHCA patients gave better mortality benefits compared to our previous records, despite poor neurological outcomes. Ventilator-associated pneumonia was the major complication of TTM. Therefore, TTM should be considered in OHCA patients, especially in shockable rhythms, after return of spontaneous circulation.
Keywords: out-of-hospital cardiac arrest, targeted temperature management
Introduction
Cardiac arrest is a crucial medical emergency. The annual incidence was ~132/100,000 in the US population.1 Although we currently have new technology to support postcardiac arrest patients, the survival rate to hospital discharge is quite low in the range of 0.5%–8.5%.2 Previous studies have reported that factors that influenced mortality included patient status, shockable rhythm, witnessed cardiac arrest, bystander cardiopulmonary resuscitation (CPR), and also targeted temperature management (TTM).3–5
TTM was introduced as part of the postcardiac arrest care bundle for out-of-hospital cardiac arrest (OHCA) patients, because this measurement potentially improved Cerebral Performance Category (CPC) scale score and survival rates to hospital discharge.6,7 From our previous report, the survival rate of OHCA patients before the implementation of TTM was only 8.2%.8
Songklanagarind Hospital is the biggest tertiary university hospital in Southern Thailand. Our hospital implemented TTM for postcardiac arrest care in 2012. Although the major benefits of TTM are in cardiac arrest patients from cardiac origins, our hospital protocol intentionally introduced TTM in every OHCA patient after obtaining return of spontaneous circulation (ROSC). However, the clinical and neurological outcomes remain unclear. Therefore, we aimed to evaluate the clinical and neurological outcomes of our treatment protocol and identify factors influencing survival to hospital discharge in OHCA patients within our institute.
Patients and methods
Study design
This study was a secondary analysis from the Medical Intensive Care Unit (MICU)-TTM registry between November 2012 and November 2015. The MICU-TTM registry is a local database of the TTM protocol in our MICU of every adult OHCA patient who obtained ROSC and was admitted to the MICU for postcardiac arrest care. All demographic data, medical history, and CPR details along with clinical and neurological outcomes were recorded in the registry. The protocol of this study was approved by the ethics committee of the Faculty of Medicine, Prince of Songkla University (EC number: 59-085-14-1). A waiver of consent was approved for inclusion in this study, and the investigators signed a confidentially agreement.
TTM protocol
The postcardiac arrest committee of Songklanagarind Hospital launched a TTM protocol in October 2012. The eligible criteria for TTM in OHCA patients are adult patients (age ≥18 years) who obtained ROSC with unconsciousness (a score of <8 on the Glasgow Coma Scale [on which scores range from 3 to 15, with lower scores representing reduced levels of consciousness]), any initial electrocardiographic rhythms, and no contraindication for hypothermia.9
After informed consent was received from a patient’s next of kin, 1 L of cold saline was intravenously infused. Subsequently, a surface cooling device was applied to rapidly induce the body temperature to 33°C and maintained the target temperature during the maintenance phase for 24 hours. The Arctic Sun® machine (Medivance Inc, Louisville, CO, USA) is the standard surface cooling machine in our unit. Core temperatures were measured by an esophageal temperature probe. Patients were then rewarmed to 37°C with a rate of 0.25°C/h and maintained at this temperature for further 48 hours. Cardiovascular, respiratory, and electroencephalogram (EEG) monitoring and serial blood tests were strictly performed according to our unit protocol. Other medical managements (ie, primary coronary intervention, infusion of intravenous thrombolytic agents, and renal replacement therapy) depended on the decision of the intensivists in charge.
Data collection
Demographic data included sex, age, medical history, characteristics of the cardiac arrest, location of the cardiac arrest, bystander-witnessed cardiac arrest, bystander CPR, first monitored electrocardiographic rhythm, time from cardiac arrest to event, CPR time, number of defibrillations, adrenaline dose, and causes of cardiac arrest. Data on clinical characteristics of the patients on admission were first measured body temperature, Glasgow Coma Scale score, presence of corneal reflex and papillary reflex, serum pH and lactate, presence of circulatory shock defined as a systolic blood pressure of ≤ 90 mmHg for >30 minutes or end-organ hypoperfusion (ie, cool extremities, a urine output of <30 mL/h, and a heart rate of <60 beats per minute), ST segment elevation myocardial infarction, and the Acute Physiologic Assessment and Chronic Health Evaluation II (APACHE II) score.
The therapeutic hypothermia process included time from ROSC until TTM was initiated, phases of TTM, and the patient’s body temperature at 24 hours, 48 hours, and 72 hours. We also recorded serious TTM complications and in-hospital complications. Procedures performed during admission were also recorded.
Outcomes
The primary outcomes evaluated were mortality and neurological outcomes after TTM. A mortality outcome was classified as “survivor” if the patient was discharged alive from the hospital and “nonsurvivor” if the patient died in the hospital. Neurological outcomes were defined according to the CPC scale10,11 and the modified Rankin Scale.12,13 Poor neurological outcomes were classified if the CPC scale score at discharge was >2. The CPC scores ranged from 1 to 5, with 1 representing good cerebral performance or minor disability, 2 representing moderate cerebral disability (function is sufficient for independent activity of daily life), 3 representing severe cerebral disability, 4 representing coma or vegetative state, and 5 representing brain death. Scores on the modified Rankin Scale ranged from 0 to 6, with 0 representing no symptoms, 1 representing no clinically significant disability despite some symptoms, 2 representing slight disability (patient is able to look after their own affairs without assistance), 3 representing moderate disability (patient requires some help but is able to walk unassisted), 4 representing moderately severe disability (patient is unable to attend to their own bodily needs), 5 representing severe disability (patient is bedridden), and 6 representing death.
Another objective was to identify factors influencing poor clinical and neurological outcomes after TTM.
Statistical analysis
Categorical data were demonstrated as percentages. Continuous data were shown as mean ± standard deviation, or median (with minimum and maximum, interquartile range), depending on the distribution of the data. The data were tested for normality using the Kolmogorov–Smirnov goodness-of-fit test. For the primary outcomes, the chi-square test or Fisher’s exact test was performed for categorical data. Student’s t-test or Mann–Whitney U test was selected for continuous variable analysis. Selected variables with P<0.1 were introduced to a multiple logistic regression model. Odds ratios and their 95% confidence intervals were used to identify the significant independent influencing factors to mortality and poor neurological outcomes after TTM. Two-tailed values of P<0.05 were deemed statistically significant. All statistical analyses were computed with the SPSS® statistical package version 16 (SPSS Inc., Chicago, IL, USA).
Results
Patients
A total of 23 OHCA patients were enrolled from November 2012 to November 2015 for TTM (Figure 1). The mean age was 54.5 years. Almost all the patients were males and developed cardiac arrest at home with a witness, but only 17.4% were resuscitated by witnesses. The most frequent rhythm was ventricular fibrillation and cause of arrest was predominantly of cardiac origin. The mean CPR time was 21 minutes (Table 1).
  | Figure 1 Patients treated with TTM. Abbreviations: OHCA, out-of-hospital cardiac arrest; TTM, targeted temperature management; IHCA, in-hospital cardiac arrest. |
In ROSC patients, the mean core temperature at the time of ICU admission was 36.8°C. Almost all of the patients were shocked, had metabolic acidosis, and were comatose. The mean APACHE II score was 21.
TTM process
The TTM process was performed initially at the MICU. The mean time from ROSC to the start of TTM was 4.39 hours. Patients were induced with cold saline, or cold gastric lavage. The temperature was managed with a surface cooling system (Arctic Sun®) in all patients. The durations of induction, maintenance, and rewarm phase were 3 hours, 24 hours, and 8 hours, respectively.
Complications of TTM occurred in only 13% of the patients. The most common complications were cardiac arrhythmias and hypotension. In-hospital complications occurred in 87% of the patients; the most common complication was ventilator-associated pneumonia. Coronary angiography and percutaneous coronary intervention were performed only in 21.7% and 13% of the patients, respectively. EEG was performed in the intensive care unit in 34.8% of the patients (Table 2).
Primary outcomes
Regarding the outcome of postcardiac arrest patients treated with TTM, survival until hospital discharge was 47.8%, but only 13% had a good neurological outcome (CPC 1–2). Most patients were in a vegetative state. The mortality rate was 52.2%. The most common cause of death was multiple organ failure (Table 3). In patients with shockable and nonshockable rhythms, the survivors were 73% and 27% (P=0.04 as per Fisher’s exact test) and good neurological outcomes were 27% and 0% (P=0.9), respectively.
Secondary outcomes
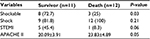
Survival patients had shockable rhythms and low APACHE II scores compared with the nonsurvival patients.
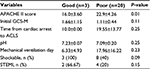
In multivariate analysis, initial shockable rhythm was positively associated with survival at hospital discharge (odds ratio 10.1, 95% confidence interval 1.1–94.3, P=0.04). The group with poor neurological outcomes had a significantly higher APACHE II score than the group with good neurological outcomes (22.9±4.2 vs 16.0±3.6, P=0.01) (Tables 4 and 5).
Discussion
The results of TTM projected in OHCA patients in our institute revealed that the survival rate until discharge was 47.8%, but only 13% obtained a good neurological outcome.
After two randomized controlled studies were reported,6,7 TTM was recommended in the international CPR guidelines.4 TTM showed benefits in decreasing mortality and improving the neurological outcomes in comatose OHCA patients.
When compared with the pre-TTM era, the survival rate and neurological outcome (CPC 1–2) in our institute improved (8.2% vs 47.8% and 4.1% vs 13%, respectively),8 but other sites had better survival rates (50%–52%) as well as better neurological outcomes (47%).14 The first reason may be that we included nonshockable and shockable rhythm patients to perform TTM. Since shockable rhythm has a better prognosis than nonshockable rhythm,15–18 one randomized clinical trial and one quasirandomized clinical trial restricted the inclusion criteria to only patients with shockable rhythm.6,7 Second, our patients spent a long time in cardiac arrest and had a low number of bystander CPRs when compared with other studies.6,7,14 Third, although the leading cause of arrest was cardiac in origin, the rate of percutaneous coronary intervention in our institute was quite low. In a study of coronary angiography in postcardiac arrest patients with suspected cardiovascular cause, a coronary artery lesion was found in 96% of patients with ST elevation and in 58% of patients without ST elevation.19 Some studies showed the benefits in early coronary angiography in patients with a presumed cardiac cause whether ST elevation or not.15,16 Finally, many patients had high core temperatures after 72 hours after the rewarming phase. Rebound fever was associated with mortality.20 However, some studies did not show an association with rebound fever and neurological outcomes, or survival rate until discharge.18,19
This study showed that TTM could be performed with minor complications in our center. However, a large number of patients had ventilator-associated pneumonia, which is similar to other TTM studies.6,7,14 We also found that 30.4% of patients had status epilepticus after cardiac arrest in spite of the fact that continuous EEG monitoring was done in only 34.8% of the patients. Malignant EEG patterns are common in comatose postcardiac arrest patients.21 The benefits from the treatment of electroencephalographic status epilepticus after CPR may come from an ongoing trail.22
Regarding the strength of the study, this study is the largest report of TTM among the tertiary hospitals in Thailand. The results of this TTM project are important to improve the process of care in our institute and in the country.
Our study had several limitations. First, it was a small retrospective study at a single center. Second, we did not perform long-term follow-up in the survival patients. Furthermore, the 3-year period of the study was quite short; hence, we had data from a small number of patients.
The results of this study suggest that we have to improve both the knowledge of people attempting bystander CPR and the referral system to minimize delay time to the hospitals. TTM should be conducted at the emergency department as quickly as possible, and controlling the temperature after rewarming is crucial since it is associated with survival outcomes.
Conclusion
In this study, TTM in OHCA patients demonstrated better mortality benefits compared to pre-TTM implementation despite the poor neurological outcomes. Ventilator-associated pneumonia was the major complication of TTM. Nevertheless, TTM should be considered in OHCA patients, especially in shockable rhythms after obtaining ROSC.
Acknowledgment
This study was fully funded by the Faculty of Medicine, Prince of Songkla University, Hat Yai, Songkhla, Thailand.
Author contributions
All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Mozaffarian D, Benjamin EJ, Go AS, et al; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics – 2015 update: a report from the American Heart Association. Circulation. 2015;131(4):e29–e322. | ||
Ong ME, Shin SD, De Souza NN, et al; PAROS Clinical Research Network. Outcomes for out-of-hospital cardiac arrests across 7 countries in Asia: the Pan Asian Resuscitation Outcomes Study (PAROS). Resuscitation. 2015;96:100–108. | ||
Yeeheng U. Factors associated with successful resuscitation of out-of-hospital cardiac arrest at Rajavithi Hospital’s Narenthorn Emergency Medical Service Center, Thailand. Asia Pac J Public Health. 2011;23(4):601–607. | ||
Callaway CW, Donnino MW, Fink EL, et al. Part 8: post-cardiac arrest care: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132(18 suppl 2):S465–S482. | ||
Sathianathan K, Tiruvoipati R, Vij S. Prognostic factors associated with hospital survival in comatose survivors of cardiac arrest. World J Crit Care Med. 2016;5(1):103–110. | ||
Bernard SA, Gray TW, Buist MD, et al. Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N Engl J Med. 2002;346(8):557–563. | ||
Hypothermia after Cardiac Arrest Study Group. Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med. 2002;346(8):549–556. | ||
Vattanavanit V, Bhurayanontachai R, Khwannimit B. Survival of out-of-hospital cardiac arrest patients and feasibility for therapeutic hypothermia. Songkla Med J. 2013;31(6):287–295. | ||
Jacobs I, Nadkarni V, Bahr J, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Councils of Southern Africa). Circulation. 2004;110(21):3385–3397. | ||
Jennett B, Bond M. Assessment of outcome after severe brain damage. Lancet. 1975;1(7905):480–484. | ||
[No authors listed]. Randomized clinical study of thiopental loading in comatose survivors of cardiac arrest. Brain Resuscitation Clinical Trial I Study Group. N Engl J Med. 1986;314(7):397–403. | ||
Rankin J. Cerebral vascular accidents in patients over the age of 60. II. Prognosis. Scott Med J. 1957;2(5):200–215. | ||
van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJ, van Gijn J. Interobserver agreement for the assessment of handicap in stroke patients. Stroke. 1988;19(5):604–607. | ||
Nielsen N, Wetterslev J, Cronberg T, et al; TTM Trial Investigators. Targeted temperature management at 33 degrees C versus 36 degrees C after cardiac arrest. N Engl J Med. 2013;369(23):2197–2206. | ||
Dumas F, Grimaldi D, Zuber B, et al. Is hypothermia after cardiac arrest effective in both shockable and nonshockable patients?: insights from a large registry. Circulation. 2011;123(8):877–886. | ||
Testori C, Sterz F, Behringer W, et al. Mild therapeutic hypothermia is associated with favourable outcome in patients after cardiac arrest with non-shockable rhythms. Resuscitation. 2011;82(9):1162–1167. | ||
Vaahersalo J, Hiltunen P, Tiainen M, et al. Therapeutic hypothermia after out-of-hospital cardiac arrest in Finnish intensive care units: the FINNRESUSCI study. Intensive Care Med. 2013;39(5):826–837. | ||
Mader TJ, Nathanson BH, Soares WE 3rd, Coute RA, McNally BF. Comparative effectiveness of therapeutic hypothermia after out-of-hospital cardiac arrest: insight from a large data registry. Ther Hypothermia Temp Manag. 2014;4(1):21–31. | ||
Spaulding CM, Joly LM, Rosenberg A, et al. Immediate coronary angiography in survivors of out-of-hospital cardiac arrest. N Engl J Med. 1997;336(23):1629–1633. | ||
Bro-Jeppesen J, Hassager C, Wanscher M, et al. Post-hypothermia fever is associated with increased mortality after out-of-hospital cardiac arrest. Resuscitation. 2013;84(12):1734–1740. | ||
Amorim E, Rittenberger JC, Baldwin ME, Callaway CW, Popescu A; Post Cardiac Arrest Service. Malignant EEG patterns in cardiac arrest patients treated with targeted temperature management who survive to hospital discharge. Resuscitation. 2015;90:127–132. | ||
Ruijter BJ, van Putten MJ, Horn J, et al; TELSTAR study group. Treatment of electroencephalographic status epilepticus after cardiopulmonary resuscitation (TELSTAR): study protocol for a randomized controlled trial. Trials. 2014;15:433. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.