Back to Journals » Clinical Ophthalmology » Volume 17
Clinical Outcomes After Bilateral Implantation of a Diffractive Trifocal Intraocular Lens: A Worldwide Pooled Analysis of Prospective Clinical Investigations
Authors Kohnen T , Lapid-Gortzak R, Ramamurthy D, Bissen-Miyajima H , Maxwell A, Kim TI, Modi S
Received 3 July 2022
Accepted for publication 21 November 2022
Published 10 January 2023 Volume 2023:17 Pages 155—163
DOI https://doi.org/10.2147/OPTH.S377234
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Video abstract of "Outcomes after bilateral implantation of a diffractive trifocal IOL" [ID 377234].
Views: 128
Thomas Kohnen,1 Ruth Lapid-Gortzak,2 Dandapani Ramamurthy,3 Hiroko Bissen-Miyajima,4 Andrew Maxwell,5 Tae-Im Kim,6 Satish Modi7
1Department of Ophthalmology, Goethe-University, Frankfurt, Germany; 2Department of Ophthalmology, Amsterdam University Medical Centers, Amsterdam, Netherlands; 3The Eye Foundation, Coimbatore, Tamil Nadu, India; 4Department of Ophthalmology, Tokyo Dental College Suidobashi Hospital, Tokyo, Japan; 5The California Eye Institute, Fresno, CA, USA; 6Department of Ophthalmology, Yonsei University College of Medicine, Seoul, South Korea; 7Seeta Eye Centers, Poughkeepsie, NY, USA
Correspondence: Thomas Kohnen, Department of Ophthalmology, Goethe University, Theodor‑Stern-Kai 7, Frankfurt, 60590, Germany, Tel +49 69 6301 6739/ 3945, Fax +49 69 6301 3893, Email [email protected]
Purpose: To investigate visual and safety outcomes of AcrySof® IQ PanOptix® (model TFNT00), a trifocal, presbyopia-correcting intraocular lens (IOL), in patients of different ethnicities across multiple countries, based on a pooled analysis of six prospective multicenter studies.
Patients and Methods: This pooled analysis included adult patients from six prospective clinical studies performed across 56 centers worldwide. After cataract removal by phacoemulsification, all patients were implanted with TFNT00; follow-up duration varied from 3 to 12 months according to the studies’ design. Binocular defocus curve; absolute manifest refraction spherical equivalent (MRSE); and binocular photopic uncorrected and corrected visual acuities at distance (UCDVA, BCDVA; 4– 5 m), intermediate (UCIVA, DCIVA; 60– 66 cm), and near (UCNVA, DCNVA; 40 cm) were measured.
Results: The study included 557 patients, 547 of whom were implanted bilaterally with the TFNT00 IOL (n = 1094 eyes). Binocular visual data at 1 month and 3– 6 months after implantation were available for up to 546 and 542 bilaterally implanted patients, respectively. A continuous range of 0.1 logarithm of the minimum angle of resolution (logMAR) or better vision from distance (0.00 diopter [D], 4– 5 m) to near (– 3.00 D; optically equivalent to 33 cm) was observed 3– 6 months after TFNT00 implantation. At 3– 6 months, 88.2% of first eyes achieved an MRSE ≤ 0.50 D and 88.7% of second eyes achieved an MRSE ≤ 0.50 D. Overall, 99.3%, 92.3%, and 94.6% of patients bilaterally implanted with TFNT00 achieved binocular photopic BCDVA, DCIVA, and DCNVA of 0.14 logMAR or better, respectively. Ocular adverse device effects and secondary surgical interventions (SSIs) were infrequent.
Conclusion: This global pooled analysis showed that TFNT00 provided a continuous range of 0.1 logMAR (~20/25 Snellen) or better vision from distance to 33 cm, with a low incidence of ocular adverse device effects and SSIs.
Keywords: PanOptix, intraocular lens, presbyopia, trifocal lens, diffractive lens, pooled analysis
Plain Language Summary
When patients undergo cataract surgery, the cloudy lens in the eye is removed and replaced with an artificial lens (known as an intraocular lens, IOL). Often, the implanted IOL is designed to provide good distance vision only, requiring patients to use spectacles for near and intermediate vision correction. Other lenses, so-called “trifocal” IOLs, create several distinct focal points for far, intermediate, and near viewing, to provide better vision at these working distances. One such trifocal lens is TFNT00, which is designed to provide patients with a continuous range of vision, helping to reduce the need for spectacles. Unlike other trifocal IOLs that target an intermediate focal point at 80 cm, TFNT00 has an intermediate focal point at 60 cm, which is a more comfortable distance for common intermediate visual activities like using a computer.
The purpose of this study was to evaluate the visual outcomes and safety of TFNT00 in patients of different ethnicities across multiple countries. This analysis was based on pooled clinical data from six studies including more than 500 patients worldwide. Results demonstrated that the TFNT00 trifocal IOL provides “20/25” or better vision from far to near (33 cm) working distances, with a good safety profile, independent of country or ethnicity.
Introduction
The current standard of care for the treatment of cataract is small-incision phacoemulsification followed by implantation of an intraocular lens (IOL).1,2 Monofocal IOLs are a common choice, but although they do provide good visual outcomes with few visual disturbances when their power is selected to correct vision at distance, additional near and intermediate correction with spectacles is usually still required.3,4 Multifocal IOLs were developed to correct presbyopia following cataract surgery at a range of distances, thereby increasing spectacle independence.3,4 Previous multifocal IOLs were bifocal, with two optical zones to improve near and distance vision.5,6 The increasing demand for a lens that provides good intermediate vision for tasks such as computer work led to the development of IOLs with a third focal point.6,7 The AcrySof® IQ PanOptix® IOL model TFNT00 (Alcon, Fort Worth, TX, USA) is a non-apodized, diffractive, trifocal, presbyopia-correcting IOL designed to provide a continuous range of vision from intermediate to near while preserving distance vision.8–10 TFNT00 is a single-piece, posterior-chamber, ultraviolet and blue light–filtering IOL with a biconvex optic and a central anterior multifocal optic diffractive structure.8–10 It uses proprietary ENLIGHTEN® optical technology to redistribute light from the first diffractive intermediate-order vision (120 cm) to the distance vision (refractive order), thereby enhancing the distance image quality.8,9,11 Moreover, TFNT00 has a +2.17 diopters (D) intermediate add power (second diffractive order) and +3.25 D near add power (third diffractive order) at the IOL plane, which translates to 1.64 D (~60 cm) and 2.35 D (~40 cm) at the corneal plane, respectively.8,9,11 Unlike most other trifocal IOLs incorporating sequential diffractive optics, TFNT00 intentionally provides an intermediate focal point at 60 cm (instead of 80 cm), because most intermediate-distance tasks are usually performed at 60–70 cm.7,12 This IOL has shown consistently positive visual outcomes after cataract surgery in numerous clinical trials worldwide, with low rates of serious and non-serious adverse events (AEs).7,13–17
This article presents the results of a pooled analysis of six prospective clinical studies investigating the visual outcomes and safety of TFNT00 after bilateral implantation in patients of different ethnicities across multiple countries.
Materials and Methods
Efficacy and safety data were pooled from six prospective clinical studies involving bilateral implantation of TFNT00 in adult patients with cataracts (N = 557), selected for inclusion in this publication as they represent all Alcon-sponsored investigations on TFNT00 conducted to date.7,13–17 Studies were conducted at 56 sites across Australia (7), Belgium (1), Brazil (3), Chile (3), Colombia (2), Denmark (2), France (1), Germany (2), India (5), Italy (2), Japan (2), Korea (4), Netherlands (2), Spain (5), United Kingdom (3) and United States of America (12).7,13–17
Phacoemulsification surgery was performed using clear corneal incisions, with all other procedures according to physician’s standard of care.7,13–17 The duration of patient follow-up varied from 3 to 12 months.7,13–17 All studies, conducted in accordance with the principles of the Declaration of Helsinki, were approved by appropriate Institutional Review Board or Ethics Committees, and all patients provided written informed consent before participation.7,13–17
Visual outcomes collected consistently across all six studies were selected for this analysis, including binocular defocus curve (ranging from +2.00 to –3.00 D, depending on the study); absolute manifest refraction spherical equivalent (MRSE); binocular photopic best-corrected distance visual acuity (BCDVA) and uncorrected distance visual acuity (UCDVA; 4–5 m); distance-corrected intermediate visual acuity (DCIVA) and uncorrected intermediate visual acuity (UCIVA; 60–66 cm); and distance-corrected near visual acuity (DCNVA) and uncorrected near visual acuity (UCNVA; 40 cm).7,13–17
The safety outcomes assessed in this pooled analysis were ocular adverse device effects (reported as AEs) and secondary surgical interventions (SSIs). If deemed to be AEs, ocular adverse device effects, including halo vision, glare, posterior capsule opacification, visual impairment, blurred vision, and lens extraction, were reported by the investigator across the full observation period for each study (ie, not at specific timepoints), when experienced in either the first or second operative eye, and coded using the Medical Dictionary for Regulatory Activities.
As patient-reported outcomes assessing visual disturbances or patient satisfaction were not included in all individual studies, nor were they standardized, they could not be pooled in this analysis.
Statistical Analyses
Since this was a pooled analysis of data on a single IOL model, no formal statistical hypothesis testing was planned. Therefore, data are summarized using descriptive statistics. Categorical data are presented as absolute numbers and percentages, whereas continuous data are presented using means, standard deviations (SD), and 95% confidence intervals. Due to variations in the available duration of outcomes between studies, and to provide the greatest sample size for this analysis, visual outcomes were pooled for the 3- and 6-month timepoints – an approach made possible by the refractive stability displayed by TFNT00 at the month 3 postoperative visit. The all-implanted set included all patients who underwent successful unilateral IOL implantation. Visual outcomes data were analyzed in patients who were implanted bilaterally with the TFNT00 IOL. Safety outcomes data were obtained using the safety analysis set, which included all patients who underwent attempted implantation, whether successful or aborted, where the IOL may have touched the eye.
Results
In total, 557 patients underwent TFNT00 implantation in the first eye. Among them, one patient underwent IOL exchange in the first, and only implanted, eye due to blurred vision;13 one patient withdrew from the study after implantation in the first eye and did not receive an IOL in the second eye;16 and eight patients received unilateral implantation only.14,15,17 Of the 547 patients who underwent TFNT00 bilateral implantation, 546 had at least 1 month of follow-up data for one of the endpoints presented.
Patient baseline demographics and characteristics are summarized in Table 1. Patients were predominantly female (63.9%), with a mean age of 65.3 years, and were predominantly either White (52.8%) or Asian (35.4%). Ethnicities by study and geographical region are presented in Figure 1. In the Asian population (N = 197), 68 (34.5%) were analyzed in the Japanese study, 44 (22.3%) in the Korean study, and 73 (37.1%) in the Indian study.
 |
Table 1 Patient Baseline Characteristics and Demographics (All-Implanted Analysis Set) |
 |
Figure 1 Ethnicity by study and geographical region. Data are from the following studies for (A) Modi S et al,14 (B) Kohnen T et al,13 (C) Lapid-Gortzak R et al,7 (D) Ramamurthy D et al,17 (E) Kim TI et al,16 (F) Bissen-Miyajima H et al.15 Abbreviations: UK, United Kingdom; US, United States. |
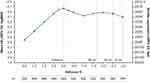
The mean binocular defocus curve at 3–6 months postoperatively is presented in Figure 2. TFNT00 implantation was shown to provide a continuous range 0.1 logarithm of the minimum angle of resolution (logMAR) or better vision from distance (0.00 D, 4–5 m) to near (–3.00 D, ~33 cm). At 0.00 D, –1.50 D (~66 cm), and –2.50 D (~40 cm), TFNT00-implanted patients achieved a mean visual acuity (VA) of 0.04 logMAR (~20/20−2 Snellen) or better. Additionally, at 3–6 months after implantation of TFNT00, an MRSE ≤0.50 D was achieved in 88.2% of first eyes and 88.7% of second eyes.
Corrected and uncorrected VA outcomes (mean ± SD) at 3–6 months and 1 month postoperatively are summarized in Figure 3. At 3 months after surgery, patients achieved a mean binocular BCDVA of –0.088±0.10 logMAR, with mean binocular DCIVA and DCNVA of –0.017±0.12 and 0.021±0.11 logMAR (Figure 3A), compared with –0.112±0.10 logMAR, –0.010±0.14 and –0.064±0.08 logMAR, respectively, at 1 month (Figure 3B). Binocular uncorrected VA results demonstrated a mean UCDVA of ≤0.00 logMAR and mean UCIVA and UCNVA of ≤0.06 logMAR at both 3–6 months and 1 month postoperatively (Figure 3C and D).
At 3–6 months, 99.3%, 92.3%, and 94.6% of patients bilaterally implanted with TFNT00 achieved binocular photopic BCDVA, DCIVA, and DCNVA of 0.14 logMAR or better, respectively (Figure 4A). Overall, >86% of patients achieved UCDVA, UCIVA, and UCNVA of 0.14 logMAR or better at 3–6 months (Figure 4B).
Ocular adverse device effects were reported by the investigator as detailed in the Methods section. These were infrequent following TFNT00 implantation, with halo vision and glare being reported in 2.2% and 1.1% of first eyes, respectively (Table 2). Of note, only four SSIs were required (Table 3): two explants in first eyes due to blurred vision or the patient being unsatisfied with the optical properties, and two in second eyes involving repositioning of the IOL.
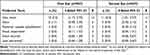 |
Table 2 Summary of Ocular Adverse Device Effects Associated with the IOL (Safety Analysis Set) |
 |
Table 3 Summary of IOL-Associated SSIs (Safety Analysis Set) |
Discussion
Results from this global pooled analysis of more than 500 patients showed that TFNT00 provided a 0.1 logMAR or better (~20/25 Snellen) VA from distance to 33cm, with a low incidence of ocular adverse device effects and SSIs. Unlike many multifocal IOLs, and even first-generation trifocal IOLs, TFNT00 provided ~0.0 logMAR intermediate vision at 60 cm, the distance associated with common activities such as viewing computer or laptop screens.7 In addition, the ~0.0 logMAR binocular vision at intermediate and near distances reported here supports the results of a recent study of TFNT00 on VA reserve, indicating an additional functional benefit for reading.18 The safety profile of TFNT00 with regard to visual disturbances (recorded as AEs) was favorable and consistent with other studies that demonstrate a low frequency of AEs and SSIs.7,9,19 Only the studies conducted in India and in Korea assessed patient-reported visual disturbances, focusing specifically on halo. In Ramamurthy et al the vast majority (86.6%) of Indian patients implanted with TFNT00 did not experience halos or did so “some of the time” 3 months postoperatively, with one individual reporting them as “severe”.17 By contrast, only 32% of Korean patients reported no or low frequency of halos within the same timeframe, with 14 instances being described as “severe”.16 Although a head-to-head comparison between the two studies cannot be made, it is of interest to note that patient-reported outcomes were assessed through different types of questionnaires, which may have contributed to the discrepancy observed.16
TFNT00 vision benefits were achieved in patients from multiple countries across Asia, Australia, Europe, South America, and United States of America indicating consistent efficacy across different ethnicities (eg, with potential for varying patient characteristics such as height and visual demands) and study centers (eg, potential slight local differences in surgical planning and implantation steps).
Although outcomes were broadly consistent with those reported in the individual studies, there were some differences. Of note, VA outcomes were better in the Japanese study compared with the overall pooled analysis population (mean BCDVA: –0.197±0.076 logMAR; DCIVA: –0.112±0.111 logMAR; DCNVA: –0.073±0.111 logMAR);15 this could be due to population/assessment center differences, or to a smaller sample size (N = 68), though error margins were broadly consistent.
This pooled analysis presents several limitations. First, non-toric TFNT00 IOLs were implanted in patients displaying up to 1.00 D of astigmatism, which may have limited the uncorrected VA improvements that could have been achieved, especially for patients with against-the-rule astigmatism. For this patient population, the toric TFNT00 IOL may provide better VA outcomes. Second, because non-standardized patient-reported outcomes were employed across the six studies, it was not possible to collate and discuss patient-reported visual disturbances or preferences to support the defocus and VA data.
Conclusion
This pooled analysis of six worldwide clinical trials shows that the TFNT00 trifocal IOL provides a continuous range of 0.1 logMAR (~20/25 Snellen) or better VA, from very near (33 cm) to distance (4–5 m), with peak performance at distance, 66 cm, and 40 cm, with a low incidence of ocular adverse device effects and SSIs, independent of country or patient ethnicity.
Abbreviations
AE, adverse event; BCDVA, best-corrected distance visual acuity; D, diopter; DCIVA, distance-corrected intermediate visual acuity; DCNVA, distance-corrected near visual acuity; IOL, intraocular lens; logMAR, logarithm of the minimum angle of resolution; MRSE, manifest refraction spherical equivalent; SD standard deviation; SSI, secondary surgical intervention; UCDVA, uncorrected distance visual acuity; UCIVA, uncorrected intermediate visual acuity; UCNVA, uncorrected near visual acuity; VA, visual acuity.
Data Sharing Statement
No further data beyond those provided in this manuscript will be shared.
Acknowledgments
The authors thank Chameleon Communications for editorial assistance in the preparation of the manuscript, with funding from Alcon Research LLC.
Author Contributions
All authors made substantial contributions to the conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agreed to be accountable for all aspects of the work.
Funding
This work was sponsored by Alcon Research LLC, Fort Worth, Texas. The sponsors participated in the design of the study, data management, data analysis, interpretation of the data, preparation, review, and approval of the manuscript.
Disclosure
Professor Kohnen, Dr Lapid-Gortzak, Professor Bissen-Miyajima and Dr Modi are consultants to, and have received grant support from, Alcon. Professor Kohnen is also consultant for Allergan, Bausch & Lomb, Geuder, Med Update, Santen, Staar, Thieme, Ziemer, and is a consultant, and conducts research for, Alcon/Novartis, Johnson & Johnson, Lensgen, Oculentis, Oculus, Presbia, Schwind, and Zeiss, outside the submitted work. Dr Lapid-Gortzak also reports grants and/or personal fees from CorNeat, Eye Yon Medical, Hanita Lenses, and Zeiss, outside the submitted work. Professor Bissen-Miyajima also reports grants and/or personal fees from Johnson and Johnson Vision, HOYA, Zeiss, and BVI, outside the submitted work. Dr Ramamurthy, Dr Maxwell, and Professor Kim are consultants to Alcon. The authors report no other conflicts of interest in this work.
References
1. Lundstrom M, Barry P, Henry Y, Rosen P, Stenevi U. Evidence-based guidelines for cataract surgery: guidelines based on data in the European Registry of Quality Outcomes for Cataract and Refractive Surgery database. J Cataract Refract Surg. 2012;38(6):1086–1093. doi:10.1016/j.jcrs.2012.03.006
2. Olson RJ, Braga-Mele R, Chen SH, et al. Cataract in the adult eye preferred practice pattern®. Ophthalmology. 2017;124(2):P1–P119. doi:10.1016/j.ophtha.2016.09.027
3. de Silva SR, Evans JR, Kirthi V, Ziaei M, Leyland M. Multifocal versus monofocal intraocular lenses after cataract extraction. Cochrane Database Syst Rev. 2016;12:CD003169. doi:10.1002/14651858.CD003169.pub4
4. Wang SY, Stem MS, Oren G, Shtein R, Lichter PR. Patient-centered and visual quality outcomes of premium cataract surgery: a systematic review. Eur J Ophthalmol. 2017;27(4):387–401. doi:10.5301/ejo.5000978
5. Kohnen T, Allen D, Boureau C, et al. European multicenter study of the AcrySof ReSTOR apodized diffractive intraocular lens. Ophthalmology. 2006;113(4):578–584. doi:10.1016/j.ophtha.2005.11.020
6. Gatinel D, Houbrechts Y. Comparison of bifocal and trifocal diffractive and refractive intraocular lenses using an optical bench. J Cataract Refract Surg. 2013;39(7):1093–1099. doi:10.1016/j.jcrs.2013.01.048
7. Lapid-Gortzak R, Bhatt U, Sanchez JG, et al. Multicenter visual outcomes comparison of 2 trifocal presbyopia-correcting IOLs: 6-month postoperative results. J Cataract Refract Surg. 2020;46(11):1534–1542. doi:10.1097/j.jcrs.0000000000000274
8. Kohnen T, Herzog M, Hemkeppler E, et al. Visual performance of a quadrifocal (trifocal) intraocular lens following removal of the crystalline lens. Am J Ophthalmol. 2017;184:52–62. doi:10.1016/j.ajo.2017.09.016
9. Carson D, Xu Z, Alexander E, Choi M, Zhao Z, Hong X. Optical bench performance of 3 trifocal intraocular lenses. J Cataract Refract Surg. 2016;42(9):1361–1367. doi:10.1016/j.jcrs.2016.06.036
10. Sudhir RR, Dey A, Bhattacharrya S, Bahulayan A. AcrySof IQ PanOptix intraocular lens versus extended depth of focus intraocular lens and trifocal intraocular lens: a clinical overview. Asia Pac J Ophthalmol (Phila). 2019;8(4):335–349. doi:10.1097/APO.0000000000000253
11. Gundersen KG, Potvin R. Trifocal intraocular lenses: a comparison of the visual performance and quality of vision provided by two different lens designs. Clin Ophthalmol. 2017;11:1081–1087. doi:10.2147/OPTH.S136164
12. Kohnen T. First implantation of a diffractive quadrafocal (trifocal) intraocular lens. J Cataract Refract Surg. 2015;41(10):2330–2332. doi:10.1016/j.jcrs.2015.11.012
13. Kohnen T, Marchini G, Alfonso JF, et al. Innovative trifocal (quadrifocal) presbyopia-correcting IOLs: 1-year outcomes from an international multicenter study. J Cataract Refract Surg. 2020;46(8):1142–1148. doi:10.1097/j.jcrs.0000000000000232
14. Modi S, Lehmann R, Maxwell A, et al. Visual and patient-reported outcomes of a diffractive trifocal intraocular lens compared with those of a monofocal intraocular lens. Ophthalmology. 2021;128(2):197–207. doi:10.1016/j.ophtha.2020.07.015
15. Bissen-Miyajima H, Ota Y, Hayashi K, Igarashi C, Sasaki N. Results of a clinical evaluation of a trifocal intraocular lens in Japan. Jpn J Ophthalmol. 2020;64(2):140–149. doi:10.1007/s10384-019-00712-4
16. Kim TI, Chung TY, Kim MJ, Lee K, Hyon JY. Visual outcomes and safety after bilateral implantation of a trifocal presbyopia correcting intraocular lens in a Korean population: a prospective single-arm study. BMC Ophthalmol. 2020;20(1):288. doi:10.1186/s12886-020-01549-z
17. Ramamurthy D, Vasavada A, Padmanabhan P, et al. Clinical outcomes after bilateral implantation of a trifocal presbyopia-correcting intraocular lens in an Indian population. Clin Ophthalmol. 2021;15:213–225. doi:10.2147/OPTH.S279001
18. Lapid-Gortzak R, Bala C, Schwiegerling J, Suryakumar R. New methodology for measuring intraocular lens performance using acuity reserve. J Cataract Refract Surg. 2021;47(8):1006–1010. doi:10.1097/j.jcrs.0000000000000561
19. Cochener B, Boutillier G, Lamard M, Auberger-Zagnoli C. A comparative evaluation of a new generation of diffractive trifocal and extended depth of focus intraocular lenses. J Refract Surg. 2018;34(8):507–514. doi:10.3928/1081597X-20180530-02
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.