Back to Journals » Cancer Management and Research » Volume 9
Clinical implications of six inflammatory biomarkers as prognostic indicators in Ewing sarcoma
Authors Li YJ, Yang X, Zhang WB, Yi C, Wang F, Li P
Received 20 July 2017
Accepted for publication 30 August 2017
Published 28 September 2017 Volume 2017:9 Pages 443—451
DOI https://doi.org/10.2147/CMAR.S146827
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Antonella D'Anneo
Yong-Jiang Li, Xi Yang, Wen-Biao Zhang, Cheng Yi, Feng Wang, Ping Li
Department of Oncology, West China Hospital, Sichuan University, Chengdu, People’s Republic of China
Abstract: Cancer-related systemic inflammation responses have been correlated with cancer development and progression. The prognostic significance of several inflammatory indicators, including neutrophil–lymphocyte ratio (NLR), platelet–lymphocyte ratio (PLR), Glasgow Prognostic Score (GPS), C-reactive protein to albumin ratio (CRP/Alb ratio), lymphocyte–monocyte ratio (LMR), and neutrophil–platelet score (NPS), were found to be correlated with prognosis in several cancers. However, the prognostic role of these inflammatory biomarkers in Ewing sarcoma has not been evaluated. This study enrolled 122 Ewing patients. Receiver operating characteristic (ROC) analysis was generated to determine optimal cutoff values; areas under the curves (AUCs) were assessed to show the discriminatory ability of the biomarkers; Kaplan–Meier analysis was conducted to plot the survival curves; and Cox multivariate survival analysis was performed to identify independent prognostic factors. The optimal cutoff values of CRP/Alb ratio, NLR, PLR, and LMR were 0.225, 2.38, 131, and 4.41, respectively. CRP/Alb ratio had a significantly larger AUC than NLR, PLR, LMR, and NPS. Higher levels of CRP/Alb ratio (hazard ratio [HR] 2.41, P=0.005), GPS (HR 2.27, P=0.006), NLR (HR 2.07, P=0.013), and PLR (HR 1.85, P=0.032) were significantly correlated with poor prognosis. As the biomarkers had internal correlations, only the CRP/Alb ratio was involved in the multivariate Cox analysis and remained an independent prognostic indicator. The study demonstrated that CRP/Alb ratio, GPS, and NLR were effective prognostic indicators for patients with Ewing sarcoma, and the CRP/Alb ratio was the most robust prognostic indicator with a discriminatory ability superior to that of the other indicators; however, PLR, LMR, and NPS may not be suitable as prognostic indicators in Ewing sarcoma.
Keywords: Ewing sarcoma, inflammatory biomarkers, prognosis, survival, CRP/Alb ratio
Introduction
Ewing sarcoma is a highly aggressive malignant bone tumor that predominantly occurs during adolescence and young adulthood and is the second most common primary bone malignancy constituting approximately 34% of all primary bone cancers.1 With the introduction of multidisciplinary treatment methods, the 5-year overall survival rate approaches 55%–75%.1,2 Conventional prognostic indicators including presence of metastasis, tumor grade, tumor site, histological subtype, and Enneking stage have gradually exposed their inaccuracy and inadequacy in clinical practice.3 Identification of easily assessed and reliable prognostic factors could help us distinguish high-risk patients and allocate them the best therapy protocol, which may lead to further improvement of treatment outcomes.
Cancer-related inflammation has been recognized as the seventh hallmark of cancer, which is tightly linked to the genetic instability of cancer cells.4 In addition, the smoldering inflammation in the tumor microenvironment could contribute to cancer progression via promoting proliferation, angiogenesis, and metastasis; reducing response to hormones and chemotherapeutic agents; and subverting adaptive immunity.4,5 Targeting of inflammatory pathways has been indicated as a novel way to further enhance therapeutic efficacy.5,6 Because of the association between inflammation and cancer development, the prognostic significance of several inflammatory indicators that measure the state of systemic inflammation response has been suggested, including neutrophil–lymphocyte ratio (NLR), platelet–lymphocyte ratio (PLR), the Glasgow Prognostic Score (GPS), C-reactive protein to albumin ratio (CRP/Alb ratio), lymphocyte–monocyte ratio (LMR), and neutrophil–platelet score (NPS), and were found to be correlated with prognosis of several cancers such as breast, lung, gastric, and urinary tract cancers.7–10
However, the prognostic role of these inflammation-based biomarkers in patients with Ewing sarcoma has not been evaluated or reported. Besides, the prognostic significance of these six indicators has hardly been wholly assessed and compared in an individual study on a certain type of cancer. Thus, the current retrospective study was conducted to evaluate the prognostic significance of different inflammatory indicators (including NLR, PLR, GPS, CRP/Alb ratio, LMR, and NPS), identify possible prognostic factors, and compare their prognostic values in patients with Ewing sarcoma.
Patients and methods
The research protocol of this retrospective study was examined and approved by the institutional review board and the medical ethics committee of West China Hospital, Sichuan University. Written informed consent was obtained from all participants. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committees and with the principles of the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
We reviewed the electronic medical records of all patients with Ewing sarcoma enrolled in our hospital from June 2009 to November 2015. Patients were included in the study if the following criteria were met: 1) patients with pathologically confirmed Ewing sarcoma [pathological criteria mainly included: small blue cells with little intercellular matrix; CD99(+) and EWS/FLI1(+); LCA(−), CEA(−) and EMA(−)]; 2) did not receive any anticancer treatment before (chemotherapy, surgery, or radiotherapy); 3) with complete medical records and laboratory reports; and 4) with regular follow-up and the corresponding clinical data. The patients in the following conditions were excluded: 1) alive patients with follow-up less than 12 months; 2) patients with clinical evidence of infection or other inflammatory diseases before the first treatment; 3) patients with diseases that could affect inflammatory indicator values including abnormal thyroid function, atherosclerosis, cardiac events, and acute pancreatitis; 4) patients with records of nonsteroidal anti-inflammatory drugs (NSAIDs), angiotensin receptor blockers (ARBs), angiotensin-converting enzyme inhibitors (ACEIs), or statins treatments were also excluded because the drugs could also affect the results of blood test.
Two authors independently extracted clinical data of interest, and a Microsoft Excel sheet was designed to collect the following information: 1) details of patients and tumor including sex, age, tumor location, Enneking stage, presence of metastasis, and pathological fracture; 2) treatment methods including neoadjuvant or adjuvant chemotherapy (or radiotherapy) and surgical option (limb salvage or amputation); 3) outcome data including occurrence of local recurrence and metastasis, and survival time; and 4) laboratory test results including albumin, CRP, neutrophil count, platelet count, lymphocyte count, and monocyte count that were used to calculate CRP/Alb ratio, NLR, PLR, and LMR.
The CRP/Alb ratio was derived by dividing the CRP level by the albumin level; the NLR was derived by dividing the neutrophil count by the lymphocyte count; the PLR was derived by dividing the platelet count by the lymphocyte count; and the LMR was obtained by dividing the lymphocyte count by the monocyte count. The GPS was appointed by a combination of both CRP and Alb levels: patients with elevated levels of CRP (>10 mg/L) and reduced levels of Alb (≤35 g/L) were allocated a score of 2; those with only one of the biochemical abnormalities were allocated a score of 1; and those with neither of these abnormalities were allocated score 0. The NPS was calculated as follows: patients with neutrophils >7.5*109/L and platelets >400*109/L were scored 2; patients with only one of the abnormities were scored 1; and patients with neutrophils ≤7.5*109/L and platelets ≤400*109/L were scored 0.
Follow-up protocols were formulated and performed according to the National Comprehensive Cancer Network (NCCN) practice guidelines. The overall survival (OS), which is the main end-point, was calculated from the date of initial histological diagnosis to the date of latest follow-up of this study (March 2017) or death. Intervals of follow-up were every 3 months for the first 4 years, then every 6 months until the latest follow-up. Routine examinations of the follow-up included physical examination, radiographs of the surgical site, chest CT, and laboratory tests. Bone scans were performed every 6 months.
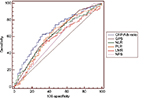
Statistical analyses were conducted using SPSS Statistics version 22.0 (IBM Corp., Chicago). Differences in groups were compared by the chi-square test. Receiver operating characteristic (ROC) analyses were performed with OS as end-point, and the optimal cutoff values for continuous prognostic variables (CRP/Alb, NLR, PLR, and LMR) were determined at the point of the maximal Youden index.11,12 The survival curves were generated using Kaplan–Meier analysis, and evaluated by log-rank test. Univariate and multivariate analyses were performed by using the Cox Regression Model to determine independent prognostic factors. Areas under the curve (AUCs) of the ROCs were calculated and compared by Z test to evaluate the discriminatory ability of the inflammation-based prognostic variables.13,14 All the statistical analyses were considered significant at two-tailed P<0.05. In addition, it needs to mention that, because these inflammatory indicators have internal correlations, only the indicator with the best discriminatory ability was incorporated in the multivariate analysis.
Results
Characteristics of patients and optimal cutoff values of inflammation-based variables
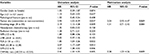
The clinicopathological characteristics of these patients are presented in Table 1. A total of 122 consecutive patients who met the inclusion and exclusion criteria were enrolled in the current study, including 70 male patients and 52 female patients. The median age was 21 years, and the majority of the tumors were located in extremities (89.3%); 105 patients were in Enneking stages I and II (86.1%), and the rest 17 patients were in the stage III (13.9%). Pathological fracture was presented in nine patients (7.3%). The neoadjuvant chemotherapy was given in 95 patients (77.9%), and all enrolled patients received adjuvant chemotherapy after surgery. Radiotherapy was given in 43 patients (35.2%).
The optimal cutoff value for CRP/Alb ratio was calculated to be 0.225 with the Youden index of 0.308, and the optical cutoff value for NLR was 2.38 (Youden index, 0.225). For PLR and LMR, the optical cutoff values were 131 (Youden index 0.212) and 4.41 (Youden index 0.185), respectively. The clinicopathological characteristics of the patients grouped by CRP/Alb ratio was presented in Table 1. The CRP/Alb ratio was found to be correlated with body mass index (BMI, P=0.037) and other inflammatory indicators (NLR, P=0.008; PLR, P=0.010; GPS, P<0.001; LMR, P=0.032), except for the NPS (P=0.056).
ROC curves of inflammation-based variables
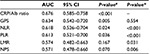
The ROC curves were generated for the survival status to evaluate the discriminatory ability of these inflammatory indicators (Figure 1). As shown in Table 2, the AUC was 0.676 (95% confidence interval [CI] 0.585–0.758) for CRP/Alb ratio, 0.634 (95% CI 0.542–0.720) for GPS, 0.618 (95% CI 0.526–0.704) for NLR, 0.613 (95% CI 0.521–0.700) for PLR, 0.574 (95% CI 0.482–0.663) for LMR, and 0.571 (95% CI 0.478–0.660) for NPS. The CRP/Alb ratio had significantly higher AUC values compared with NLR (P<0.001), PLR (P<0.001), LMR (P=0.031), and NPS (P=0.006) (Table 2).
Survival analysis
The median OS of all cohorts was 35 months, and 75 (61.5%) patients were alive at the end of the study follow-up. Survival curves revealed that patients with lower CRP/Alb ratio had significantly better survival than patients with higher CRP/Alb ratio (P=0.005, Figure 2A). Similar results were also observed when patients were grouped by GPS (P=0.006, Figure 2B), NLR (P=0.013, Figure 2C), and PLR (P=0.032, Figure 2D). The values of LMR (P=0.165, Figure 2E) and NPS (P=0.103, Figure 2F) were not significantly associated with patient survival.
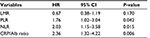
Results of univariate and multivariate analyses are presented in Table 3. The univariate analysis revealed that variables associated with better OS included tumor site (HR 2.94, 95% CI 1.03–8.39; P=0.037), Enneking stage (HR 2.19, 95% CI 1.12–4.28; P=0.009), and the inflammation-based indicators including PLR (HR 1.85, 95% CI 1.04–3.26; P=0.032), NLR (HR 2.07, 95% CI 1.17–3.69; P=0.013), GPS (HR 2.27, 95% CI 1.28–4.02; P=0.006), and CRP/Alb ratio (HR 2.41, 95% CI 1.33–4.35; P=0.005). Because the inflammatory indicators of CRP/Alb ratio, NLR, PLR, and GPS have correlations, only the CRP/Alb ratio was incorporated in the multivariate analysis. The multivariate analysis demonstrated that the CRP/Alb ratio (HR 2.28; 95% CI 1.23–4.26; P=0.009) remained an independent prognostic factor for better OS.
Finally, as we utilized the optimal cutoff values derived from the ROC analysis for the continuous variables (CRP/Alb, NLR, PLR, and LMR) in the survival analysis, we additionally used the median values of these inflammatory indicators to test the stability of the results, presented in Table 4. The results showed that the CRP/Alb, NLR, PLR, and LMR were still significantly correlated with unfavorable survival of the patients when utilizing the median values as the cutoff values, which indicated that the significance may not be sensitive to the cutoff values.
Discussion
The prognostic values of the inflammatory indicators in Ewing sarcoma were, to our knowledge, initially evaluated and compared in the current retrospective study based on individual data from 122 patients. Our findings demonstrated that CRP/Alb ratio, GPS, NLR, and PLR were significantly correlated with survival of patients with Ewing sarcoma. In addition, the CRP/Alb ratio may have a discriminatory ability superior to the other indicators and remained as a novel and promising inflammatory prognostic factor.
The relationship between chronic inflammation and malignant tumor has been researched for decades, and it is increasingly recognized that the systemic inflammatory response plays a crucial role in cancer development and progression.4,5 Mechanisms for the inflammatory response in cancer have been proposed. The growth and invasion of tumor cells would lead to tissue necrosis, hypoxia, and local damage, which disrupts the homeostasis and activates acute-phase responses.15,16 Then, tumor cells and/or tumor-associated leukocytes would release pro-inflammatory cytokines including interleukin (IL)-1, IL-6, IL-8, tumor necrosis factor (TNF), and vascular endothelial growth factor (VEGF).17–19 These inflammatory cytokines could promote tumor angiogenesis, growth, invasion, and metastasis; subvert adaptive immune response; and enhance the resistance to cytotoxic agents.20,21
CRP is an acute-phase reactant that is regulated by pro-inflammatory cytokines, especially IL-6. The presence of systemic inflammatory status in cancer, reflected by elevated CRP level, often accompanies decreased serum albumin concentration, with lean tissue breakdown and continuous weight loss, resulting in impaired nutritional status and increased mortality.19,22 Indeed, elevated CRP levels were found to be associated with poor survival of patients with bone sarcomas.23 In addition, neutrophils interact with tumor cells via secretion of cytokines and promoting tumor development.24,25 Lymphocytes play a crucial role in mediating immunological destruction of cancer cells, and lymphocytopenia indicates impairment of the host immune response to tumor.26,27 Monocytes could exert protumoral activities, including promotion of metastasis, immunosuppression, and angiogenesis mainly attributable to tumor-associated macrophages (TAMs).28,29 Platelets were also reported to serve as chemoattractants, contributing to migration of tumor cells.30,31 These inflammatory theoretic backgrounds lead to the emergence of several inflammation-based prognostic indicators in patients with cancer.
The most commonly used inflammatory indicators are the NLR and GPS; however, these two biomarkers are nonspecific. Old age and diseases including atherosclerosis, cardiac events, strokes, abnormal thyroid function, and acute pancreatitis could lead to an increase of biomarker values.32 In addition, the values could also be affected by various drugs such as ARBs, ACEIs, and statins.33 This emphasizes the importance of comorbidities correction or exclusion, which is often absent in previous reports on inflammatory markers. In the current study, those risks of bias were well-avoided. Different from other cancers that primarily afflicted the old, Ewing sarcoma predominantly occurred in adolescents and young adults, and the median age was only 21 in our cohort. As a result, the aforementioned diseases and drug administration could be largely avoided in these patients. Besides, factors that may lead to biases were excluded during inclusion of the patients, which could enable the current study to obtain accurate results.
First, ROC curve analysis was conducted to assess and compare the discriminatory ability of the inflammatory indicators, which has been validated in previous studies.13,14 The CRP/Alb ratio was observed to have the highest AUC value, followed by GPS and NLR. LMR and NPS have the lowest AUC values, and the P-values of the two indicators did not reach statistical significance, suggesting that LMR and NPS may not be suitable for use in Ewing sarcoma. The following Z test showed that the AUC value of CRP/Alb was significantly higher than that of NLR, PLR, LMR, and NPS, indicating the superior discriminatory ability of CRP/Alb ratio in terms of prognosis among patients with Ewing sarcoma. Moreover, as the CRP/Alb ratio and GPS are based on two protein components, and other indicators such as NLR, PLR, and LMR are based on two cellular components, the results suggested that the parameters of inflammation-related protein may be more reliable than those of cellular parameters in predicting prognosis in patients with Ewing sarcoma.
The cutoff values of the indicators were determined by the ROC curves based on the highest Youden index.11,12 Patients were grouped by the cutoff values and survival analyses were conducted. Because only a small proportion of patients have two points of GPS and NPS, patients with scores of 1 and 2 were grouped together when calculating HR values, thus achieving a more appropriate statistical analysis. In the univariate analysis, the higher values of CRP/Alb ratio, GPS, NLR, and PLR were correlated with unfavorable prognosis. The lower LMR value and higher NPS score were not found to have significant prognostic values – only a tendency toward poor survival could be observed. The relative poor prognostic ability of LMR and NPS in patients with Ewing sarcoma may partially explain the insignificance.
Because these inflammatory indicators have intrinsic correlations, only the CRP/Alb ratio – which had the highest theoretical discriminatory ability detected by the ROC analysis – was involved in the multivariate analysis, and remained an independent prognostic factor in the test. The CRP/Alb ratio is a relatively novel indicator derived from GPS. Instead of being stratified into only three scores (0, 1, and 2) as with GPS, the CRP/Alb ratio is calculated in a quantitative ratio with a continuous range of values. In the current study, higher values of HR for the CRP/Alb ratio indicated a superior prognostic effect compared with GPS, suggesting that the CRP/Alb in the form of a continuous variable may be able to theoretically better utilize the values of CRP and albumin.
The tumor site was identified as a prognostic indicator in the univariate analysis, and this is possibly due to the fact that the site of origin could critically influence chances for radical surgery, which could influence treatment outcomes and survival. The Enneking stage was also associated with a poor prognosis in the univariate analysis, but we did not identify it as an independent prognostic factor in the cohort. Compared with these prognostic indicators, these inflammatory biomarkers have advantages of being simple, easily available, economical, objective, and reproducible and could be measured at the beginning or early stage of treatment and monitored throughout the entire therapy periods. As a result, these biomarkers are potentially easy and worthy of being promoted in the management of patients with Ewing sarcoma, which could assist doctors in prognosis estimation and clinical decision-making at a relatively low cost. In addition, although parameters of inflammation-related proteins including CPR/Alb ratio and GPS exhibited more reliable features than the cellular parameters in the study, the two categories of indicators are actually not mutually incompatible. The complementary combination of CRP/Alb ratio with NLR and PLR could form a more complex model, which may provide firmer prognostic information for clinicians. Whether these inflammatory indicators could be incorporated into the stratification system of cancer patients to instruct individual treatment needs to be clarified in future prospective studies.
Last, it needs to be noted that higher values of CRP/Alb ratio were found to be correlated with lower BMI levels in the cohort. The finding supports the view that cancer-related systemic inflammation often accompanies an elevation of the overall consumption status of the body. As a biomarker based on two protein components of the body, the CRP/Alb ratio may not only be an inflammatory indicator but also remain a marker reflecting the nutritional status of patients with cancer. There have been studies using nutritional supplements to alter the inflammatory and nutritional status of patients with cancer, and improve their immune function.34,35 The application of inflammatory biomarkers in evaluating the overall inflammatory and trophic status of patients with cancer and assisting the nutritional support therapy may be a promising way ahead for future relevant researches.
A potential limitation of the current study is that it is a retrospective, single-center study. Although the patient samples were relatively large among studies of patients with Ewing sarcoma, and the multivariate analysis was conducted to reduce the bias, the study was restricted by its retrospective and single-center design. First, due to the retrospective design, the factor of response to chemotherapy could not be evaluated in the survival analysis because data were missing for some patients and could not be obtained retrospectively. Second, although relative strict inclusion standards were adopted to enable a similar background condition, heterogeneity still existed in the treatment of these patients, which may bring potential bias to the results. Thus, the results of the current study should be interpreted with caution and need to be validated by future multicenter prospective studies.
Conclusion
Our findings demonstrated that CRP/Alb ratio, GPS, NLR, and PLR were significantly associated with prognosis of patients with Ewing sarcoma. Besides, CRP/Alb ratio is an independent and robust prognostic indicator which may have a discriminatory ability superior to that of other inflammatory indicators. Due to the retrospective design of the current study, further prospective studies are needed to validate our findings.
Acknowledgments
The authors gratefully acknowledge Dr Xin Lu, and the staff in the Department of Oncology, Department of Orthopedics and Evidence-Based Medicine Center, West China Hospital, Sichuan University. This study was supported by the Foundation of Science and Technology support plan, Department of Sichuan Province.
Disclosure
The authors report no conflicts of interest in this work.
References
Gaspar N, Hawkins DS, Dirksen U, et al. Ewing sarcoma: current management and future approaches through collaboration. J Clin Oncol. 2015;33(27):3036–3046. | ||
Jiang Y, Ludwig J, Janku F. Targeted therapies for advanced Ewing sarcoma family of tumors. Cancer Treat Rev. 2015;41(5):391–400. | ||
Li YJ, Dai YL, Cheng YS, Zhang WB, Tu CQ. Positron emission tomography (18)F-fluorodeoxyglucose uptake and prognosis in patients with bone and soft tissue sarcoma: a meta-analysis. Eur J Surg Oncol. 2016;42(8):1103–1114. | ||
Mantovani A, Allavena P, Sica A, Balkwill F. Cancer-related inflammation. Nature. 2008;454(7203):436–444. | ||
Diakos CI, Charles KA, McMillan DC, Clarke SJ. Cancer-related inflammation and treatment effectiveness. Lancet Oncol. 2014;15(11): e493–e503. | ||
Aggarwal BB, Vijayalekshmi RV, Sung B. Targeting inflammatory pathways for prevention and therapy of cancer: short-term friend, long-term foe. Clin Cancer Res. 2009;15(2):425–430. | ||
Gu X, Sun S, Gao XS, et al. Prognostic value of platelet to lymphocyte ratio in non-small cell lung cancer: evidence from 3,430 patients. Sci Rep. 2016;6:23893. | ||
Koh CH, Bhoo-Pathy N, Ng KL, et al. Utility of pre-treatment neutrophil-lymphocyte ratio and platelet-lymphocyte ratio as prognostic factors in breast cancer. Br J Cancer. 2015;113(1):150–158. | ||
Li Y, Wang C, Xu M, et al. Preoperative NLR for predicting survival rate after radical resection combined with adjuvant immunotherapy with CIK and postoperative chemotherapy in gastric cancer. J Cancer Res Clin Oncol. 2017;143(5):861–871. | ||
Altan M, Haberal HB, Akdoğan B, Özen H. A critical prognostic analysis of neutrophil-lymphocyte ratio for patients undergoing nephroureterectomy due to upper urinary tract urothelial carcinoma. Int J Clin Oncol. Epub 2017 June 9. | ||
Ishizuka M, Nagata H, Takagi K, Iwasaki Y, Shibuya N, Kubota K. Clinical significance of the C-reactive protein to albumin ratio for survival after surgery for colorectal cancer. Ann Surg Oncol. 2016;23(3):900–907. | ||
Youden WJ. Index for rating diagnostic tests. Cancer. 1950;3(1):32–35. | ||
Liu Z, Jin K, Guo M, et al. Prognostic value of the CRP/Alb ratio, a novel inflammation-based score in pancreatic cancer. Ann Surg Oncol. 2017;24(2):561–568. | ||
Camp RL, Dolled-Filhart M, Rimm DL. X-tile: a new bio-informatics tool for biomarker assessment and outcome-based cut-point optimization. Clin Cancer Res. 2004;10(21):7252–7259. | ||
Balkwill F, Mantovani A. Inflammation and cancer: back to Virchow? Lancet. 2001;357(9255):539–545. | ||
Heikkilä K, Ebrahim S, Lawlor DA. A systematic review of the association between circulating concentrations of C reactive protein and cancer. J Epidemiol Community Health. 2007;61(9):824–833. | ||
Jab łońska E, Kiluk M, Markiewicz W, Piotrowski L, Grabowska Z, Jabłoński J. TNF-alpha, IL-6 and their soluble receptor serum levels and secretion by neutrophils in cancer patients. Arch Immunol Ther Exp (Warsz). 2001;49(1):63–69. | ||
McCourt M, Wang JH, Sookhai S, Redmond HP. Activated human neutrophils release hepatocyte growth factor/scatter factor. Eur J Surg Oncol. 2001;27(4):396–403. | ||
McMillan DC. The systemic inflammation-based Glasgow Prognostic Score: a decade of experience in patients with cancer. Cancer Treat Rev. 2013;39(5):534–540. | ||
Shamamian P, Schwartz JD, Pocock BJ, et al. Activation of progelatinase A (MMP-2) by neutrophil elastase, cathepsin G, and proteinase-3: a role for inflammatory cells in tumor invasion and angiogenesis. J Cell Physiol. 2001;189(2):197–206. | ||
Kantola T, Klintrup K, Väyrynen JP, et al. Stage-dependent alterations of the serum cytokine pattern in colorectal carcinoma. Br J Cancer. 2012;107(10):1729–1736. | ||
Roxburgh CS, McMillan DC. Cancer and systemic inflammation: treat the tumour and treat the host. Br J Cancer. 2014;110(6):1409–1412. | ||
Aggerholm-Pedersen N, Maretty-Kongstad K, Keller J, Baerentzen S, Safwat A. The prognostic value of serum biomarkers in localized bone sarcoma. Transl Oncol. 2016;9(4):322–328. | ||
Ji H, Houghton AM, Mariani TJ, et al. K-ras activation generates an inflammatory response in lung tumors. Oncogene. 2006;25(14):2105–2112. | ||
Swierczak A, Mouchemore KA, Hamilton JA, Anderson RL. Neutrophils: important contributors to tumor progression and metastasis. Cancer Metastasis Rev. 2015;34(4):735–751. | ||
Lissoni P, Brivio F, Fumagalli L, et al. Efficacy of cancer chemotherapy in relation to the pretreatment number of lymphocytes in patients with metastatic solid tumors. Int J Biol Markers. 2004;19(2):135–140. | ||
Li MX, Liu XM, Zhang XF, et al. Prognostic role of neutrophil-to-lymphocyte ratio in colorectal cancer: a systematic review and meta-analysis. Int J Cancer. 2014;134(10):2403–2413. | ||
Galdiero MR, Bonavita E, Barajon I, Garlanda C, Mantovani A, Jaillon S. Tumor associated macrophages and neutrophils in cancer. Immunobiology. 2013;218(11):1402–1410. | ||
Ishii H, Takahara M, Nagato T, et al. Monocytes enhance cell proliferation and LMP1 expression of nasal natural killer/T-cell lymphoma cells by cell contact-dependent interaction through membrane-bound IL-15. Int J Cancer. 2012;130(1):48–58. | ||
Ishikawa S, Miyashita T, Inokuchi M, et al. Platelets surrounding primary tumor cells are related to chemoresistance. Oncol Rep. 2016;36(2):787–794. | ||
Orellana R, Kato S, Erices R, et al. Platelets enhance tissue factor protein and metastasis initiating cell markers, and act as chemoattractants increasing the migration of ovarian cancer cells. BMC Cancer. 2015;15:290. | ||
Sawant AC, Adhikari P, Narra SR, Srivatsa SS, Mills PK, Srivatsa SS. Neutrophil to lymphocyte ratio predicts short- and long-term mortality following revascularization therapy for ST elevation myocardial infarction. Cardiol J. 2014;21(5):500–508. | ||
Karaman M, Balta S, Seyit Ahmet AY, et al. The comparative effects of valsartan and amlodipine on vWf levels and N/L ratio in patients with newly diagnosed hypertension. Clin Exp Hypertens. 2013;35(7):516–522. | ||
Mocellin MC, Camargo CQ, Nunes EA, Fiates GM, Trindade EB. A systematic review and meta-analysis of the n-3 polyunsaturated fatty acids effects on inflammatory markers in colorectal cancer. Clin Nutr. 2016;35(2):359–369. | ||
Mocellin MC, Pastore e Silva Jde A, Camargo Cde Q, et al. Fish oil decreases C-reactive protein/albumin ratio improving nutritional prognosis and plasma fatty acid profile in colorectal cancer patients. Lipids. 2013;48(9):879–888. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.