Back to Journals » Clinical Ophthalmology » Volume 17
Clinical Features of Syphilis Patients with Ocular Symptoms as the Initial Manifestation
Authors Matsumoto H, Suzuki S, Nagata M, Senoo T, Watanabe M, Kawashima H
Received 13 June 2023
Accepted for publication 14 September 2023
Published 3 October 2023 Volume 2023:17 Pages 2901—2907
DOI https://doi.org/10.2147/OPTH.S425821
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Haruka Matsumoto,1 Shigenari Suzuki,1 Mayumi Nagata,1 Tadashi Senoo,1 Meri Watanabe,2 Hidetoshi Kawashima2
1Department of Ophthalmology, Dokkyo Medical University, Mibu, Japan; 2Department of Ophthalmology, Jichi Medical University, Shimotsuke, Japan
Correspondence: Haruka Matsumoto, Department of Ophthalmology, Dokkyo Medical University, 880 Kitakobayashi, Shimotsuga-gun, Mibu, Tochigi, 321-0293, Japan, Tel +81 282 86 1111, Fax +81 282 86 0630, Email [email protected]
Purpose: This study aimed to investigate the clinical features of patients with syphilis having ocular symptoms as the initial manifestation.
Patients and Methods: Eleven patients diagnosed with ocular syphilis at Dokkyo Medical University Hospital and Jichi Medical University Hospital between November 2018 and April 2022 were studied retrospectively.
Results: Six patients were diagnosed with secondary, three were latent, and one was tertiary stage syphilis. Ten out of 11 patients underwent cerebrospinal fluid analysis, and 1 refused. Nine out of 10 patients tested positive, of which 4 presented with neurological symptoms and the others were asymptomatic. Nine out of 11 patients tested negative for human immunodeficiency virus. Antiluetic therapy was administered to 10 out of 11 patients, which improved or maintained visual acuity at − 0.1 logMAR in 9 patients. One patient achieved the best-corrected visual acuity − 0.1 logMAR in one eye, whereas the other showed no improvement due to severe chorioretinal degeneration.
Conclusion: Ocular syphilis presents with various clinical findings and has no significant ocular manifestations without acute syphilitic posterior placoid chorioretinitis. Patients diagnosed with syphilis based on ocular symptoms should undergo cerebrospinal fluid analysis.
Keywords: syphilis, ocular syphilis, secondary stage syphilis, antiluetic therapy, neurosyphilis, sexually transmitted disease
Introduction
The prevalence of syphilis has increased enormously worldwide,1 and Japan is no exception.2,3 This retrospective study was conducted in two medical institutes located in Tochigi Prefecture, Japan. The number of patients with syphilis doubled in 2022 compared with those in 2017, from 5967 to 12,966 patients. This marked the first instance of reporting over 10,000 patients in a single year, the first time since 1999.4,5 Ocular syphilis is a relatively rare disease, reported in 0.5% of the total uveitis treated in Japan;6 however, the increase in patients with syphilis indicates that the prevalence of ocular syphilis is increasing. It is believed that there are various clinical features of syphilitic uveitis.7 Although acute syphilitic posterior placoid chorioretinitis (ASPPC) is reported as a typical fundus feature in recent years, ASPPC is only observed in 3–12% of patients and often manifests as various other clinical symptoms,7,8 which makes diagnosis difficult. Moreover, only 1–8% of patients with syphilis develop syphilitic uveitis,9 and limited studies have discussed about groups of patients with ocular syphilis in Japan. Diagnosing and providing appropriate treatment is essential to prevent permanent vision loss since successful treatment of uveitis can lead to the improvement of visual acuity.10 Neurosyphilis is another complication of syphilis in the long term. The early stages of neurosyphilis include asymptomatic meningitis, symptomatic meningitis, gumma, and meningovascular syphilis, whereas the late stages include dementia, paralytica, and tabes dorsalis.11 It is important to assess whether patients with syphilis have developed early-stage neurosyphilis, such as meningitis, to prevent late neurosyphilis, which is irreversible. This study aimed to examine the clinical features in patients with syphilis who presented with ocular symptoms as the initial manifestation, particularly in recent years.
Materials and Methods
This was a retrospective study of patients diagnosed with ocular syphilis at the Dokkyo Medical University Hospital and Jichi Medical University Hospital in Tochigi Prefecture, Japan, between November 2018 and April 2022. Informed consent is obtained from all patients for publication of this study and accompanying images. This study was approved by the Ethics Committee of the Dokkyo Medical University Hospital (No. R-66-7J), and all procedures were performed in accordance with the Declaration of Helsinki.
In this study, patients who presented to our institutions with ocular symptoms, such as unexplained uveitis, and diagnosed as active syphilis were selected. The diagnosis was confirmed using serological tests, including rapid plasma regain (RPR) and Treponema pallidum particle agglutination assay. The stages of syphilis, from the duration of possible infection opportunity as well as dermatological and neurological examination, were diagnosed. Patients were diagnosed with latent syphilis when the possible infection opportunity was more than a year ago, in addition to no experience of recurrent episodes. The Standardisation of Uveitis Nomenclature (SUN) was used to classify anterior chamber cells and vitreous opacity12 as follows: 0: none; 1+: faint; 2+: moderate; 3+: marked; and 4+: intense. Other ocular manifestations were defined to be classified in the following four stages: -: none; +: moderate; ++: marked; and +++: intense. Patients diagnosed with active syphilis but suspected of other origins of uveitis were excluded from the study.
Each patient underwent the following ophthalmological examinations: best-corrected visual acuity (BCVA), non-contact tonometry, slit-lamp biomicroscopy, and ophthalmoscopy. Optical coherence tomography and fundus fluorescein angiography were performed on selected patients.
BCVA was measured using Landolt C. Results were converted decimal to logMAR visual acuity. Counting fingers, hand movement, light perception, and no light perception vision were converted to logMAR visual acuity of 1.9, 2.3, 2.7, and 3.0, respectively, based on the report by Bach et al.13 The paired-sample t-test was used for statistical analysis. Analysis of cerebrospinal fluid (CSF) and human immunodeficiency virus (HIV) antibody status was performed on patients who agreed to participate. For CSF analysis, when the result showed an increase in the number of cells, CSF was further examined to check for laboratory characteristics of aseptic meningitis.
Patients underwent neurological and dermatological examinations following the diagnosis of syphilis. Then, the stages of syphilis were classified based on the general symptoms of the patients. All patients who provided consent chose to receive antiluetic therapy at our institution were prescribed an appropriate regimen for 14 days or longer. The antiluetic therapy included penicillin G or amoxicillin, and those who were allergic to penicillin were administered ceftriaxone or doxycycline. Ocular examination and BCVA were remeasured after antiluetic therapy at the point when RPR declined to one-quarter to that of before treatment to assess the improvement of ocular syphilis. The changes in BCVA were examined using a paired-sample t-test.
Results
In this study, 19 eyes of 11 patients belonging to 5 men and 6 women, with an average age of 53.5 ± 5.3 years, all of whom were over 20 years old, were examined. Bilateral findings were found in 8 out of 11 patients. All patients tested positive for RPR and T. pallidum hemagglutination assay and were diagnosed with active syphilis. Of the 11 patients, 6 had secondary-stage syphilis, 3 had latent, 1 had tertiary (rate), and the remaining 1 refused further clinical examination to determine the stage. None of the patients had congenital syphilis (Table 1).
 |
Table 1 Patients Background and Physiological Findings |
BCVA was measured at the first appointment and following antiluetic therapy (Table 2). Before antiluetic therapy administration, 13 of the 20 eyes showed a decline in BCVA. We administered antiluetic therapy to 10 patients, and 9 achieved improvement in visual accuracy or maintained it at −0.1 logMAR. One patient achieved BCVA −0.1 logMAR in one eye, whereas the other eye showed no improvement due to severe chorioretinal degeneration. The remaining two eyes of one case were untreated due to treatment refusal by the patient. We analyzed the BCVA before and after treatment using a t-test, which was statistically significant (P = 0.029). In our data analysis, we excluded the data of the patients who refused treatment. Within the group, some eyes showed ocular inflammation without a corresponding decline in BCVA. This indicated that ocular inflammation caused by syphilis does not necessarily manifest as a decline in BCVA.
 |
Table 2 Changes of Visual Accuracy Before and After Antiluetic Therapy |
Anterior ocular findings assessed using slit-lamp biomicroscopy are shown in Table 3. Anterior chamber cells were the most common finding among all the patients and were observed in seven eyes of five patients. Four eyes (three patients) experienced keratic precipitates (KPs), and one presented with mutton fat KPs. Iris nodules and posterior synechia were observed in one eye.
 |
Table 3 Ocular Findings at the First Appointment |
Posterior ocular findings were examined using ophthalmoscopy. Patients presented more clinical manifestations in the posterior ocular segment than that in the anterior ocular chamber. Opacitates corporis vitrei (OCV) was the most common manifestation and was seen in 13 eyes (8 patients). Other posterior ocular findings were exudative vitreoretinopathy in eight eyes of four patients, disc edema in seven eyes of five patients, macular edema in two eyes of one patient, and ASPPC in two eyes of two patients (Figure 1). Retinal vasculitis was observed in four eyes of two patients. After antiluetic therapy, ocular manifestations improved except for two eyes, in which one presented moderate OCV and the other presented posterior synechia.
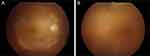 |
Figure 1 Acute syphilitic posterior placoid chorioretinitis observed at the first appointment. (A) Right eye of a 63-year-old man. (B) Left eye of a 68-year-old man. |
Other non-ocular examination results are presented in Table 1. Nine out of 11 patients were tested for HIV antibodies, and none of them were positive. CSF was extracted from 10 patients, 1 remained untested due to examination refusal. The increase of protein in CSF was considered positive; eight patients tested positive, and two tested negative, indicating neural infiltration of syphilis in these patients. However, only four patients experienced neurological symptoms, such as headache and vestibular symptoms.
Discussion
We encountered 11 patients in whom ocular symptoms were the initial symptoms, subsequently leading to a syphilis diagnosis. These patients exhibited various ocular manifestations as previously reported;9,14 however, a typical manifestation, such as ASPPC,15,16 was only observed in two eyes of two patients within our group. Intraocular inflammation is a combination of granulomatous uveitis, such as mutton fat KPs and OCV with nodular lesions, and non-granulomatous uveitis manifested as diffuse OCV associated with edema.
Complications related to HIV are common among patients with syphilis,17,18 and neurosyphilis is often observed in such patients.19 According to a study by Rasoldier et al, there was a statistically significant increase in the numbers of Treponema antibodies in the CSF of patients with co-existing HIV and syphilis.20 Therefore, HIV testing is essential for patients diagnosed with syphilitic uveitis. In our patient group, no cases of complicated HIV were observed; however, HIV testing was not carried out in two patients who declined examination.
Vanhaecke21 reported that 80% of patients with early latent syphilis who tested positive for CSF Treponema antibody only presented with ocular symptoms. Another report stated that 50% of patients with syphilitic uveitis had complications because of neurosyphilis.22 These reports suggested that a certain number of potential cases of neurosyphilis exist in patients with ocular syphilis. In this study, 8 out of 10 patients tested positive for meningitis, whereas more than half showed no neurological symptoms. All patients were confirmed HIV-negative except for two patients who refused the test. This indicated that regardless of HIV infection, ocular syphilis frequently develops into neurosyphilis. In this study, 9 patients tested for HIV were negative, and 9 out of 10 patients tested for CSF were positive for aseptic meningitis, but only 4 patients had any neurological symptoms. Therefore, it is highly likely that a high percentage of patients with ocular syphilis develop early neurosyphilis even in the absence of subjective complaints. Therefore, a neurologist should be consulted once ocular syphilis is diagnosed.
Asymptomatic neurosyphilis often shows cutaneous symptoms.23 Untreated neurosyphilis leads to late neurosyphilis, which presents with serious neurological disorders, such as progressive supranuclear palsy and locomotor ataxia. In this study, four patients showed such asymptomatic cutaneous symptoms.
Penicillin is the first choice for antiluetic therapy.24 In this study, most patients who received antiluetic therapy (both penicillin and cephems) showed alleviation of ocular symptoms, followed by an improvement in BCVA. Studies have suggested that improvement in visual acuity following syphilitic uveitis depends on the severity of vasculitis, neurosyphilis, and early therapeutic intervention.25
This study had some limitations. First, it was conducted at two medical institutions located nearby and did not examine the nationwide trends. Second, this was a retrospective study involving multiple ophthalmologists; variations in diagnosis and treatment methods occurred without a standardized protocol. Considering the increasing number of patients with syphilis in Japan, a multicenter survey is required to examine trends in disease patterns and treatment strategies among the Japanese population.
Conclusion
Ocular syphilis presents with various clinical findings and has no characteristic ocular manifestations except ASPPC. Therefore, it is important to suspect syphilis when evaluating uveitis of unknown cause. In addition, multidisciplinary medical care, including CSF analysis, should be provided to patients whose syphilis is detected by ocular symptoms.
Acknowledgments
We would like to thank Editage for English language editing. No funding was received for this study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Mathew RG, Goh BT, Westcott MC. British Ocular Syphilis Study (BOSS): 2-year national surveillance study of intraocular inflammation secondary to ocular syphilis. Invest Ophthalmol Vis Sci. 2014;55(8):5394–5400. doi:10.1167/iovs.14-14559
2. National Institute of Infectious Diseases, Japan. Infectious agents surveillance report; 2020:6–8. Available from: https://www.niid.go.jp/niid/en/iasr-vol41-e/865-iasr/9542-479te.html.
3. Sugishita Y, Kayebeta A, Soejima K, Yauchi M. Rapid increase of syphilis in Tokyo: an analysis of infectious disease surveillance data from 2007 to 2016. Western Pac Surveill Response J. 2019;10(1):6–14. doi:10.5365/wpsar.2017.8.2.006
4. Number of syphilitic patients records the highest. The Asahi Shimbun Company; 2022: 19.
5. Summary of syphilis notifications in Japan as at 5 Jan 2023. CSIER, CFEIR, Department of Bacteriology I, NIID [homepage on the Internet]. Available from: https://www.niid.go.jp/niid/images/epi/syphilis/2022q4/syphilis2022q4.pdf.
6. Sonoda KH, Hasegawa E, Namba K, et al. Epidemiology of uveitis in Japan: a 2016 retrospective nationwide survey. Jpn J Ophthalmol. 2021;65(2):184–190. doi:10.1007/s10384-020-00809-1
7. Zhang T, Zhu Y, Xu G. Clinical features and treatments of syphilitic uveitis: a systematic review and meta-analysis. J Ophthalmol. 2017;2017:6594849. PMID:28751982. doi:10.1155/2017/6594849
8. Eandi CM, Neri P, Adelman RA, Yannuzzi LA, Cunningham ET; International Syphilis Study Group. Acute syphilitic posterior placoid chorioretinitis: report of a case series and comprehensive review of the literature. Retina. 2012;32(9):1915–1941. doi:10.1097/IAE.0b013e31825f3851
9. Oliver GF, Stathis RM, Furtado JM, et al. Current ophthalmology practice patterns for syphilitic uveitis. Br J Ophthalmol. 2019;103(11):1645–1649. doi:10.1136/bjophthalmol-2018-313207
10. Gu X, Gao Y, Yan Y, et al. The importance of proper and prompt treatment of ocular syphilis: a lesson from permanent vision loss in 52 eyes. J Eur Acad Dermatol Venereol. 2020;34(7):1569–1578. doi:10.1111/jdv.16347
11. Gonzalez H, Koralnik IJ, Marra CM. Neurosyphilis. Semin Neurol. 2019;39(04):448–455. doi:10.1055/s-0039-1688942
12. Jabs DA, Nussenblatt RB, Rosenbaum JT; Standardization of Uveitis Nomenclature (SUN) Working Group. Standardization of uveitis nomenclature for reporting clinical data. Results of the First International Workshop. Am J Ophthalmol. 2005;140(3):509–516. doi:10.1016/j.ajo.2005.03.057
13. Bach M, Schulze-Bonsel K, Feltgen N, Burau H, Hansen L. Author response: numerical imputation for low vision states. Invest Ophthalmol Vis Sci. 2007;26(10.1177):2474126416680670.
14. Fu EX, Geraets RL, Dodds EM, et al. Superficial retinal precipitates in patients with syphilitic retinitis. Retina. 2010;30(7):1135–1143. doi:10.1097/IAE.0b013e3181cdf3ae
15. Gass JD, Braunstein RA, Chenoweth RG. Acute syphilitic posterior placoid chorioretinitis. Ophthalmology. 1990;97(10):1288–1297. doi:10.1016/s0161-6420(90)32418-1
16. Meira-Freitas D, Farah ME, Höfling-Lima AL, Aggio FB. Optical coherence tomography and indocyanine green angiography findings in acute syphilitic posterior placoid choroidopathy: case report. Arq Bras Oftalmol. 2009;72(6):832–835. doi:10.1590/s0004-27492009000600019
17. Li SY, Birnbaum AD, Tessler HH, Goldstein DA. Posterior syphilitic uveitis: clinical characteristics, co-infection with HIV, response to treatment. Jpn J Ophthalmol. 2011;55(5):486–494. doi:10.1007/s10384-011-0053-z
18. Tsuboi M, Nishijima T, Yashiro S, et al. Prognosis of ocular syphilis in patients infected with HIV in the antiretroviral therapy era. Sex Transm Infect. 2016;92(8):605–610. doi:10.1136/sextrans-2016-052568
19. Quilter LAS, de Voux A, Amiya RM, et al. Prevalence of self-reported neurologic and ocular symptoms in early syphilis cases. Clin Infect Dis. 2021;72(6):961–967. doi:10.1093/cid/ciaa180
20. Rasoldier V, Gueudry J, Chapuzet C, et al. Early symptomatic neurosyphilis and ocular syphilis: a comparative study between HIV-positive and HIV-negative patients. Infect Dis Now. 2021;51(4):351–356. doi:10.1016/j.medmal.2020.10.016
21. Vanhaecke C, Grange P, Benhaddou N, et al. Clinical and biological characteristics of 40 patients with neurosyphilis and evaluation of Treponema pallidum nested polymerase chain reaction in cerebrospinal fluid samples. Clin Infect Dis. 2016;63(9):1180–1186. doi:10.1093/cid/ciw499
22. Shen J, Feng L, Li Y. Ocular syphilis: an alarming infectious eye disease. Int J Clin Exp Med. 2015;8(5):7770–7777.
23. Ghanem KG. REVIEW: neurosyphilis: a historical perspective and review. CNS Neurosci Ther. 2010;16(5):e157–e168. doi:10.1111/j.1755-5949.2010.00183.x
24. Workowski KA, Bachmann LH, Chan PA, et al. Sexually transmitted infections treatment guidelines, 2021. MMWR Recomm Rep. 2021;70(4):1–187. doi:10.15585/mmwr.rr7004a1
25. Balaskas K, Sergentanis TN, Giulieri S, Guex-Crosier Y. Analysis of significant factors influencing visual acuity in ocular syphilis. Br J Ophthalmol. 2011;95(11):1568–1572. doi:10.1136/bjo.2010.194498
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
