Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 16
Clinical Features and the Outcome Evaluations of Keloid and Hypertrophic Scar Treatment with Triamcinolone Injection in Mekong Delta, Vietnam – A Cross-Sectional Study
Authors Van Nguyen L , Ly HQ, Vo HT, Pham TT, Nguyen NK, Vo TV, Phan TQ, Tran PTN, Ly HHV , Mai HTT
Received 27 July 2023
Accepted for publication 11 November 2023
Published 17 November 2023 Volume 2023:16 Pages 3341—3348
DOI https://doi.org/10.2147/CCID.S432735
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Jeffrey Weinberg
Lam Van Nguyen,1 Huy Quang Ly,1 Hau Thi Vo,1 Thao Thanh Pham,2 Nam Ky Nguyen,3 Thi Van Vo,4 Trung Quoc Phan,1 Phuong Thi Ngoc Tran,1 Hung Huynh Vinh Ly,5 Ha Thi Thao Mai1
1Department of Cosmetic Plastic Surgery, Faculty of Medicine, Can Tho University of Medicine and Pharmacy, Can Tho, Vietnam; 2Department of Dermato-Venereology, Faculty of Medicine, Can Tho University of Medicine and Pharmacy, Can Tho, Vietnam; 3Department of Pharmacology and Clinical Pharmacy, Faculty of Pharmacy, Can Tho University of Medicine and Pharmacy, Can Tho, Vietnam; 4Department of Pediatrics, Faculty of Medicine, Can Tho University of Medicine and Pharmacy, Can Tho, Vietnam; 5Department of Orthopedics, Faculty of Medicine, Can Tho University of Medicine and Pharmacy, Can Tho, Vietnam
Correspondence: Hung Huynh Vinh Ly, Department of Orthopedics, Faculty of Medicine, Can Tho University of Medicine and Pharmacy, No. 179, Nguyen Van Cu Street, An Khanh Ward, Ninh Kieu District, Can Tho, 900000, Vietnam, Email [email protected]
Background: Excessive scarring is a common problem that can have significant cosmetic and psychological consequences for patients. Intralesional injection therapy, such as the use of triamcinolone, has emerged as an effective treatment option for hypertrophic scars. The objective of this study was to describe the morphological features of hypertrophic scars, categorize them, and evaluate the efficacy of triamcinolone injection therapy in treating these scars.
Materials and Methods: A cross-sectional descriptive study of 80 patients with hypertrophic scars treated with triamcinolone intralesional injection at Can Tho University of Medicine and Pharmacy Hospital from 5/2018 to 5/2021.
Results: There were 80 patients in all, with a male/female ratio of 1/1.05 and a median age of 15– 35. There were 129 scars in all, with scar age > 1 year accounting for 83%, keloid scars accounting for 64%, and hypertrophic scars accounting for the remaining 36%. Scars are most commonly seen on the trunk, accounting for 53.5% of all scars, particularly on the anterior chest wall. When the source of scars was discovered, trauma and acne accounted for 24% and 23%, respectively, while the rest were predominantly spontaneous scars, accounting for 49%. Scarring and discomfort of mild to moderate severity were common clinical symptoms; scars larger than 5cm in size had more symptoms than scars smaller than 5cm. Prior to the therapy, the mean Vancouver Score Scale-VSS was 6.55± 2.13. After 24 weeks of the therapy, 96.7% of patients had entirely improved itching symptoms, 75% had completely improved pain, and 25% still had minimal pain. After therapy, the mean Vancouver Score Scale-VSS was 2.55± 1.81 (p< 0.05). At week 24, 3.75% of patients experienced skin shrinkage, 3.75% experienced depigmentation, and 13.75% experienced vasodilation.
Conclusion: Triamcinolone intralesional injection should be utilized as a first-line therapy for hypertrophic scarring.
Plain Language Summary: This study looked at the effectiveness of triamcinolone injection (TAC) therapy in treating hypertrophic scars, which can cause significant cosmetic and psychological problems for patients. The study included 80 patients who had hypertrophic scars and were treated with triamcinolone injections over a period of 24 weeks. The majority of the scars were keloid scars (64%) and had an age of over one year (83%). Scars were most commonly found on the trunk, especially the anterior chest wall. The most common sources of scarring were trauma and acne. Mild to moderate scarring and discomfort were common symptoms, with larger scars having more symptoms. Before treatment, the mean Vancouver Score Scale-VSS was 6.55± 2.13. After 24 weeks of treatment, 96.7% of patients had improved itching symptoms, 75% had improved pain, and 25% still had minimal pain. The mean Vancouver Score Scale-VSS was also significantly reduced after treatment (2.55± 1.81). Some side effects were observed, such as skin shrinkage, depigmentation, and vasodilation, but these were experienced by a small percentage of patients. Based on these results, the study concludes that triamcinolone injection therapy should be considered as the first-line treatment for hypertrophic scarring. This therapy was found to be effective in reducing symptoms and the overall appearance of scars, with few side effects. This study provides valuable information for healthcare professionals who treat patients with hypertrophic scars, and may help improve the quality of life for those affected by this condition.
Keywords: clinical features, hypertrophic scar, triamcinolone intralesional injection
Introduction
The formation of scars following surgery is a significant concern for both patients and healthcare professionals. During the process of scar formation, disruptions in the settlement of collagen can lead to an overproduction and buildup of collagen, resulting in the development of overgrown scars, such as keloid and hypertrophic scars. This can have a negative impact on patients’ physical and emotional wellbeing, as excessive scarring can be aesthetically displeasing and may lead to functional impairments. As a result, it is important for healthcare professionals to carefully monitor the healing process following surgery and to take appropriate measures to prevent or minimize the development of excessive scarring.1–3 These scars have a cosmetic effect, decrease function, inflict emotional and physiological damage, consequently, decrease the patient’s standard of living. We can now understand the essence of the wound rehabilitation and the disorders associated with it thanks to advances in molecular biology, genetics and technology.4 However, the answer to the determining mechanism of scar formation has yet to be discovered, so treatments and preventions continue to focus on reducing inflammation.5
Corticosteroids help to reduce inflammation. In addition, it inhibits the formation of collagen, decreases production of glycosaminoglycan, inhibits fibroblast growth, and promotes degradation of them. Corticosteroid injection, in this case using triamcinolone (TAC), is one of the most common methods.6–8
International studies on the treatment of hypertrophic scars and keloid, show that corticosteroids injection, specifically TAC, is the most recommended treatment.1,6,9–11
There has been no research into the characteristics of hypertrophic scars in Vietnam, especially the outcome and side effects of triamcinolone injection. Therefore, this study is conducted with two aims, to describe the characteristics and classify hypertrophic scars, and to evaluate the result of triamcinolone injection treatment for hypertrophic scars.
Materials and Methods
The study was conducted between May 2018 and May 2021 at the Center for Aesthetic Surgery and Skin Care, Hospital of Can Tho University of Medicine and Pharmacy, and involved 80 patients between the ages of 15 and 60 who were seeking treatment for excessive scarring. The study utilized a cross-sectional descriptive method and a non-control clinical intervention approach.
To be eligible for inclusion in the study, patients had to meet certain criteria, including the absence of ulcerative scarring, eczema, bleeding, pustules, local anesthetics allergy, hypersensitivity to the drug, Cushing’s syndrome or pseudo-Cushing’s syndrome, history or current gastrointestinal disease, infectious diseases such as pulmonary tuberculosis or disseminated fungal infection, chronic diseases such as hypertension, diabetes, heart failure, congenital or acquired immunodeficiency, the use of another topical or systemic scar treatment, and pregnancy or lactation. By carefully selecting eligible patients, the study was able to ensure that the results were meaningful and accurately reflected the outcomes of triamcinolone injection treatment for hypertrophic scars in a specific patient population.
The study recorded general characteristics of patients, including age, gender, place of residence, educational background, and occupation. Scar morphological features, such as scar number, location, and area, were also documented. Scars with surfaces smaller than 1cm2 and the same origin were considered as one scar group. Patients were classified into two groups based on the number of scars (single or multiple) and three groups based on scar age (<1 year, 1–3 years, >3 years). The origins of scarring were recorded as spontaneous, acne, trauma, incision, or ear piercing. Functional symptoms, such as itching and pain, were evaluated using a four-point scale (severe, moderate, mild, none).
Scars were categorized into keloid scars, which extend beyond the boundaries of the original lesion and can develop spontaneously over years, and hypertrophic scars, which remain within the original lesion boundaries and develop within 4 to 8 weeks after injury. Scar evaluation was based on the Vancouver Scar Scale (VSS) (Appendix 1), a semi-quantitative approach used to assess changes in the shape of burn scars during treatment. In cases of multiple scars or scar groups, the scar with the largest area was chosen for assessment. Treatment results were classified into four levels of adaptation based on VSS changes after 24 weeks: very good (>75% decrease in VSS score), good (51–75% decrease), adequate (25–50% decrease), and poor (<25% decrease). Corticosteroid-related side effects and complications, such as ulcers, infections, skin atrophy, depigmentation, vascular proliferation, thinning of scar surface, muscle tissue necrosis or atrophy, acne rash, menstrual disorders, hypertension, and gastritis, were recorded dichotomously as yes or no.
Methods of Data Collection and Evaluation
The clinical characteristics of each scar were reassessed after each treatment, with the reduction in VSS score compared to pre-procedural being calculated. Triamcinolone drug was diluted with 2% lidocaine HCl solution in a ratio of 1mL of TAC solution (80mg/mL) to 1mL of lidocaine solution to achieve a concentration of 20 mg/mL for the first injection. The number of injections should not exceed 5mL each time.
Patients were explained the study, and the anesthetic reaction was tested before sterilizing the scars and injecting the drug. The drug was injected until the scar became pale, with the needle placed 0.5 cm near the scar, parallel to it, and 1–2 mm away from its surface. This process was repeated until reaching 0.5 cm away from the lesion’s border, and the scar was then compressed with bandages. Patients were scheduled for the next session, which took place 4 weeks later.
Treatment and follow-up lasted 24 weeks, with each session taking place every 4 weeks. The treatment concluded when the scar elevation assessed on the VSS scale dropped to 0, but observation continued for another 24 weeks.
Data Processing and Analysis Methods
We assessed, synchronously coded the collected data and typed into Microsoft Excel 2016. Then we extracted, analyzed and processed data using SPSS 22.0 software, in which: The qualitative variables are described by frequency and percentage, using One-Sample Kolmogorov–Smirnov test to assess the standard distribution of the data samples. We used the Chi-square test (χ2) to compare the proportions between two or more groups and the paired t-test at the level of statistical significance of p < 0.05 to compare the mean between periods. We also implemented the Independent Sample Test to compare the mean between the two groups and One-Way ANOVA to compare mean values between multiple groups.
Research Ethics
The research is conducted honestly and seriously, the research results and suggestions are used for the purpose of improving health, limiting the occurrence and progression of diseases in the community. Ethical issues for this study were approved by the Scientific Review Committee of the Can Tho University of Medicine and Pharmacy (Approval number: 648/QDDHYDCT in 2019). The study obtained the consent of the patients (Informed consent was obtained from all participants who were 20 years of age and over. For participants under the age of 20, parental or legal guardian consent was obtained, and the participants themselves also provided their assent), and the approval of both the Can Tho University of Medicine and Pharmacy and the affiliated hospital, in accordance with the 2013 Helsinki Declaration. All research participants were provided with detailed explanations regarding the purpose and content of the study, and they voluntarily agreed to participate and collaborate throughout the research process. Participants had the right to refuse participation or withdraw from the study at any stage.
Results
The study included an equal number of male and female participants. The majority of participants were between 15–35 years old (75%), with a median age of 26 years. The highest and lowest ages were 72 and 10, respectively. The most common occupations were employees (35%) and students (30%), and 48.8% of participants had a university education or higher. The majority of participants (63.57%) lived in urban areas.
A total of 129 scars were identified, with 83% of them being more than 1 year old. Patients with one scar or a group of scars had a higher success rate (70%) compared to those with multiple scars (30%). Table 1 provides the classification of overgrown scars, with the majority of participants having keloid scars (63.57%). The main causes of scarring were spontaneous (48.83%), trauma (24.03%), and acne (23.26%), with other causes comprising 3.88%.
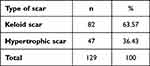 |
Table 1 Classification of Overgrown Scars |
The scars were mostly found on the chest (24.03%), anterior sternum (23.26%), legs (15.50%), lower jaw (10.08%), and shoulder (6.20%). Functional symptoms such as pruritus (82.4%) and pain (35.3%) were commonly found in the breast and chest area. Pruritus was also commonly found in the head and neck region (79.2%), but pain was less common. Before treatment, 25% of participants reported pain in the scar area (17.5% mild pain; 7.5% moderate pain), and 75% of participants had itching symptoms (68.8% mild itching; 6.2% moderate itching). Scars with an area of ≥5cm2 showed higher incidence of itching and pain compared with scars with an area of <5cm2, as shown in Table 2.
 |
Table 2 The Locations and Areas of the Scars |
The majority of scars had an area of <5cm2 (75%), with 23.8% having an area of 5–15cm2, and only 1.2% having an area of >15cm2. The average Vancouver Scar Scale (VSS) score was 6.550±2.1282, with no significant difference between men and women. However, VSS scores were significantly higher in scars that were more than 1 year old (6.902±2.1269) compared to scars that were less than 1 year old (5.421±1.7422). Table 3 shown the average VSS by number, scar area, and each scar location.
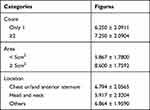 |
Table 3 Average VSS Score by Count, Area, and Location |
After 6 weeks of treatment, itching symptoms improved significantly from 91.7% mild itching and 8.3% moderate itching to 56.7% mild itching and 1.6% moderate itching, with 41.7% of participants reporting no itching. Pain symptoms also improved markedly from 70% mild pain and 30% moderate pain to 40% mild pain and 20% moderate pain, with 20% of participants reporting no pain symptoms (as shown in Figure 1).
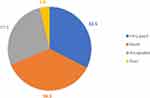 |
Figure 1 Treatment results by VSS improvement before and after treatment (24 weeks). |
After 24 weeks of treatment, 96.7% of participants had complete improvement of pruritus symptoms, and only 3.3% had mild itching. Pain improved completely in 75% of participants, and only 25% had mild pain. The mean VSS score decreased significantly from 6.550±2.1282 to 2.550±1.8135 (p<0.05).
Regarding treatment outcomes, 32.5% of participants had very good treatment results, 36.3% had good results, 27.5% had acceptable results, and only 3.8% had poor results (as shown in Table 4). Treatment results varied according to the number, location, and area of scars (as described in Table 5).
 |
Table 4 Change in VSS Means Score and Components Over Time |
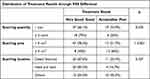 |
Table 5 Distribution of Treatment Results Through VSS Difference in Number, Area and Location of Scars |
Side effects of skin atrophy, depigmentation, and vasodilation were reported by 3.75%, 3.75%, and 13.75% of participants, respectively, at the 24th week. Side effects were observed as early as the 12th week, after 2 courses of treatment.
Discussion
Principal Findings
The study involved 80 patients, with 70% of them having one or more scars. Among these scars, 63.57% were keloids, and 36.43% were hypertrophic scars. Spontaneous scarring was the most common cause of scarring (48.83%), and the chest was the most common location for scars (24.03%). The average VSS score was 6.550±2.1282, with lower scores observed in the scar group <1 year and the scar group with an area <5cm2.
After 24 weeks of treatment, 96.7% of patients experienced complete improvement of pruritus symptoms, and pain improved completely in 75% of patients. The mean VSS score decreased significantly from 6.550±2.1282 to 2.550±1.8135 (p<0.05). Treatment outcomes, as measured by VSS improvement before and after treatment, showed that 32.5% of patients had very good results, and 36.3% had good results. These results were better in the group with a scar area <5cm2.
Possible Explanations and Comparisons with Other Studies
In comparison to other studies by Do.D., Dinh.N., Song.H., and Belie.O., our study shows significant similarities in terms of ages, clinical characteristics of overgrown scars (quantity, ages, causes, and functional symptoms), and scar treatment with TAC injection.12–15
However, there are still some discrepancies with the previous research. The gender ratio of our research greatly differs from other studies that took place in Vietnam (with the ratio of male to female was 1/4 and Dinh H.N. with that ratio was 1/2).13,14 In our research, the proportion of females and males is nearly equal. However, the number of females is greater than males, but not significantly, which is similar to that of another recent research worldwide.16,17 This shows a shift in the demands of society, with men paying more attention to cosmetic issues. In regard to the causes of overgrown scars, we found that, unlike other research, 48.83% of scars are spontaneous. However, the main causes are still trauma and acne. In addition, our Vancouver Scar Scale-VSS pre-treatment had some differences to Abedini’s research,9 which perhaps due to epidemiological factors. Our results of hypertrophic scar treatment with TAC injection are quite compatible with that of previous studies. However, there are still variations in terms of unwanted side-effects. In the research of Dinh Huu Nghi,14 3.1% of the patients had acne, 14.7% had menstrual disorders, 3.1% experienced hypertension, and according to Heitanen’s study, 44% of patients had integument atrophy and 50% had vasodilation.8 This can be due to the differences in the specimens and the time length between each injection.
Implications
The use of TAC injection remains an effective, economical, and widely applicable procedure for the treatment of excessive scarring, despite its drawbacks, particularly its potential side effects. However, to minimize these downsides, the use of a reduced dosage of TAC has been shown to be effective in decreasing the occurrence of side effects, such as integument atrophy and vasodilation. Specifically, studies have demonstrated that a 20mg/mL dose of TAC can be effective in reducing side effects, making the procedure even more beneficial for patients seeking treatment for excessive scarring. By using a reduced dosage of TAC, medical professionals can provide patients with a safe and effective treatment option that can improve their quality of life and reduce the negative impact of excessive scarring on their physical and emotional wellbeing.
Further Works
Currently, there is a lack of research data on the morphological characteristics of overgrown scars in the Vietnamese community, as well as on the outcomes and potential side effects associated with the use of intralesional triamcinolone injection for the treatment of excessive scarring. As a result, our study aimed to bridge this knowledge gap by providing a comprehensive description of the morphological characteristics of overgrown scars, as well as a thorough classification of hypertrophic scars. Additionally, we evaluated the efficacy of triamcinolone injection as a treatment option for hypertrophic scars in patients seeking medical treatment. By conducting this research, we hope to shed light on the best practices for treating excessive scarring in the Vietnamese community, and to provide healthcare professionals with the information they need to make informed decisions when treating patients with this condition.
Conclusion
Overall, excessive scar treatment with TAC injection has positive effects on all scar characteristics of the VSS (vascularity, pigmentation, pliability and height). Subsequently, the majority of patients show great improvement in functional symptoms after 24 weeks of observation and treatment, all these findings are statistically significant.
Institutional Review Board Statement
The Institutional Review Board of Can Tho University of Medicine and Pharmacy gave its approval to the study.
Data Sharing Statement
The corresponding author may obtain any data from the study upon reasonable request, [email protected] (H.H.V.L.).
Acknowledgments
We acknowledge the cooperation and support of outpatients, clinical doctors, and collaborators at the University Hospital of “Can Tho University of Medicine and Pharmacy” for the time and effort they devoted to the study. We also thank you for the support from Can Tho University of Medicine and Pharmacy.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There was no external support for this study.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Berman B, Maderal A, Raphael B. Keloids and hypertrophic scars: pathophysiology, classification, and treatment. Dermatol Surg. 2017;43:S3–S18. doi:10.1097/DSS.0000000000000819
2. Chapman MS. Keloids and Hypertrophic Scars. In: Skin Disease: Diagnosis and Treatment. Elsevier Health Sciences; 2017.
3. Lee HJ, Jang YJ. Recent understandings of biology, prophylaxis and treatment strategies for hypertrophic scars and keloids. Int J Mol Sci. 2018;19(3):711. doi:10.3390/ijms19030711
4. El-Hamid El-Azhary EA, Abd Al-Salam FM, El-Hafiz HSA, Maghraby HM. Fractional Carbon Dioxide (CO(2)) Laser Alone Versus Fractional CO(2) laser combined with triamcinolone acetonide or trichloroacetic acid in keloid treatment: a comparative clinical and radiological study. Dermatol Pract Concept. 2022;12(2):e2022072. doi:10.5826/dpc.1202a72
5. Srivastava S, Kumari H, Singh A. Comparison of fractional CO2 laser, verapamil, and triamcinolone for the treatment of keloid. Adv Wound Care. 2019;8(1):7–13. doi:10.1089/wound.2018.0798
6. Garg AM, Shah YM, Garg A, et al. The efficacy of intralesional triamcinolone acetonide (20mg/mL) in the treatment of keloid. Int Surg J. 2018;5(3):868–872. doi:10.18203/2349-2902.isj20180497
7. Hewedy E-S-S, Sabaa BE-SI, Mohamed WS, Hegab DS. Combined intralesional triamcinolone acetonide and platelet rich plasma versus intralesional triamcinolone acetonide alone in treatment of keloids. J Dermatol Treat. 2022;33(1):150–156. doi:10.1080/09546634.2020.1730742
8. Hietanen KE, Järvinen TA, Huhtala H, Tolonen TT, Kuokkanen HO, Kaartinen IS. Treatment of keloid scars with intralesional triamcinolone and 5-fluorouracil injections–a randomized controlled trial. J Plast Reconstr Aesthet Surg. 2019;72(1):4–11. doi:10.1016/j.bjps.2018.05.052
9. Abedini R, Sasani P, Mahmoudi HR, Nasimi M, Teymourpour A, Shadlou Z. Comparison of intralesional verapamil versus intralesional corticosteroids in treatment of keloids and hypertrophic scars: a randomized controlled trial. Burns. 2018;44(6):1482–1488. doi:10.1016/j.burns.2018.05.005
10. Andrews JP, Marttala J, Macarak E, Rosenbloom J, Uitto J. Keloids: the paradigm of skin fibrosis—Pathomechanisms and treatment. Matrix Biology. 2016;51:37–46. doi:10.1016/j.matbio.2016.01.013
11. Al Janahi S, Lee M, Lam C, Chung HJ. Laser-assisted drug delivery in the treatment of keloids: a case of extensive refractory keloids successfully treated with fractional carbon dioxide laser followed by topical application and intralesional injection of steroid suspension. JAAD Case Rep. 2019;5(10):840–843. doi:10.1016/j.jdcr.2019.07.010
12. Belie O, Ugburo AO, Mofikoya BO. Demographic and clinical characteristics of keloids in an urban center in Sub-Sahara Africa. Niger J Clin Pract. 2019;22(8):1049–1054. doi:10.4103/njcp.njcp_395_18
13. Dan DT. Applied research on treatment of keloids and hypertrophic scars by CO2 laser surgery. Nd-YAG laser combined with topical triamcinolone acetonide injection. Inst Clin Me Sci Res. 2006;108:1.
14. Nghi DH. Evaluation of Treatment Efficacy of Keloids with Triamcinolon Acetonid Injection in Lesions. Hanoi Medical University; 2009.
15. Song H, Tan J, Fu Q, Huang L, Ao M. Comparative efficacy of intralesional triamcinolone acetonide injection during early and static stage of pathological scarring. J Cosmet Dermatol. 2019;18(3):874–878. doi:10.1111/jocd.12690
16. Aggarwal A, Ravikumar BC, Vinay KN, Raghukumar S, Yashovardhana DP. A comparative study of various modalities in the treatment of keloids. Int J Dermatol. 2018;57(10):1192–1200. doi:10.1111/ijd.14069
17. Morelli CM, Salzillo R, Segreto F, Persichetti P. Triamcinolone acetonide intralesional injection for the treatment of keloid scars: patient selection and perspectives. Clin Cosmet Investig Dermatol. 2018;11:387–396. doi:10.2147/CCID.S133672
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
