Back to Journals » Clinical Ophthalmology » Volume 13
Clinical comparison of speculum’s influence on intraoperative aberrometry reading
Authors Lafetá Queiroz RF, Kniggendorf DV, de Medeiros AL, Hida WT , Nakano CT, Carricondo PC , Nosé W, Rolim AG, Motta AFP
Received 22 June 2018
Accepted for publication 4 February 2019
Published 7 June 2019 Volume 2019:13 Pages 953—958
DOI https://doi.org/10.2147/OPTH.S177992
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser

Rodrigo Franco Lafetá Queiroz,1,2 Danilo Varela Kniggendorf,1,2 André Lins de Medeiros,1,2 Wilson Takashi Hida,1–4 Celso Takashi Nakano,1,2 Pedro Carlos Carricondo,3 Walton Nosé,4 Andre Gustavo Rolim,1,2 Antonio Francisco Pimenta Motta1,2
1Hospital Oftalmológico de Brasília, Brasília, DF, Brazil; 2Centro de Estudos Oftalmológicos Renato Ambrósio, Brasília, DF, Brazil; 3Universidade de São Paulo, SP, Brazil; 4Universidade Federal de São Paulo, São Paulo, SP, Brazil
Purpose: The aim of this study was to evaluate the influence of four different types of speculums on aberrometry reading (OPD SCAN III [OPD]) and on intraoperative aberrometry reading (optiwave response analyzer, ORA).
Patients and methods: This prospective, controlled, comparative study of consecutive cases included the evaluation of five eyes of five patients with monofocal intraocular lens (IOL) implantation. Seventeen measures were performed on each patient: for each speculum, there were two measurements on the OPD and another two on ORA with four different types of blepharostats. A control measure was performed on the without blepharostat in the dominant eye of each patient, therefore totalizing 85 measurements. The measures with the blepharostats were as follows: without pressure (WF) or passive measure and after pressure (AF) or active measure to close the eye. The speculum used in all patients was as follows: open-edged wire (Barraquer); threaded with open blade (Lieberman), with 21 mm aperture; wired with solid blade (Barraquer); and threaded with solid blade (Lieberman) with 21 mm opening. An evaluation of the objective refractive data from the OPD and ORA and the corneal astigmatism from the OPD was performed.
Results: Spherical equivalent (SE) of the OPD with the use of blepharostat compared to the OPD without speculum presented only 37.5% of results without statistical significance. Regarding the SE of ORA with speculum usage, compared to the OPD without blepharostat, only 12.5% were not significant. Regarding the accuracy of the ORA refractive axis with the use of blepharostats, all results presented statistical significance.
Conclusion: Thus, in the present study, we reached the conclusion between the studied blepharostats that the most suitable for use in the aphakic and pseudophakic capture of the ORA is the open blade threaded blepharostat (Lieberman).
Keywords: cataract, surgery, astigmatism, corneal topography, cornea
Introduction
Cataract surgery became increasingly safer and more reproducible over the recent years with the introduction of modern techniques of phacoemulsification and with the evolving technology combined with the introduction of femtosecond laser and anti-surge mechanisms, being the most performed surgery in the world.1
The opening of the eyelid for ocular surgery used to be a complex problem. Three procedures were suggested for the solution of this problem, involving the use of the following: retractors (insured by an assistant), blepharostats (speculum), sutures (inserted into the free eyelid border or skin or held in place by means of metallic devices).2
Along with an increasingly early diagnosis, there is currently a greater demand among patients who want to maintain their productivity and daily activities.3
A postoperative outcome without refractive errors is one of the main objectives of modern phacoemulsification. The corneal topography has been the most used examination to guide the surgical plane and to evaluate the postoperative results. Nevertheless, real-time information about the refractive state during cataract surgery can assist in the correct placement of intraocular lenses (IOLs), and it may also automatically consider the induced astigmatism in clear corneal incisions.4
Wavefront aberrometry is widely used to improve outcomes after visual laser correction. However, the types of aberrometers used in keratorefractive surgeries are too large to be used intraoperatively, and their variation and dynamic range are not wide enough for the aphakic measures required for cataract surgery. The optiwave response analyzer (ORA; Alcon Inc, Fort Worth, TX, USA) is small enough to be mounted under the surgical microscope and is fully integrated into an easy and accessible interface for the surgeon; it is the third-generation version of the intraoperative aberrometry system.5–7 OPD-SCAN III ([OPD]; Nidek, Gamagori, Japan) is an aberrometer popularly used in the preoperative period of cataract surgery for surgical incision programming and astigmatism correction.8
Therefore, it requires a blepharostat that induces the least refractive error to calculate the IOL to be implanted. The purpose of this study was to evaluate the influence of four different types of blepharostats on aberrometry reading (OPD) and on intraoperative aberrometry reading (ORA) in order to know whether there is a significant difference between them.
Patients and methods
This prospective, controlled, comparative study of consecutive cases included the evaluation of five eyes of five patients submitted to femtosecond laser cataract surgery with monofocal IOL implantation. Four measures were performed with each blepharostat: two on the OPD and another two on ORA (intraoperative aberrometer) with four different types of blepharostats. A control measure was performed on the OPD, aberrometer, without speculum in the dominant eye of each patient. Therefore, despite a small number of subjects, we could reach a total amount of 85 measurements in this paper. The measures with the blepharostats were as follows: without force (WF) or passive measure and after forcing (AF) or active measure to close the eye.
The speculum used in all cases was as follows: open-edged wire – Barraquer (speculum Barraquer odous with open blade [B1]; Odous, Belo Horizonte, Brazil; Figure 1); threaded with open blade – Lieberman forceps (speculum Lieberman forceps with open blade [B2]; Katena, Denville, NJ, USA), with 21 mm aperture (Figure 2); wired with solid blade – Barraquer (speculum Barraquer odous with closed blade [B3]; Odous; Figure 3); and threaded with solid blade – Lieberman (speculum Lieberman odous with closed blade [B4]; Odous; Figure 4) with 21 mm opening; all were made from the same material.
  | Figure 1 B1 – speculum Barraquer odous with open blade. |
  | Figure 2 B2 – speculum Lieberman forceps with open blade. |
  | Figure 3 B3 – speculum Barraquer odous with closed blade. |
  | Figure 4 B4 – speculum Lieberman odous with closed blade. |
An evaluation of the objective (spherical, cylinder, and axis) refractive data from the OPD and ORA and the corneal astigmatism (flat axis value [K1], steep axis value [K2], and respective axis) from the OPD was performed. Spherical equivalent (SE) was the primary outcome measure.
Inclusion criteria were as follows: age between 50 and 75 years, axial length between 22.5 and 24.5 mm, femtosecond laser-assisted cataract surgery, absence of posterior capsule opacity, corneal thickness between 500 and 580 mm. Exclusion criteria were as follows: ocular pathologies, irido-corneal angle <25°, eyelid drooping.
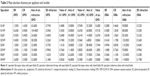
Statistical significance was tested using Student’s t-test and p-value for the analysis of the data collected. To infer the conclusion about which would be the best blepharostat, an absolute numerical methodology was applied, using a summary of significant p-values for each variable and apparatus (Table 1) and a table of means for each variable and apparatus (Table 2). Then, a ranking of the points of the lowest variations was performed when compared to the examination without speculum. After that, a numerical result was verified for each variable, being excluded from the ranking when the values were statistically significant (Table 3). In this way, we took the sum of the ranking for each variable and multiplied by the number of times it was statistically significant, thus obtaining a general ranking where the lowest value equals the best blepharostat (Table 4).
The study was conducted in accordance with the principles of the Declaration of Helsinki and was approved by the institutional review board (IRB) of the Hospital Oftalmológico de Brasília with written informed consent provided by the patients.
Results
Comparing the spherical refraction in the OPD with and without blepharostat, B1 without pressure (WF), B2 after pressure (AF), B3AF, B3WF, B3AF, and B4AF were statistically significant (0.50 D of median±0.38 D of SD, p=0.0186; 0.50±0.41 D, p=0.0402; 1.25±0.57 D, p=0.007; 1.50±0.72 D, p=0.0138; 0.25±0.33 D, p=0.0367, respectively); the other analyses were not significant.
In the cylindrical refraction from the OPD with and without blepharostat, only the blepharostats, B3AF and B3WF, presented statistical significance (2.50±0.94 D, p=0.0058; 1.25±0.70 D, p=0.0244, respectively).
With respect to the axis of refraction in the OPD, only the B1WF, B2AF, and B4WF blepharostats presented statistical significance (82°±46.38°, p=0.0073; 29°±18.39°, p=0.0403; 38°±40.78°, p=0.0448, respectively).
The SE presented statistical significance in the blepharostats such as B1WF, B2AF, B2WF, B3AF, and B4AF (0.50±0.40 D, p=0.03; 0.38±0.10 D, p=0.0009; 0.13±0.13 D, p=0.0184; 0.74±0.54 D, p=0.034; 1.00±0.58 D, p=0.0158, respectively).
When we evaluated the corneal curvature with the OPD, we observed that the blepharostats, B1WF, B1AF, B2WF, B2AF, and B4WF, significantly altered the corneal axis (K1; 0.37± 0.32 D, p=0.048; 0.28±0.33 D, p=0.0476; 0.62±0.43 D, p=0.029; 0.97±0.39 D, p=0.0135; 0.54±0.55 D, p=0.0269, respectively).
However, when we observed the K1 axis, no blepharostat presented statistically significant results. The most curved axis (K2) was statistically significant in the following: B1AF, B3AF, and B3WF (0.70±0.27 D, p=0.042; 1.53±0.52 D, p=0.0045; 0.59±0.51 D, p=0.0201, respectively).
In the K2 axis only, the B2AF blepharostat presented a statistically significant result, 16°±7.96°, p=0.0155.
With respect to the astigmatism of the OPD, only the B3AF and B3WF speculums had significant results (2.04±1.59 D, p=0.0181; 1.42±0.70 D, p=0.0149, respectively).
When we compared the blepharostats in the spherical refraction in the ORA device, we obtained the following blepharotats with significance: B1AF, B1WF, B2AF, B3WF and B4AF (0.2±0.0942 D, p=0.0078; 0.52±0.3174 D, p=0.0393; 0.71±0.5633 D, p=0.0315; 1.18±0.3057 D, p=0.0016; 0.41±0.1837 D, p=0.0136, respectively).
In the cylindrical refraction, we found the following blepharotats with significance: B1AF, B2WF, B3AF, B3WF, B4AF, and B4WF (0.57±0.2230 D, p=0.0095; 1.11±0.2520 D, p=0.0005; 0.96±0.2261 D, p=0.0011; 0.65±0.4235 D, p=0.0186; 0.92±0.5705 D, p=0.0113; 1.00±0.5527 D, p=0.0094, respectively).
In the comparison of the ORA refraction axis, all B1AF, B1WF, B2AF, B2WF, B3AF, B3WF, B4AF, and B4WF were statistically significant (89°±11,4543°, p=0.0001; 90°±16.9263°, p=0.0003; 83°±7.8549°, p=0.00001; 119°±24.4131°, p=0.0003; 123°±23.8584°, p=0.0005; 106°±21.9704°, p=0.0007; 135°±27.3002°, p=0.0005; 112°±30.2605°, p=0.0011, respectively).
As for SE in the ORA, B1AF, B1WF, B2AF, B2WF, B3WF, B4AF and B4WF presented statistical significance (0.15±0.2501 D, p=0.0451; 0.35±0.1976 D, p=0.0167; 0.35±0.1031 D, p=0.002; 0.19±0.1412 D, p=0.0147; 1.00±0.2406 D, p=0.0008; 0.57±0.3898 D, p=0.0388; 0.21±0.1094 D, p=0.022, respectively).
Discussion
This is the first study to compare the effect of blepharostats on the ORA aberrometric measurement; furthermore, this is an unpublished study and there are no other studies to compare with. As a comparison of the data collected from the OPD with speculum with the data of the OPD without blepharostat and with the ORA measurement data was performed, a correlative inference between the OPD groups with speculum and ORA with speculum regarding the statistical comparison was established; therefore, the blepharostat that might influence less on the aphakic reading of the ORA could be settled.
In the present study, there was an observation that the SE of the OPD with the use of blepharostat compared to the OPD without blepharostat presented only 37.5% of results without statistical significance. Regarding the SE of the ORA with the use of speculums compared to the OPD without blepharostat, only 12.5% were not significant. Regarding the accuracy of the ORA axis with the use of blepharostats, all results presented statistical significance.
Conclusion
It is possible to infer that the comparative analysis of ORA in relation to the OPD without blepharostat was inferior to the analysis of the OPD with speculum. The open blade threaded blepharostat (Lieberman, Katena) was the most similar to the data capture of the OPD without speculum, when the patient does or does not force the eye to close. Thus, in the present study, we reached the conclusion that the most suitable for use in the aphakic and pseudophakic ORA capture is the open blade threaded blepharostat, Lieberman (Katena), probably due to the speculum design.
Acknowledgments
The abstract of this paper was presented at the American Society of Cataract and Refractive Surgeons (ASCRS) Annual Meeting 2018 in Washington, DC, USA, as a poster presentation with interim findings. The poster’s abstract was published in “Poster Abstracts” in the ASCRS Annual Meeting Journal.
Disclosure
The authors report no conflicts of interest in regard to this paper.
References
Abell RG, Vote BJ. Cost-effectiveness of femtosecond laser-assisted cataract surgery versus phacoemulsification cataract surgery. Ophthalmology. 2014;121(1):10–16. | ||
Barraquer JI. New blepharostat for ocular surgery of anterior segment. Ophthalmologica. 1957;134(3):200–202. | ||
Maxwell WA, Cionni RJ, Lehmann RP, Modi SS. Functional outcomes after bilateral implantation of apodized diffractive aspheric acrylic intraocular lenses with a +3.0 or +4.0 diopter addition power Randomized multicenter clinical study. J Cataract Refract Surg. 2009;35(12):2054–2061. | ||
de Medeiros AL, de Araújo Rolim AG, Motta AFP, et al. Comparison of visual outcomes after bilateral implantation of a diffractive trifocal intraocular lens and blended implantation of an extended depth of focus intraocular lens with a diffractive bifocal intraocular lens. Clin Ophthalmol Auckl NZ. 2017;11:1911–1916. | ||
Chen M. An evaluation of the accuracy of the ORange (Gen II) by comparing it to the IOLMaster in the prediction of postoperative refraction. Clin Ophthalmol Auckl NZ. 2012;6:397–401. | ||
Hemmati HD, Gologorsky D, Pineda R. Intraoperative wavefront aberrometry in cataract surgery. Semin Ophthalmol. 2012;27(5–6):100–106. | ||
Ianchulev T, Hoffer KJ, Yoo SH, et al. Intraoperative refractive biometry for predicting intraocular lens power calculation after prior myopic refractive surgery. Ophthalmology. janeiro de 2014;121(1):56–60. | ||
Pathak B, Boruah BR. Improvement in error propagation in the Shack-Hartmann-type zonal wavefront sensors. J Opt Soc Am A Opt Image Sci Vis. 2017;34(12):2194–2202. |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.