Back to Journals » Infection and Drug Resistance » Volume 11
Clinical characteristics and antimicrobial resistance of pneumococcal isolates of pediatric invasive pneumococcal disease in China
Authors Cai K, Wang Y , Guo Z, Xu X, Li H, Zhang Q
Received 14 August 2018
Accepted for publication 25 October 2018
Published 26 November 2018 Volume 2018:11 Pages 2461—2469
DOI https://doi.org/10.2147/IDR.S183916
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Sahil Khanna
Kang Cai,1 Yizhong Wang,2 Zhongqin Guo,3 Xiaonan Xu,1 Huajun Li,1 Qingli Zhang1,4
1Department of Pediatrics, Xinhua Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China; 2Department of Infectious Diseases, Shanghai Children’s Hospital, Shanghai Jiao Tong University, Shanghai, China; 3School of Public Health and Management, Ningxia Medical University, Yinchuan, China; 4Department of Pediatrics, Xinhua Hospital, Shanghai Jiao Tong University School of Medicine, Chongming Branch, Shanghai, China
Purpose: Streptococcus pneumoniae causes serious infections globally, including invasive pneumococcal disease (IPD). We analyze clinical features of pediatric IPD cases identified in China and antibiotic susceptibility of isolated pneumococcal strains.
Methods: Confirmed pediatric IPD patients were prospectively recruited to the study. Symptoms at the time of hospitalization, laboratory tests, antimicrobial susceptibility of pneumococcal isolates, treatments, hospital stay, and residual findings at discharge were analyzed systematically.
Results: From January 2008 to December 2017, a total of 123 hospitalized children diagnosed with IPD were enrolled: 68 from pediatric departments of Xinhua Hospital, and 55 from Lanzhou University Second Hospital. Of these pediatric IPD patients, 81 (65.86%) were male, and 98 (79.67%) <5 years old. Most cases (96, 78.05%) were diagnosed during the cold season between September and February. Sepsis was observed in 82 (66.67%) patients, 48 (39.02%) children were diagnosed with meningitis, 41 (33.33%) with pneumonia, 30 (24.39%) with pleurisy, and 4 (3.25%) with osteomyelitis. Underlying diseases were noted in 35 (28.45%) patients and concurrent infections in 45 (36.58%). The overall mortality rate was 2.44%. IPD children who developed sepsis and necrotizing pneumonia showed higher proportions of intensive care-unit admission, intravenous γ-globulin, glucocorticoid use, hemofiltration and ventilator, and longer duration of fever, hospital stay, and antibiotic use than nonsepsis and pneumonia subjects. Antimicrobial resistance of S. pneumoniae showed a highly unsusceptible rate for erythromycin (96.75%), trimethoprim-sulfamethoxazole (79.67%), and tetracycline (77.23%). All isolates were sensitive to vancomycin, linezolid, and levofloxacin.
Conclusion: Clinical symptoms were severe in the majority of pediatric IPD patients. More intensive treatments were demanded for IPD children with sepsis and necrotizing pneumonia. High resistance rates for erythromycin, trimethoprim–sulfamethoxazole, and tetracycline were found.
Keywords: Streptococcus pneumoniae, children, invasive pneumococcal disease, antimicrobial resistance
Introduction
Streptococcus pneumoniae is a major cause of serious infections associated with high morbidity and mortality globally.1 Normally, S. pneumoniae colonizes asymptomatically in the nasopharynx of healthy carriers; however, it can be pathogenic and transmit to other locations, causing both noninvasive and invasive diseases in susceptible individuals, particularly in young children and elderly people.2 Invasive pneumococcal disease (IPD) is defined as isolation of S. pneumoniae from a normally sterile body site, such as blood, cerebrospinal fluid (CSF), synovial fluid, pericardial fluid, pleural fluid, and peritoneal fluid, corresponding with bacteremia, meningitis, septic arthritis, pericarditis, pleurisy, and peritonitis, respectively.2 Mortality rates of children associated with IPD are approximately 5.3%–27.5%, and even higher dependent on the IPD type.3–6 It has been reported that IPD causes more than 1 million deaths annually worldwide, mostly children aged <5 years.7,8 Most of IPD associated deaths occur in developing countries, including China.1,7 In 2000, it was estimated that around 30,000 children <5 years old died from IPD in China.1 Studies have aimed to analyze pediatric IPD characteristics in different regions of China in the last few decades. For example, 31 pneumococcal isolates of IPD patients aged <5 years from eight cities were reported in 2008.9 In another study, 61 invasive pneumococcal strains were isolated from pediatric patients in a single hospital.10 A study of eleven centers identified 171 pneumococcal isolates from pediatric IPD cases, which yielded 5.2 pneumococcal isolates per hospital per year on average.11 In addition, a total of 80 IPD children were identified from January 2010 to December 2015 in Suzhou.12 In the current study, we aimed to analyze clinical features of pediatric IPD cases identified in Shanghai and Lanzhou, China and antimicrobial resistance of pneumococcal strains isolated from those IPD children.
Methods
Study cohort
A total of 123 hospitalized children <14 years of age diagnosed with confirmed IPD between January 2008 and December 2017 in the pediatric departments of Xinhua Hospital, Shanghai Jiao Tong University School of Medicine, and Lanzhou University Second Hospital, China, were prospectively enrolled in the study. Shanghai is located in the east of China, and Lanzhou in the west. The diagnosis of IPD was based on cultures positive for S. pneumoniae that were isolated from a normally sterile body site, including blood, CSF, synovial fluid, pericardial fluid, pleural fluid, and peritoneal fluid. Non-IPD children with S. pneumoniae from sputum were excluded from the study. Pneumococcal sepsis was defined by a positive blood culture for S. pneumoniae with at least two of four criteria: fever >38.0 °C or hypothermia <36.0 °C, tachycardia >90 beats/min, tachypnea >20 breaths/min, leukocytosis >12×109/L, and leucopenia.13 Necrotizing pneumonia was diagnosed by the formation of abscesses and cavitation within the lung parenchyma.14 Written informed consent was obtained from parents or legal guardians of children eligible for study enrollment. This study was approved by the regional ethical review boards in Xinhua Hospital and Lanzhou University Second Hospital, and was carried out in accordance with the principles of the Declaration of Helsinki. Data were systematically extracted from the hospital records of enrolled children: symptoms and findings at time of hospitalization, laboratory-test results, length of hospital stay, treatments, and residual clinical findings at discharge.
Serology testing
An indirect immunofluorescence-assay kit (Pneumoslide; Vircell, Granada, Spain) was used for the simultaneous diagnosis in human serum of IgM antibodies of the main infectious agents of the respiratory tract, including Mycoplasma pneumoniae, Coxiella burnetii, Chlamydophila pneumoniae, adenovirus, respiratory syncytial virus, influenza A, influenza B, and parainfluenza serotypes 1–3. Epstein–Barr virus (EBV)-antibody tests of EBV viral capsid antigens IgM and IgG, EBV nuclear antigen IgG antibodies, and Cytomegalovirus IgM and IgG were performed with a Liaison assay (DiaSorin, Saluggia, Italy).
S. pneumoniae isolation
Blood, CSF, synovial fluid, pericardial fluid, pleural fluid, and peritoneal fluid samples taken from IPD children were inoculated on blood-agar plates and incubated at 35°C, 5% CO2 incubators for 24 hours. S. pneumoniae isolates were identified by colony morphology on blood agar and optochin test, and confirmed by matrix-assisted laser desorption/ionization time-of-flight (MALDI-TOF) mass spectrometry (Microflex LT; Bruker, Billerica, MA, USA). For MALDI-TOF analysis, bacterial proteins from blood cultures were extracted using a MALDI Sepsityper kit (Bruker). Each purified blood-culture extract (1 µL) was transferred to an individual spot on the Bruker 96-spot target plate and covered with a 1 µL α-cyano-4-hydroxycinnamic acid matrix (Bruker). The target plate was then read and analyzed by the Bruker Microflex LT system. A protein profile of each specimen with m/z values of 3,000–15,000 was generated based on a minimum of 240 laser-shot measurements. Profiles were further analyzed using Biotyper 3.0 software (Bruker) in blood-culture mode according to the manufacturer’s recommendation.
Antimicrobial resistance testing
Antimicrobial resistance testing of the confirmed S. pneumoniae isolates was determined by Etest and Kirby–Bauer disk on Mueller–Hinton agar plates following Clinical and Laboratory Standard Institute guidelines. Antibiotics tested by Etest assay were penicillin and ceftriaxone. Colonies were transferred into test tubes of 5 mL normal sterile saline adjusted to obtain turbidity matching 0.5 McFarland standard. Isolates were inoculated onto Mueller–Hinton agar with sheep-blood plates, and disks impregnated with antimicrobial agents were dispensed on inoculated plates, incubated at 35°C and 5% CO2 for 20–24 hours, and zones of inhibition measured after incubation. For determination of drug resistance, antibiotic-susceptibility breakpoints for S. pneumoniae were according to the 2008 amendments to the Clinical and Laboratory Standard Institute guidelines. Commercial antibiotic disks of amoxicillin (25 µg), cefuroxime (30 µg), cefotaxime (30 µg), chloramphenicol (30 µg), erythromycin (15 µg), levofloxacin (5 µg), linezolid (30 µg), meropenem (10 µg), tetracycline (30 µg), vancomycin (30 µg), and trimethoprim–sulfamethoxazole (25 µg) were purchased from Thermo Fisher Scientific, and penicillin (25 µg) disks were purchased from BioMérieux. The quality-control strain was S. pneumoniae ATCC49619.
Statistical analysis
Statistical analysis was performed with SPSS 24 for Windows. Rank-sum tests were used to evaluate the significance of different groups. All data are presented as medians with IQR. Statistical significance was defined as P<0.05.
Results
Clinical and demographic characteristics of pediatric IPD patients
Among a total of 123 hospitalized children diagnosed with IPD from January 2008 to December 2017, 68 were enrolled from the pediatric departments of Xinhua Hospital, and 55 from Lanzhou University Second Hospital. As shown in Figure 1, a total of 151 S. pneumoniae isolates were isolated from specimens of 123 patients, including 82 isolates from blood, 29 isolates from CSF, and 40 isolates from pleural fluid. There were 28 repeated isolates from different types of specimens from the same patients (13 repeated isolates from blood and CSF specimens, 15 repeated isolates from blood and pleural fluid). No statistical difference was observed by comparison of characteristics of subjects from the two sites, including age, sex, and clinical manifestations (data not shown). As shown in Table 1, of those pediatric IPD patients, 81 (65.86%) were male and 98 (79.67%) <5 years old. A seasonal trend was observed, with 78.05% of all cases diagnosed during the cold season between September and February. In contrast, the lowest frequency was found during June–August (4.88%). Sepsis was observed in a total of 82 (66.67%) patients, with 48 (39.02%) children diagnosed with meningitis, 41 (33.33%) with pneumonia, 30 (24.39%) with pleurisy, and four (3.25%) with osteomyelitis. A total of 35 (28.45%) patients had underlying diseases, including nine with congenital heart diseases, eleven with malnutrition, and 15 with anemia. Concurrent infection was noted in 45 patients: nine (7.32%) children were coinfected with EBV, eleven (8.94%) with respiratory syncytial virus, and 25 (20.33%) with Mycoplasma pneumoniae. None of the IPD children was taking pneumococcal conjugate vaccine (PCV). Data on health status at hospital discharge showed that 120 (97.56%) children were clinically healthy when they left the hospital, while three (2.44%) had died.
  | Figure 1 Diagram of pneumococcal isolates identification process. |
  | Table 1 Clinical and demographic characteristics of children with invasive pneumococcal disease in Shanghai (n=68) and Lanzhou (n=55), 2008–2017 |
Comparison of disease severity in IPD children with or without sepsis
Among 82 IPD children who developed sepsis, 58 (72.5%) were male, and all patients aged <12 months (30) developed sepsis (Table 2). Comparison of laboratory tests showed that the number of subjects with elevated white-blood-cell counts and CRP levels were significantly higher in patients with sepsis than those without sepsis. In pediatric IPD subjects who developed sepsis, the proportions of intensive care-unit admission, intravenous γ-globulin (IVIG), glucocorticoid use, hemofiltration, and ventilator were 56.09%, 92.68%, 97.56%, 47.56%, and 14.63%, respectively, significantly higher than nonsepsis patients. Hospital data showed that duration of fever, hospital stay, and antibiotic use in the sepsis group were 12 (IQR 9–15), 16 (IQR 13–20), and 17 (IQR 15–22) days, respectively, significantly longer than the nonsepsis group: 7 (IQR 6–9), 11 (IQR 8.5–13), and 11 (IQR 9–14) days. The overall mortality rate was 3.66% (three of 82) in the sepsis group, and no deaths happened in nonsepsis patients (Table 2).
Comparison of disease severity in IPD children with necrotizing pneumonia and pneumonia
A total of 41 IPD children were diagnosed with pneumonia, with necrotizing pneumonia observed in eleven (Table 3). All patients with necrotizing pneumonia showed elevated white-blood-cell counts. Hydrothorax was observed in most IPD patients with necrotizing pneumonia (eight of eleven, 72.72%). Proportions of pediatric IPD subjects that received bronchoscopy, pleural perfusion, ventilator, and hemofiltration were 81.81%, 45.45%, 54.54%, and 100% in necrotizing pneumonia patients, significantly higher than patients with pneumonia. All pediatric IPD subjects with necrotizing pneumonia were treated with IVIG and glucocorticoid. Hospital data showed that duration of fever, hospital stay, and antibiotic use was 15 (IQR 13–18), 25 (IQR 23–26), and 23 (IQR 21–25) days, respectively, significantly longer than the pneumonia group (Table 3).
Antimicrobial resistance
As shown in Table 4, total insusceptibility rates of penicillin, amoxicillin, chloramphenicol, ceftriaxone, cefotaxime, and meropenem were 27.64% (34 of 123), 21.13% (26 of 123), 18.69% (23 of 123), 29.36% (36 of 123), 31.71% (39 of 123), and 48.78% (60 of 123), respectively. High insusceptibility rates of S. pneumoniae isolates were observed in erythromycin (96.75%, 119 of 123), tetracycline (77.23%, 95 of 123), and trimethoprim–sulfamethoxazole (79.67%, 98 of 123) tests. No statistical differences were found in the antimicrobial susceptibility of most tested antibiotics between Shanghai and Lanzhou, except for cefotaxime, which was higher in Shanghai than Lanzhou (P<0.042). All isolates were sensitive to vancomycin, linezolid, and levofloxacin.
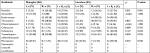  | Table 4 Antimicrobial susceptibility of pneumococcal isolates from children with invasive pneumococcal disease in Shanghai (n=68) and Lanzhou (n=55) Abbreviations: I, intermediate; R, resistant. |
Discussion
S. pneumoniae is a leading bacterial pathogen that causes both noninvasive and invasive diseases worldwide.1,15,16 It was estimated that S. pneumoniae caused 14.5 million episodes of serious disease and was responsible for 11% of all deaths in children aged <5 years in 2000.1 In the current study, we identified a total of 123 pediatric IPD patients from January 2008 to December 2017 in Shanghai and Lanzhou, China. Most patients (98, 79.67%) were <5 years old and diagnosed during the cold season, which was similar to several recent reports from China.12,17 For example, a recent study showed that most pediatric IPD patients (77 of 80) were aged <5 years.12 Normally, IPD causes more severe clinical symptoms than noninvasive community-acquired pneumonia and can be fatal. Among these confirmed pediatric IPD cases, the overall mortality rate was 2.44% (three of 123), which was lower than other reports with mortality of 5.3%–27.5%.3–6 IPD was defined as culture-positive S. pneumoniae from normally sterile body sites.
Our data showed that 82 blood specimens, 31 CSF specimens, and 40 pleural fluid specimens from 123 IPD subjects were S. pneumoniae-positive. Some patients were found to be S. pneumoniae-positive from more than one sterile body site, ie, 13 subjects were S. pneumoniae-positive in both blood and CSF, and 17 were S. pneumoniae-positive in both blood and pleural fluid. Based on the clinical features and results of S. pneumoniae culture results, the numbers of children diagnosed with meningitis, pneumonia, pleurisy, and osteomyelitis were 48 (39.02%), 41 (33.33%), 30 (24.39%), and 4 (3.25%), respectively. It has been implicated that the presence of an underlying chronic disease is a risk factor for IPD.4,18,19 Two recent studies showed that around 15%–16% of IPD children had an underlying disease.12,20 In our identified IPD cases, underlying diseases were observed in 35 (28.45%) patients. Furthermore, concurrent infection with other pathogens was also reported in IPD children. It has been reported that most IPD children (44 of 71, 62%) <5 years of age were coinfected with respiratory virus, with rhinovirus and influenza virus being the most frequently detected.21 Concurrent infection was also noted in our study: 45 patients (36.58%) were coinfected with other pathogens, including EBV and respiratory syncytial virus.
S. pneumoniae-caused bacterial sepsis is a main life-threatening pneumococcal disease in children. A study has shown that 13.3% of subjects suffered sepsis among 15 IPD cases with S. pneumoniae positive in blood.22 Chiu et al showed that 28 pediatric patients (56%) had sepsis among 50 identified IPD patients.20 In a study from Peru, 7.9% of pediatric patients were diagnosed with sepsis in a total of 101 IPD episodes studied, with an overall case-fatality rate of 22.0%.23 From January to December 2006, 768 children with sepsis were observed in three hospitals with 2,219 hospitalizations of IPD children <5 years of age in Bangalore, India, and 87 deaths were attributable to sepsis in a total of 178 deaths.24 It was reported that two of five fatal cases among 41 confirmed pediatric IPD were due to sepsis.25 In the current study, a total of 82 (66.67%) pediatric IPD patients with sepsis were identified, which was comparable with the study by Chiu et al.20 Comparison of disease severity and outcome of IPD children with or without sepsis showed that patients with sepsis had more severe symptoms, higher proportion of referrals to intensive care units, longer duration of hospital stay, fever, and antibiotic use, and all three deaths were in IPD patients with sepsis. All patients aged <12 months developed sepsis, suggesting that young age is a high risk factor for sepsis in IPD.
Pneumonia is a major common clinical complication of S. pneumoniae infection. Studies show that the majority of pediatric IPD subjects suffer from pneumonia.18,20 Necrotizing pneumonia is defined as the development of necrosis, liquefaction, and cavitation of the lung parenchyma from an infectious pathogen, including S. pneumoniae.26 Necrotizing pneumonia remains an uncommon complication of pneumonia in children, but its incidence is increasing. Pneumococcal infection is the predominant cause of necrotizing pneumonia in children.14 In all 41 IPD children with pneumonia, 11 were diagnosed with necrotizing pneumonia, and the proportions of pediatric IPD subjects receiving bronchoscopy, pleural perfusion, ventilator, and hemofiltration were significantly higher in patients with necrotizing pneumonia than pneumonia. The numbers of patients treated with IVIG and glucocorticoid were significantly higher in necrotizing pneumonia subjects, and duration of fever, hospital stay, and antibiotic use were longer than pneumonia, suggested that more intensive care was required in IPD children with necrotizing pneumonia.
Pneumococcal resistance to antimicrobials is a serious and growing problem globally, particularly in Asian regions. It has been shown that Asian regions have the highest levels of S. pneumoniae-antibiotic resistance.27 High erythromycin-resistance rates S. pneumoniae isolates have been reported in several studies in China, eg, rates of 96.4% in Beijing,17 85.7% in Shanghai,28 and 92.1% in Chongqing.29 A multicenter survey of eleven centers also showed a high rate of erythromycin resistance – 95.9%.11 In the present study, the erythromycin-resistance rate of S. pneumoniae was high, at 96.75% (119 of 123), suggesting an increasing trend of pneumococcal erythromycin resistance in China. Similar to other studies in China,11,29 the resistance rate to trimethoprim–sulfamethoxazole (79.67%) of S. pneumoniae was also high in the current study, followed by tetracycline (77.23%) resistance. Insusceptibility rates of penicillin, amoxicillin, chloramphenicol, ceftriaxone, cefotaxime, and meropenem were 27.64%, 21.13%, 18.69%, 29.36%, 31.71%, and 48.78%, respectively. We found that all isolates were sensitive to vancomycin, linezolid, and levofloxacin.
Because of costs and lack of disease-burden data, the Chinese government has not adopted PCV in its national immunization program. PCV7 was approved by the Chinese Food and Drug Administration in 2008; however, uptake was low and concentrated in cities.30,31 The administration approved PCV13 for use in infants and children in a 3+1 schedule at 2, 4, and 6 months of age, with a fourth (booster) dose administered at approximately 12–15 months of age in 2016.31,32 However, PCV is currently available only for infants whose parents are able to pay for the vaccine. Studies have shown that PCV coverage was around 10% for children aged 2–7 years living in Shanghai, and locals had higher coverage than the floating population.30,33 In this study, non IPD children were taking PCV.
Several limitations exist in the present study. Firstly, the serotypes of S. pneumoniae isolates were not determined. Serotyping of pneumococcal isolates should be included in future investigations. Secondly, the sample size of our study was limited. More pneumococcal strains and study of isolates from other clinical specimens should be collected in future work.
Conclusion
S. pneumoniae is a pathogen that causes invasive diseases, particularly in young children. We found that the majority of the 123 identified IPD children were <5 years old. Clinical symptoms were severe in IPD children, and more intensive treatments were required for IPD children with sepsis and necrotizing pneumonia. Antimicrobial resistance tests of S. pneumoniae isolates found high insusceptible rates of erythromycin, trimethoprim–sulfamethoxazole, and tetracycline. All isolates were sensitive to vancomycin, linezolid, and levofloxacin. Pneumococcal vaccination is recommended, and intensive care should be considered for IPD children.
Abbreviations
ALB, albumin; ALT, alanine aminotransferase; CK-MB, creatine kinase muscle and brain type; CLSI, Clinical and Laboratory Standards Institute; CRP, C-reactive protein; CSF, cerebrospinal fluid; EBV, Epstein–Barr virus; Hb, hemoglobin; ICU, intensive care unit; IPD, invasive pneumococcal disease; IQR, interquartile range; IVIG, intravenous γ-globulin; Pct, procalcitonin; RSV, respiratory syncytial virus; WBCs, white blood cells
Author contributions
All authors contributed to conception and design of the study. KC, YW, and QZ analyzed and interpreted the data. YW and QZ drafted the manuscript. KC, YW, and ZG provided the study materials and selected patients. KC, XX, and HL collected and assembled data. All authors drafted the article or revised it critically for important intellectual content, approved the final manuscript, and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Acknowledgments
This work was supported by a grant from the National Natural Science Foundation of China (81500449). We acknowledge Yidu Cloud Technology Company Ltd for their contribution in the technology and data-platform support.
Disclosure
The authors report no conflicts of interest in this work.
References
O’Brien KL, Wolfson LJ, Watt JP, et al. Burden of disease caused by Streptococcus pneumoniae in children younger than 5 years: global estimates. Lancet. 2009;374(9693):893–902. | ||
Kadioglu A, Weiser JN, Paton JC, Andrew PW. The role of Streptococcus pneumoniae virulence factors in host respiratory colonization and disease. Nat Rev Microbiol. 2008;6(4):288–301. | ||
Berjohn CM, Fishman NO, Joffe MM, Edelstein PH, Metlay JP. Treatment and outcomes for patients with bacteremic pneumococcal pneumonia. Medicine. 2008;87(3):160–166. | ||
Chen CJ, Lin CL, Chen YC, et al. Host and microbiologic factors associated with mortality in Taiwanese children with invasive pneumococcal diseases, 2001 to 2006. Diagn Microbiol Infect Dis. 2009;63(2):194–200. | ||
Gómez-Barreto D, Espinosa-Monteros LE, López-Enríquez C, Jiménez-Rojas V, Rodríguez-Suárez R. Invasive pneumococcal disease in a third level pediatric hospital in Mexico City: epidemiology and mortality risk factors. Salud Publica Mex. 2010;52(5):391–397. | ||
Rückinger S, von Kries R, Siedler A, van der Linden M. Association of serotype of Streptococcus pneumoniae with risk of severe and fatal outcome. Pediatr Infect Dis J. 2009;28(2):118–122. | ||
Black RE, Cousens S, Johnson HL, et al. Global, regional, and national causes of child mortality in 2008: a systematic analysis. Lancet. 2010;375(9730):1969–1987. | ||
Rajaratnam JK, Marcus JR, Flaxman AD, et al. Neonatal, postneonatal, childhood, and under-5 mortality for 187 countries, 1970-2010: a systematic analysis of progress towards Millennium Development Goal 4. Lancet. 2010;375(9730):1988–2008. | ||
Liu Y, Wang H, Chen M, et al. Serotype distribution and antimicrobial resistance patterns of Streptococcus pneumoniae isolated from children in China younger than 5 years. Diagn Microbiol Infect Dis. 2008;61(3):256–263. | ||
Liu C, Xiong X, Xu W, Sun J, Wang L, Li J. Serotypes and patterns of antibiotic resistance in strains causing invasive pneumococcal disease in children less than 5 years of age. PLoS One. 2013;8(1): e54254. | ||
Xue L, Yao K, Xie G, et al. Serotype distribution and antimicrobial resistance of Streptococcus pneumoniae isolates that cause invasive disease among Chinese children. Clin Infect Dis. 2010;50(5):741–744. | ||
Zhang X, Tian J, Shan W, et al. Characteristics of pediatric invasive pneumococcal diseases and the pneumococcal isolates in Suzhou, China before introduction of PCV13. Vaccine. 2017;35(33):4119–4125. | ||
Christensen JS, Jensen TG, Kolmos HJ, Pedersen C, Lassen A. Bacteremia with Streptococcus pneumoniae: sepsis and other risk factors for 30-day mortality--a hospital-based cohort study. Eur J Clin Microbiol Infect Dis. 2012;31(10):2719–2725. | ||
Spencer DA, Thomas MF. Necrotising pneumonia in children. Paediatr Respir Rev. 2014;15(3):240–245. | ||
Tan TQ. Pediatric invasive pneumococcal disease in the United States in the era of pneumococcal conjugate vaccines. Clin Microbiol Rev. 2012;25(3):409–419. | ||
Wei L, Liu W, Zhang XA, et al. Detection of viral and bacterial pathogens in hospitalized children with acute respiratory illnesses, Chongqing, 2009-2013. Medicine. 2015;94(16):e742. | ||
Zhou L, Ma X, Gao W, et al. Molecular characteristics of erythromycin-resistant Streptococcus pneumoniae from pediatric patients younger than five years in Beijing, 2010. BMC Microbiol. 2012;12:228. | ||
Haddad MB, Porucznik CA, Joyce KE, et al. Risk factors for pediatric invasive pneumococcal disease in the Intermountain West, 1996–2002. Ann Epidemiol. 2008;18(2):139–146. | ||
Levine OS, Farley M, Harrison LH, Lefkowitz L, McGeer A, Schwartz B. Risk factors for invasive pneumococcal disease in children: a population-based case-control study in North America. Pediatrics. 1999;103(3):E28. | ||
Chiu NC, Chi H, Peng CC, et al. Retrospective study of prognostic factors in pediatric invasive pneumococcal disease. PeerJ. 2017;5:e2941. | ||
Launes C, de-Sevilla MF, Selva L, Garcia-Garcia JJ, Pallares R, Muñoz-Almagro C. Viral coinfection in children less than five years old with invasive pneumococcal disease. Pediatr Infect Dis J. 2012;31(6):650–653. | ||
Riva E, Salvini F, Garlaschi ML, Radaelli G, Giovannini M. The status of invasive pneumococcal disease among children younger than 5 years of age in north-west Lombardy, Italy. BMC Infect Dis. 2012;12:106. | ||
Ochoa TJ, Egoavil M, Castillo ME, et al. Invasive pneumococcal diseases among hospitalized children in Lima, Peru. Rev Panam Salud Publica. 2010;28(2):121–127. | ||
Shah AS, Nisarga R, Ravi Kumar KL, Hubler R, Herrera G, Kilgore PE. Establishment of population-based surveillance for invasive pneumococcal disease in Bangalore, India. Indian J Med Sci. 2009;63(11):498–507. | ||
Al Ayed MS, Hawan AA. Retrospective review of invasive pediatric pneumococcal diseases in a military hospital in the southern region of Saudi Arabia. Ann Saudi Med. 2011;31(5):469–472. | ||
Nicolaou EV, Bartlett AH. Necrotizing pneumonia. Pediatr Ann. 2017;46(2):e65–e68. | ||
Song JH, Jung SI, Ko KS, et al. High prevalence of antimicrobial resistance among clinical Streptococcus pneumoniae isolates in Asia (an ANSORP study. Antimicrob Agents Chemother. 2004;48(6):2101–2107. | ||
Zhao GM, Black S, Shinefield H, et al. Serotype distribution and antimicrobial resistance patterns in Streptococcus pneumoniae isolates from hospitalized pediatric patients with respiratory infections in Shanghai, China. Pediatr Infect Dis J. 2003;22(8):739–742. | ||
Chen J, Liu L, Wang G, et al. Correlation between usage of macrolide antibiotic and resistance of Streptococcus pneumoniae clinic isolates from Chongqing children’s hospital. Pediatr Pulmonol. 2009;44(9):917–921. | ||
Wagner AL, Sun X, Montgomery JP, Huang Z, Boulton ML. The impact of residency and urbanicity on Haemophilus influenzae Type b and pneumococcal immunization in Shanghai Children: a Retrospective Cohort Study. PLoS One. 2014;9(5):e97800. | ||
Shen K, Wasserman M, Liu D, et al. Estimating the cost-effectiveness of an infant 13-valent pneumococcal conjugate vaccine national immunization program in China. PLoS One. 2018;13(7):e0201245. | ||
Wu DB, Chaiyakunapruk N, Chong HY, Beutels P. Choosing between 7-, 10- and 13-valent pneumococcal conjugate vaccines in childhood: a review of economic evaluations (2006–2014). Vaccine. 2015;33(14):1633–1658. | ||
Boulton ML, Ravi NS, Sun X, Huang Z, Wagner AL. Trends in childhood pneumococcal vaccine coverage in Shanghai, China, 2005–2011: a retrospective cohort study. BMC Public Health. 2016;16:109. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


