Back to Journals » International Journal of Nephrology and Renovascular Disease » Volume 16
Clinical Application Value of Contrast-Enhanced Ultrasound in the Diagnosis of Renal Space-Occupying Lesions
Authors Liu Q, Gong H, Chen Q, Yuan C, Hu B
Received 16 September 2023
Accepted for publication 28 November 2023
Published 5 December 2023 Volume 2023:16 Pages 253—259
DOI https://doi.org/10.2147/IJNRD.S432436
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Pravin Singhal
Video abstract presented by Liu
Views: 93
Qiping Liu,1,* Huiling Gong,1,* Qiqi Chen,1 Chunyan Yuan,2 Bin Hu1
1Department of Ultrasound, Minhang Hospital, Fudan University, Shanghai, 201199, People’s Republic of China; 2Department of Pathology, Minhang Hospital, Fudan University, Shanghai, 201199, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Bin Hu; Chunyan Yuan, Email [email protected]; [email protected]
Objective: To study the clinical application value of contrast-enhanced ultrasound (CEUS) in diagnosing renal space-occupying lesions.
Methods: Sixty-seven patients with renal space-occupying lesions detected by routine ultrasound examination received the contrast-enhanced ultrasound examination. When observing the perfusion mode of the mass, we analyzed the perfusion characteristics of contrast-enhanced ultrasound and compared them with the surgical pathological results.
Results: Sixty-seven lesions, which were identified in 67 patients with renal space-occupying lesions, included 55 renal malignant tumors and 12 benign ones. The sensitivity of qualitative diagnosis by CEUS imaging was 96.4%, the specificity was 66.7%, and the accuracy was 91.0%.
Conclusion: The real-time blood supply of renal space-occupying lesions helps judge their nature according to the enhancement mode. It has high clinical application value in diagnosing benign and malignant lesions.
Keywords: ultrasound examination, renal lesions, contrast-enhanced ultrasound
The renal tumor is a common tumor in the urinary system, usually without obvious clinical symptoms, and most of them are malignant. Ultrasound examination is the primary imaging method for clinically screening renal space-occupying lesions. It is of great clinical significance to find and judge the benign and malignant renal space-occupying lesions.1 Contrast-enhanced ultrasound has been used in studying multiple organs and has also made much progress in the application of renal space-occupying lesions.2
Contrast-enhanced ultrasound can help to dynamically observe the microvascular perfusion process of the lesions in real-time, which is of great significance in the diagnosis and differential diagnosis of benign and malignant renal lesions and has also become a vital imaging method for the evaluation of renal space-occupying lesions.3–5
By observing the septa’s blood supply and thickness, CEUS can perceive a difference between solid and cystic lesions, and even simple cysts and complicated cysts. As for this, it may improve the diagnostic accuracy of renal space-occupying lesions and provide a low-cost, acceptable alternative solution.
While we noted such consequences with concern, 67 patients with 67 lesions confirmed renal space-occupying lesions by surgery were analyzed retrospectively at the Minhang Hospital affiliated with Fudan University over the past decade. Contrast-enhanced ultrasound was applied in examining renal space-occupying lesions. Summarizing the perfusion mode of contrast-enhanced ultrasound and analyzing its perfusion characteristics, we will explore the clinical application value of CEUS in diagnosing renal space-occupying lesions.
Data and Methods
General Information
We collected 67 patients with all single renal space-occupying lesions by routine ultrasound examination in Minhang Hospital affiliated with Fudan University from July 2013 to June 2022. There were 48 males, 19 females, 32 right renal lesion cases, and 35 left renal ones. The ages ranged from 31 to 81 (60 years old on average). CEUS was performed in all 67 lesions. Inclusion criteria:1) To have received both routine and contrast-enhanced ultrasound; 2) With complete material; 3) Not allergic to contrast agent. Exclusion criteria: 1) Allergic to contrast agent or having severe cardiopulmonary dysfunction; 2) Under 18 years old. This retrospective study was conducted following the Declaration of Helsinki and the Declaration of Istanbul. All procedures were approved by the Institutional Review Board at Minhang Hospital, Fudan University. Informed consent was obtained from all patients at the time of their examinations.
Instruments and Methods
Four types of ultrasonic scanners (Aplio i900, Canon, Japan; Aplio 500, Canon, Japan; SSA-790A (AplioXG), Canon, Japan; Resona 7s, Mindray, China) with 1–6 MHz linear transducers and CEUS modules equipped were in use. First, we observed the location, shape, size, echo, number of kidney tumors, surrounding adjacent tissue demarcation, and blood flow condition through routine ultrasound from multiple sections and angles. Then, we switched it to CEUS mode and selected SonoVue as the contrast agent. 5 mL of normal saline was injected before use, and 1.2–1.8 mL of the mixture was extracted after shaking. When displaying the best section of the lesion, we injected the mixture rapidly through the cubital vein, followed by 5 mL of normal saline, and started the timer simultaneously. After the injection, we observed the image continuously for 3–6 min. All the images are archived for offline analysis.
The playback clips were repeatedly reviewed by 2–3 experienced sonographers who had not acquired the pathological results before. The contrast agent changes in the mass were observed dynamically. The perfusion patterns were summarized in terms of enhancement time, intensity, and degree of uniformity, and we analyzed the perfusion characteristics.
Qualitative analysis indexes: ① Enhancement time, compared with the surrounding normal renal cortex, included fast-in, synchronous-in, and slow-in; ② Washout time, compared with the surrounding normal renal cortex, included fast-out, synchronous-out, and slow-out; ③ Enhancement intensity, compared with the surrounding normal renal cortex, included hyperenhancement, isoenhancement, hypoenhancement, and non-enhancement; ④ The homogeneity of perfusion; ⑤ Whether there was a peritumoral hyper-enhanced rim (PHR) sign, which is defined as the appearance of ring-shaped enhancement at the periphery of a renal tumor during the CEUS process, significantly brighter than that of the normal renal cortex in and around the kidney.6 Finally, the medical history and surgical pathology data were followed up for contrast.
Statistical Analysis
All statistical analyses were performed by SPSS version 19.0 (SPSS, Inc, Chicago, IL), and comparisons between the enumeration data were done by the chi-square test. P < 0.05 was considered statistically significant.
Results
Basic Pathological Results of the Lesions
All renal space-occupying lesions were pathologically confirmed after surgery. 55 of the 67 lesions were malignant, including 52 renal clear cell carcinomas (77.6%), one renal papillary carcinoma (1.5%), one acquired cystic disease-associated renal cell carcinoma (1.5%), one transcription factor E3 (TFE3) gene-translocation renal cell carcinoma (1.5%); The rest 12 patients were benign, including eight renal angiomyolipomas (11.9%), and four renal oncocytomas (6.0%). The sensitivity of CEUS in the qualitative diagnosis of renal space-occupying lesions was 96.4%, specificity was 66.7%, and accuracy was 91.0% (Table 1).
 |
Table 1 Comparison Between CEUS and Pathological Findings |
CEUS Findings
Renal Malignant Tumors
① Of all the 52 cases of renal clear cell carcinoma in CEUS, 29 showed fast-in, 13 synchronous-in, and 10 slow-in. Regarding washout time, 22 cases showed fast-out, 13 synchronous-out, and 20 slow-out. Concerning the enhancement intensity, 29 cases showed hyperenhancement, 15 isoenhancement, and eight hypoenhancement. 35 cases had heterogeneous enhancement and 17 had homogeneous enhancement (Figure 1). ② One case of renal papillary carcinoma showed fast-in, fast-out, heterogeneous isoenhancement. ③ One case of acquired cystic disease-associated renal cell carcinoma (RCC) showed synchronous-in, fast-out, heterogeneous hyperenhancement. ④ One case of TFE3 gene-translocation RCC showed fast-in, fast-out, heterogeneous hyperenhancement.
 |
Figure 1 A female patient with renal clear cell carcinoma (arrows) under CEUS (dual layout). (A) Fast-in at 7th sec. (B) Heterogeneous hyperenhancement at 20th sec. (C) Slow-out at 124th sec. |
Renal Benign Tumors
① Of the eight cases of renal angiomyolipomas, six showed slow-in, two synchronous-in. When it came to washout time, five cases showed synchronous-out, two slow-out, and one fast-out. Concerning the enhancement intensity, seven cases showed isoenhancement and one hypoenhancement. Five cases had homogeneous enhancement, and three had heterogeneous enhancement (Figure 2). ② Of the four cases of renal oncocytomas, two showed fast-in, one synchronous-in, and one slow-in. When it came to washout time, two cases showed slow-out, one synchronous-out, and one fast-out. Concerning the enhancement intensity, one case showed hyperenhancement, two isoenhancement, and one hypoenhancement. Three cases had homogeneous enhancement and one had heterogeneous enhancement.
 |
Figure 2 A male patient with renal angiomyolipomas (arrows) under CEUS (dual layout). (A) Synchronous-in at 11th sec. (B) Heterogeneous isoenhancement at 14th sec. (C) Synchronous-out at 69th sec. |
From statistical analysis, renal malignant tumors had features about fast-in, fast-out, slow-out, hyperenhancement, and heterogeneous enhancement. In contrast, benign ones had features about slow-in, synchronous-out, slow-out, isoenhancement, hypoenhancement, and homogeneous enhancement (Table 2).
 |
Table 2 Comparison Between Benign and Malignant Space-Occupying Tumors of Kidney on CEUS |
Findings of PHR Sign of Renal Tumors
24 of 55 malignant tumors had PHR signs, and the rest did not have them; 1 of 12 benign tumors had PHR signs, and the rest did not have them (Table 3).
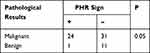 |
Table 3 PHR Sign of the Renal Tumors |
Discussion
Currently, the imaging methods on renal space-occupying lesions mainly cover routine ultrasound, CT, MRI, etc. CEUS has advantages in effectively reflecting the blood flow perfusion inside the lesions and is real-time and non-radiative. All of the above on CEUS makes up for the deficiency of routine ultrasound, CT, MRI, and other examinations in the differential diagnosis of renal space-occupying lesions nowadays. It offers valuable diagnostic information for clinical use.7 CEUS is a new technology developed in recent years to display the perfusion in the tissue objectively. By microbubbles of contrast agents, it is possible to visualize the microvessels and nourishing vessels of tumors and to display the distribution of blood flow in and around the lesion. SonoVue, a novel ultrasound contrast agent, is a blood pool tracer. It is restricted in the vessel, enabling dynamic microcirculation perfusion observation in real time.8
RCC is the most common tumor, accounting for 80–90% of all renal malignant tumors. Clear cell carcinoma is the most common type of RCC.3 The CEUS performance of RCC is related to factors such as tumor internal angiogenesis density, vascular diameter, tortuosity, and arteriovenous fistula. In this study, 31 of 55 renal carcinomas showed fast-in, and 30 showed hyperenhancement, which is in keeping with the literature reporting that the CEUS performance of renal cancer is mostly fast-in and hyperenhanced.3,9,10
In 24 of 55 cases of renal cancer in this group, a PHR sign was found during the CEUS process. The pathological basis of PHR detection derives from the rich vascular components around renal cancer. PHR is related to the identification, staging, and surgical scheme selection of benign and malignant tumors, which is of great significance for clinical diagnosis and treatment.11 Some researchers discovered that when the edge of incisions was negative, it was no longer necessary to restrict the width of the normal kidney tissue above tumors for excision. The psedocapsule, generally recognized, is a security boundary between the tumor and normal tissue. A complete psedocapsule usually means an early phase of the tumor with low aggressiveness, and it reduces the possibility of infiltration and metastasis of tumors to some extent. Additionally, the psedocapsule is easy to separate from the normal renal tissue. Based on the above characteristics, tumor enucleation (TE), a urological surgical procedure that allows surgeons to keep the adjacent normal tissue and integrally remove the tumor along with its psedocapsule, is adopted clinically.12,13
38 of 55 renal cancers in this group showed heterogeneous enhancement, and 17 showed homogeneous enhancement in CEUS. It can clearly show the non-enhanced areas of liquefaction and necrosis in the whole process of CEUS, which helps judge the tumor’s nature. The most probable reason for that is the rapid growth rate of malignant tumors, which often appear as internal liquefaction necrosis, hemorrhage, or cystic changes. If there are smaller tumors, it is challenging to observe internal small cystic changes, liquefaction, or necrosis by conventional 2D ultrasound, but CEUS is able to do so.
Angiomyolipoma is the most common benign renal tumor, and the ultrasound examination manifestation is up to the proportion of blood vessels, smooth muscle, and fat. Tumors consisting of fat are the most common, which is hyperechoic and easy to diagnose. Tumors consist of hypoechoic vascular smooth muscle, which is usually mistaken for renal cancers. Angiomyolipomas are divided into two types: fast-in, slow-out and slow-in, slow-out on CEUS.14 In this study, there were eight angiomyolipomas examined by CEUS. Three cases showed slow-in and synchronous-out, two showed slow-in and slow-out, two showed synchronous-in and synchronous-out, and one showed slow-in and fast-out. It was consistent with reports in the literature.14 Renal oncocytoma is a relatively rare benign tumor of the renal parenchyma, accounting for 3–7% of renal tumors.15 Through ultrasound, the lesion of renal oncocytoma is able to be seen in the renal parenchyma, and it is mainly solid, slightly hyperechoic, circular or oval, of clear boundary, and regular blood flow signal in the periphery. A few lesions have cystic structures.16 It can present as a fast-in, slow-out enhancement, and hyperechoic ring17 around the lesion during the delay phase or hyperenhancement and delayed washout.18 In this study, there was one case of hyperenhancement and surrounding hyperenhancement ring, one case of fast-in and fast-out, one case of slow-in and slow-out, and one case of synchronous-in and synchronous-out, which is consistent with the literature.15,16 It is so easily confused with renal cancer that we should pay more attention to identification clinically in order not to misdiagnose it.
In summary, CEUS has the advantages of easy-to-do, inexpensiveness, and non-radiation. It makes it possible to observe the blood perfusion of renal space-occupying lesions in real time. It can more clearly show the outline and extent of the lesions and improve the visualization rate of pseudocapsule and necrosis areas. It is also precious for the diagnosis of renal space-occupying diseases to differentiate the malignant from the benign. As we step deeper into the domain of CEUS, more ingenious usages that we have never considered may be discovered. It will be available to add CEUS into routine clinical practice if more and more practitioners are familiar with its function and application. Due to the small number of cases in this study, it is necessary to expand the sample capacity to discover laws that we may not find in the study and improve the diagnostic accuracy rate of CEUS on renal space-occupying lesions. Furthermore, it can play a significant role in staging renal tumors preoperatively and precisely.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethical Consideration
This study was approved by the institutional review board of Minhang Hospital, Fudan University. This study compiles with the Declaration of Helsinki.
Funding
Natural Science Foundation of Minhang District, Shanghai (2021MHZ095).
Disclosure
No potential conflict of interest was reported by the authors.
References
1. Zarzour JG, Lockhart ME, West J, et al. Contrast-enhanced ultrasound classification of previously indeterminate renal lesions. J Ultrasound Med. 2017;36(9):1819–1827. doi:10.1002/jum.14208
2. Miele V, Piccolo CL, Sessa B, Trinci M, Galluzzo M. Comparison between MRI and CEUS in the follow-up of patients with blunt abdominal trauma managed conservatively. Radiol Med. 2016;121(1):27–37. doi:10.1007/s11547-015-0578-1
3. Yanagi M, Kiriyama T, Akatsuka J, et al. Differential diagnosis and prognosis of small renal masses: association with collateral vessels detected using contrast-enhanced computed tomography. BMC Cancer. 2022;22(1):856. doi:10.1186/s12885-022-09971-w
4. Rübenthaler J, Negrão de Figueiredo G, Mueller-Peltzer K, Clevert DA. Evaluation of renal lesions using contrast-enhanced ultrasound (CEUS); a 10-year retrospective European single-centre analysis. Eur Radiol. 2018;28(11):4542–4549. doi:10.1007/s00330-018-5504-1
5. Dietrich CF, Nolsøe CP, Barr RG, et al. Guidelines and good clinical practice recommendations for Contrast-Enhanced Ultrasound (CEUS) in the liver-update 2020 WFUMB in cooperation with EFSUMB, AFSUMB, AIUM, and FLAUS. Ultrasound Med Biol. 2020;46(10):2579–2604. doi:10.1016/j.ultrasmedbio.2020.04.030
6. Mukherjee A, Madamsetty VS, Paul MK, Mukherjee S. Recent advancements of nanomedicine towards antiangiogenic therapy in cancer. Int J Mol Sci. 2020;21(2):455. doi:10.3390/ijms21020455
7. Cai Y, Li F, Li Z, et al. Predictive value of contrast-enhanced ultrasound combined with conventional ultrasound in solid renal parenchymal lesions. Br J Radiol. 2021;94(1125):20210518. doi:10.1259/bjr.20210518
8. Sun Y, Xiong X, Pandya D, et al. Enhancing tissue permeability with MRI guided preclinical focused ultrasound system in rabbit muscle: from normal tissue to VX2 tumor. J Control Release. 2017;256:1–8. doi:10.1016/j.jconrel.2017.04.017
9. Bertelli E, Palombella A, Sessa F, et al. Contrast-enhanced ultrasound (CEUS) imaging for active surveillance of small renal masses. World J Urol. 2021;39(8):2853–2860. doi:10.1007/s00345-021-03589-6
10. Olson MC, Abel EJ, Mankowski Gettle L. Contrast-enhanced ultrasound in renal imaging and intervention. Curr Urol Rep. 2019;20(11):73. doi:10.1007/s11934-019-0936-y
11. Pan KH, Jian L, Chen WJ, et al. Diagnostic performance of contrast-enhanced ultrasound in renal cancer: a meta-analysis. Front Oncol. 2020;10:586949. doi:10.3389/fonc.2020.586949
12. Bensalah K, Pantuck AJ, Rioux-Leclercq N, et al. Positive surgical margin appears to have negligible impact on survival of renal cell carcinomas treated by nephron-sparing surgery. Eur Urol. 2010;57(3):466–471. doi:10.1016/j.eururo.2009.03.048
13. Berdjis N, Hakenberg OW, Zastrow S, Oehlschläger S, Novotny V, Wirth MP. Impact of resection margin status after nephron-sparing surgery for renal cell carcinoma. BJU Int. 2006;97(6):1208–1210. doi:10.1111/j.1464-410X.2006.06157.x
14. Cao H, Fang L, Chen L, et al. The independent indicators for differentiating renal cell carcinoma from renal angiomyolipoma by contrast-enhanced ultrasound. BMC Med Imaging. 2020;20(1):32. doi:10.1186/s12880-020-00436-9
15. Schwarze V, Marschner C, Negrão de Figueiredo G, Knösel T, Rübenthaler J, Clevert DA. Single-center study: the diagnostic performance of contrast-enhanced ultrasound (CEUS) for assessing renal oncocytoma. Scand J Urol. 2020;54(2):135–140. doi:10.1080/21681805.2020.1736621
16. Geyer T, Schwarze V, Marschner C, et al. Diagnostic performance of Contrast-Enhanced Ultrasound (CEUS) in the evaluation of solid renal masses. Medicina. 2020;56(11):624. doi:10.3390/medicina56110624
17. Wu Y, Du L, Li F, Zhang H, Cai Y, Jia X. Renal oncocytoma: contrast-enhanced sonographic features. J Ultrasound Med. 2013;32(3):441–448. doi:10.7863/jum.2013.32.3.441
18. Galmiche C, Bernhard JC, Yacoub M, Ravaud A, Grenier N, Cornelis F. Is multiparametric MRI useful for differentiating oncocytomas from chromophobe renal cell carcinomas? AJR Am J Roentgenol. 2017;208(2):343–350. doi:10.2214/AJR.16.16832
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
