Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 15
Chronic Cough and Phlegm in Subjects Undergoing Comprehensive Health Examination in Japan – Survey of Chronic Obstructive Pulmonary Disease Patients Epidemiology in Japan (SCOPE-J)
Authors Omori H , Higashi N, Nawa T, Fukui T, Kaise T , Suzuki T
Received 6 November 2019
Accepted for publication 21 March 2020
Published 15 April 2020 Volume 2020:15 Pages 765—773
DOI https://doi.org/10.2147/COPD.S237568
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Hisamitsu Omori,1 Noritaka Higashi,2 Takeshi Nawa,3 Toshiki Fukui,4 Toshihiko Kaise,5 Takeo Suzuki5
1Department of Biomedical Laboratory Sciences, Faculty of Life Sciences, Kumamoto University, Kumamoto, Japan; 2Japanese Red Cross Kumamoto Health Care Center, Kumamoto, Japan; 3Department of Internal Medicine, Hitachi General Hospital, Hitachi, Japan; 4Center for Preventive Medical Treatment, Olive Takamatsu Medical Clinic, Takamatsu, Japan; 5Japan Development Division, GlaxoSmithKline K.K., Tokyo, Japan
Correspondence: Toshihiko Kaise
Japan Development Division, GlaxoSmithKline K.K., 1-8-1 Akasaka, Minato-ku, Tokyo 107-0052, Japan
Tel +81 80 5927 9500
Fax +81 3 4231 5993
Email [email protected]
Purpose: The purpose of this study was to estimate the prevalence of subjects with chronic cough and phlegm and describe their characteristics including the presence or absence of airflow limitation among the general population in Japan.
Subjects and Methods: This was an observational cross-sectional survey targeting multiple regions of Japan. Subjects aged 40 years or above who were undergoing comprehensive health examination were recruited. The existence of chronic cough and phlegm, airflow limitation, and treatment for respiratory diseases were examined. Chronic cough and phlegm were defined as having both symptoms for at least 3 months of the year and for at least 2 consecutive years, or as receiving any treatment for chronic bronchitis at the time of recruitment. Airflow limitation was defined as forced expiratory volume in 1 s/forced vital capacity (FEV1/FVC) less than 0.7.
Results: In a total of 22,293 subjects, 380 subjects (1.7%) had chronic cough and phlegm. Among these 380 subjects, 21.8% received treatment for a respiratory disease, and 11.6% had airflow limitation. Compared to subjects without both chronic cough and phlegm but with airflow limitation, subjects with chronic cough and phlegm without airflow limitation were younger, more likely to be current smokers (39.6%), and had higher total scores on a chronic obstructive pulmonary disease (COPD) assessment test (CAT). Scores of CAT questions 1– 4 (cough, phlegm, chest tightness, breathlessness, respectively) were higher in subjects with chronic cough and phlegm regardless of airflow limitation.
Conclusion: This study demonstrated that subjects identified to have chronic cough and phlegm in comprehensive health examination settings were symptomatic, while most of them did not receive any treatment for respiratory diseases and did not have airflow limitation. Screening subjects for chronic cough and phlegm in a comprehensive health examination followed by a detailed examination of screened subjects could be an effective approach for better management of chronic cough and phlegm. Smoking cessation should be included in the management, in consideration that around 40% of subjects with chronic cough and phlegm were current smokers.
Keywords: respiratory disease, chronic bronchitis, spirometry, lung function, general population, health checkup
Introduction
Since 2013, the second term of Health Japan 21 has aimed to prevent the onset and progression of lifestyle-related diseases. Chronic obstructive pulmonary disease (COPD), cancer, circulatory diseases, and diabetes mellitus were selected as target diseases.1 One goal was to improve COPD awareness to 80% by 2022, but awareness was still low (28.1%) in the 2018 survey.2 COPD is often understood as a generic term for emphysema and chronic bronchitis, but COPD is a physiologically defined disease and airflow limitation determined by spirometry is mandatory for its diagnosis. On the other hand, emphysema is a pathomorphologically defined disease with destruction of the alveolar walls, whereas chronic bronchitis is a symptomatologically defined disease with persistent cough and phlegm.3–6 Such complexities may make the individual conditions of COPD difficult to understand.
Non-obstructive chronic bronchitis with persistent cough and phlegm can cause exacerbation and impair activities of daily living, and therefore has recently attracted attention.7–12 Non-obstructive chronic bronchitis could be left undiagnosed owing to lack of airflow limitation, and approaches are needed for better management. Several previous studies have shown the prevalence of chronic cough and phlegm,7–12 which are typical symptoms of chronic bronchitis, however the prevalence of airflow limitation among subjects with chronic cough and phlegm has scarcely been examined. In the present study, we aimed to estimate the prevalence of chronic cough and phlegm among the general population, and to describe their characteristics including the presence or absence of airflow limitation. This approach could provide additional information about the characteristics of chronic cough and phlegm and of non-obstructive chronic bronchitis.
Subjects and Methods
Study Design and Participants
This was a follow-up study to SCOPE-J (Survey of Chronic Obstructive pulmonary disease Patients Epidemiology in Japan),13 a prospective, multicenter, cross-sectional, observational study. Fourteen sites participated from the following regions in Japan: five in Kanto, one in Chubu, two in Kinki, three in Chugoku/Shikoku, and three in Kyushu. The following items were investigated in Ningen Dock (comprehensive health examination in Japanese) examinees aged 40 years or older: age, sex, height, body weight, smoking habit/index, lung function, high-sensitivity C-reactive protein (CRP) level, fasting blood glucose level, hemoglobin A1c value, cough/phlegm symptoms, diagnosis history/current treatment status for respiratory diseases (chronic bronchitis, emphysema, COPD, bronchial asthma, diffuse panbronchiolitis, bronchiectasis, pneumonia, pulmonary tuberculosis, pulmonary fibrosis, lung abscess, and pneumoconiosis) and comorbidities (myocardial infarction, angina pectoris, cerebrovascular disease, osteoporosis, fracture, depression, anxiety disorder, sleep disorder, diabetes mellitus, and lung cancer), and chronic obstructive pulmonary disease assessment test (CAT) findings.14
The protocol was approved by the Ethics Committee of the Faculty of Life Sciences, Kumamoto University (Number 575) and the study was conducted in accordance with the Declaration of Helsinki and the Ethical Guidelines for Epidemiological Research (partially revised on December 1, 2008 by the Ministry of Education, Culture, Sports, Science and Technology and the Ministry of Health, Labor and Welfare). Examinees who gave written informed consent were included in the study.
Procedures
Chronic cough and phlegm were defined as having both symptoms for at least 3 months of the year and for at least 2 consecutive years,15 or receiving any treatment for chronic bronchitis at the time of recruitment. Quality control and spirometer calibration were performed in accordance with previously published recommendations.16 All study sites were members of the Japan Society of Ningen Dock and performed standardized and high-quality spirometry. The airway reversibility test by bronchodilator inhalation was not performed, since the purpose of the health examination was screening and not establishing a definitive diagnosis. Airflow limitation was defined as [forced expiratory volume in 1 s]/[forced vital capacity] (FEV1/FVC) less than 0.7. The predictive values of lung function were calculated using the predictive equation reported by the Japanese Respiratory Society (male: FEV1 [L] = 0.036 × height [cm] −0.028 × age −1.178, female: FEV1 [L] = 0.022 × height [cm] −0.022 × age −0.005; male: FVC [L] = 0.042 × height [cm] −0.024 × age- 1.185, female: FVC [L] = 0.031 × height [cm] −0.019 × age −1.105).17
Statistical Analysis
Demographics, clinical characteristics, and presence of comorbidities of the subjects were tabulated by presence or absence of both chronic cough and phlegm. For comorbidities, the number and proportion of subjects who were on a given treatment at the time of the health examination were summarized (lung cancer was regarded as present if a subject had history of lung cancer, regardless of current treatment). The prevalence of chronic cough and phlegm was calculated by sex, age group, and smoking history. The subjects were divided into four groups according to the presence or absence of chronic cough and phlegm and airflow limitation (Group 1: without either chronic cough and phlegm or airflow limitation, Group 2: with chronic cough and phlegm only [without airflow limitation], Group 3: with airflow limitation only [without chronic cough or phlegm], and Group 4: with both chronic cough and phlegm and airflow limitation) and demographics, lung function, and CAT scores were shown. To investigate characteristics of subjects with chronic cough and phlegm in comparison with subjects with airflow limitation, Groups 2 (with chronic cough and phlegm only) and 3 (with airflow limitation only) were compared as post hoc analysis. For categorical data, the number of subjects in each category was tabulated and a chi-squared test was performed. For continuous data, means and standard deviations (SD) were calculated, and the Wilcoxon rank-sum test was performed after checking normality. For CAT scores, means for responses to each question were also calculated. Respiratory disease treatment status and existence of airflow limitation in subjects with chronic bronchitis were shown. Statistical analyses were performed using R version 2.15.2 software (R Foundation for Statistical Computing, Vienna, Austria).
Results
A total of 22,293 examinees was enrolled between December 2012 and August 2013, and the number of subjects with both chronic cough and phlegm was 380 (1.7%). Table 1 shows the characteristics of subjects with or without chronic cough and phlegm, and the total study population. The proportion of current smokers was higher in subjects with chronic cough and phlegm (41.8%) compared to those without (18.8%).
 |
Table 1 Characteristics of the Subjects |
Table 2 shows the prevalence of chronic cough and phlegm by smoking history, sex, and age group. Since 100 subjects lacked smoking history data, 22,193 subjects with smoking history were included in the table. The prevalence of chronic cough and phlegm among subjects aged over 60 years (2.2%) was higher than in those aged 40–49 years (1.3%) and 50–59 years (1.7%). Males had higher prevalence (2.1%) than females (1.1%). The prevalence by smoking history showed that it was more prevalent among current smokers (3.7%) than past smokers (1.4%) or never-smokers (1.1%).
 |
Table 2 Prevalence of Chronic Cough and Phlegm by Smoking History, Sex, and Age Group (for Subjects with Smoking Data Only) |
Table 3 shows the presence or absence of treatment for any respiratory disease and airflow limitation in 380 subjects with chronic cough and phlegm. Among the subjects, 21.8% were receiving treatment for any respiratory disease and 11.6% showed airflow limitation.
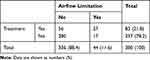 |
Table 3 Presence or Absence of Treatment for Any Respiratory Diseases and Airflow Limitation in Subjects with Chronic Cough and Phlegm |
Table 4 shows the characteristics of four sub-groups among subjects defined by existence of chronic cough and phlegm, and airflow limitation. When Group 2 (with chronic cough and phlegm only) was compared with Group 3 (with airflow limitation only), Group 2 was younger, had more females, higher body mass index (BMI), more current smokers (39.6% vs 25.5%), lower smoking index, higher FEV1, higher %FEV1, higher FEV1/FVC, and higher total CAT score compared with Group 3.
 |
Table 4 Characteristics of Subjects in Four Groups According to the Presence or Absence of Chronic Cough and Phlegm, and Airflow Limitation |
Figure 1 shows the mean CAT scores in each item by group for four groups. Group 2 showed higher scores on responses to Questions 1 (cough), 2 (phlegm), 3 (chest tightness) and 4 (breathlessness) than Group 3.
Discussion
Our study evaluated the presence or absence of airflow limitation and treatment among subjects with chronic cough and phlegm (Table 3). Subjects without airflow limitation comprised 88.4% and those without treatment made up 78.2%. Among those without treatment, the proportion of subjects without airflow limitation was as high as 94.3% (280/297). One of the reasons for the low treatment rate could be the absence of recommendation for further examination if a subject is identified to have chronic cough and phlegm in comprehensive health examination. On the other hand, if a subject has airflow limitation or decreased vital capacity in comprehensive health examination, follow-up consultation is requested.18 Thus recommendation of follow-up examination with explanation of benefits of early consultation19 could be an effective approach for better management of chronic cough and phlegm regardless of whether airflow limitation exists or not.
Patients with asthma or bronchiectasis are known to present chronic cough and phlegm as common symptoms.20 Adachi et al examined symptoms among asthma patients being managed by specialists in Japan, and found that 44.5% of the patients presented cough in the daytime and 56.9% had phlegm.21 In our study, subjects with asthma or bronchiectasis as well as those with chronic bronchitis may have contributed to the number of subjects with both chronic cough and phlegm. In fact, 12.6% (48/380) and 3.4% (13/380) of subjects with chronic cough and phlegm in our study were being treated for asthma and bronchiectasis, respectively, at the time of the recruitment, while corresponding proportions among the subjects without chronic cough and phlegm were only 1.2% (266/21,293) and 0.1% (11/21,293).
The proportion of examinees with airflow limitation among subjects with chronic cough and phlegm was 11.6% in our study. A previous report from Japan showed that 47.2% of the patients with chronic bronchitis had airflow limitation,22 although the target population was outpatients who needed treatment and thus was different from our target population. In our study and the previous report,22 male proportion was 77.1% and 76.1%, age was 56.7 ± 9.7 (mean ± SD) and 65.7 ± 12.6, and smoking amount was 19.7 and >30 pack-years, respectively. Younger age distribution and smaller smoking amount in our study may have resulted in smaller proportion of airflow limitation among chronic cough and phlegm, since both older age and larger smoking amount were associated with higher proportion of airflow limitation.22
Our study also showed that the age of the subjects with chronic cough and phlegm only was younger than that of the airflow limitation only group, and the proportion of females was also higher. In a previous study comparing COPD phenotypes, patients with chronic bronchitis only had a younger age (mean ± SD) of 51.4 ± 14.8 years, than COPD only (63.2 ± 10.9) and emphysema only (63.3 ± 13.3),23 suggesting that cough and sputum develop from a younger age than airflow limitation. It was also reported in that previous report that the proportion of females was as high as 63.2% in chronic bronchitis only (42.4% in COPD only and 37.8% in emphysema only). In comparisons between males and females with COPD after matching by FEV1, Saint George’s Respiratory Questionnaire scores were worse in females than in males despite a lower smoking index and a milder level of gas-exchange impairment in females,24 suggesting that females with COPD are more symptomatic. The proportion of females among patients with COPD was higher in the airway-lesion-predominant type than in the emphysema-lesion-predominant type,25 which suggests that females tend to have chronic-bronchitis-type rather than pulmonary-emphysema-type COPD.
In our study, the proportion of never-smokers in subjects with chronic cough and phlegm was 32.7%. In the previous report,22 the proportion of never-smokers was 21.3% in patients with chronic bronchitis. Passive smoking, air pollution, infection, allergy, and aging were considered as potential explanations for chronic cough and phlegm or chronic bronchitis among never-smokers.26
In our study, the mean total CAT score of subjects with chronic cough and phlegm was more than 10 regardless of having airflow limitation. The presence of chronic bronchitis in patients with COPD has been reported to be associated with a poor prognosis, such as frequent exacerbation or rapid decline in lung function.27–30 In addition, chronic bronchitis without COPD has also been reported to be associated with higher risk of poor prognosis. Patients with non-obstructive chronic bronchitis as well as those with COPD had lower activities of daily living and exercise levels than the general population.7 Cognitive deterioration was observed not only in patients with COPD, but also in patients with chronic bronchitis without airflow limitation.31 It was reported that a group with chronic cough and phlegm had a higher risk of developing COPD than a group without symptoms in a follow-up of subjects aged 20 to 44 years without an asthma diagnosis and without airflow limitation.32 Taken together, chronic bronchitis or chronic respiratory symptoms can be associated with poor prognosis even without COPD or airflow limitation.
In our study, Group 2 had higher CAT scores than Group 3, which suggests that assessment of symptoms is important in addition to airflow limitation. Martinez et al investigated the usefulness of the first four questions of CAT (cough, phlegm, chest tightness, and breathless) to assess risk in ever-smokers with normal lung function and reported that responses to the first four questions out of the total eight questions were able to identify high-risk patients.33 CAT scores for patients with chronic-bronchitis-type and chronic-bronchitis-free-type COPD were investigated, and they were higher for responses to all of the eight questions in chronic-bronchitis-type, although there were no differences in lung function.34
Since the proportion of current smokers was high (41.8%) among subjects with chronic cough and phlegm, smoking cessation is necessary in addition to medical treatment. The proportion of subjects who attempted to quit smoking in the past year was 23.0% in Japan,35 which was lower than that in the United Kingdom36 and the United States.37 The most common reasons for wanting to quit smoking in current smokers was the cost of smoking, and the lower cost of smoking in Japan38 may be one of the reasons for the high percentage of current smokers in our study. Another possible reason is a limited use of medication for smoking cessation39 resulting in smoking cessation failure.
A strength of our study is that we prospectively included more than 22,000 examinees at multiple sites in multiple regions in Japan. By this prospective study design, we could evaluate the presence of chronic cough and phlegm using a questionnaire. All participating sites were members of the Japan Society of Ningen Dock, and the quality of spirometry was high and standardized. Some important limitations of our study were as follows. Since the age and sex distribution of comprehensive health examinees and the general population are not the same, care is needed in extrapolating the results. Because we measured only pre-bronchodilator airflow limitation, care is needed when comparing our results with those of other studies with post-bronchodilator airflow limitation. Chronic cough and phlegm are typical symptoms of chronic bronchitis, but subjects with chronic cough and phlegm may include those with diseases other than chronic bronchitis including asthma, bronchiectasis, non-tuberculous mycobacteriosis and sinobronchial syndrome. Other than respiratory diseases, gastroesophageal reflux disease (GERD) is reported to affect chronic cough and phlegm,40 but we did not collect data of comorbid GERD in this study. Information on medications was not available, since only the presence or absence of treatment for some diseases are investigated by self-reported questionnaires in health examinations, and records of medical treatment in primary and advanced care are not linked with health examination data. No information on passive smoking or environmental factors (such as occupational factors and air pollution) were obtained.
Conclusions
This study demonstrated that subjects identified to have chronic cough and phlegm in comprehensive health examination settings were symptomatic, while most of them did not receive any treatment for respiratory diseases and did not have airflow limitation. Screening subjects for chronic cough and phlegm in comprehensive health examinations followed by a recommendation of detailed examination for screened subjects could be an effective approach for better management of chronic cough and phlegm. Smoking cessation should be included in the management, in consideration that around 40% of subjects with chronic cough and phlegm were current smokers.
Abbreviations
AL, airflow limitation; BMI, body mass index; CAT, chronic obstructive pulmonary disease assessment test; CRP, c-reactive protein; COPD, chronic obstructive pulmonary disease; FEV1, forced expiratory volume in 1 s; FVC, forced vital capacity; SD, standard deviation; SCOPE-J, survey of chronic obstructive pulmonary disease patients epidemiology in Japan.
Acknowledgments
The authors are grateful to the examinees who participated in this survey and the staff of the medical institutions who contributed to this survey. The following investigators took part in data collection of this survey: Dr. Takeshi Nawa (Hitachi General Hospital, Hitachi Ltd.), Dr. Kazuhiro Gotou (Health Park Clinic Kurosawa), Dr. Takashi Nakagawa (Omiya City Clinic), Dr. Koji Yamashita (Yotsukaido Tokushukai Hospital), Dr. Tatsuo Morikawa (Tokyo-Nishi Tokushukai Hospital), Dr. Takayuki Kashiwabara (JA Shizuoka Kohseiren Enshu Hospital), Dr. Tatsuya Shiraki (Matsubara Tokushukai Hospital), Dr. Ryo Kobayashi (Bell Clinic), Dr. Hiroshi Sonobe (Chugoku Central Hospital), Dr. Toshiki Fukui (Center for Preventive Medical Treatment, Olive Takamatsu Medical Clinic), Dr. Tokuji Motoki (Kochi Kenshin Clinic), Dr. Yasuhiro Ogata, Dr. Noritaka Higashi (Japanese Red Cross Kumamoto Health Care Center), Dr. Junko Aburaya (Koga Kenshin Center, Koga Ekimae Clinic), and Dr. Koki Ido (Osumi Kanoya Hospital).
Author Contributions
Conception or design: HO, TK, TS; data acquisition: NH, TN, TF; analysis or interpretation: all authors. Drafting the manuscript: HO, TK, TS; revising the manuscript critically for important intellectual content: all authors. All authors approved the final version for publication and agreed to be accountable for all aspects of the work.
Disclosure
GlaxoSmithKline (GSK) was the funding source and was involved in all stages of this study (WEUSKOP6290). GSK also funded all costs associated with the publishing of the present manuscript. HO, NH, TN, and TF received funding for this study from GSK. TK is an employee of GSK and owns stock of the company. TK received pay for a part-time lecture from Shiga University of Medical Science. TS is an employee of GSK. The authors report no other conflicts of interest in this work.
References
1. Ministry of Health, Labor and Welfare. A basic direction for comprehensive implementation of national health promotion. Available from: http://www.mhlw.go.jp/file/06-Seisakujouhou-10900000-Kenkoukyoku/0000047330.pdf.
2. GOLD Japan Committee. COPD recognition survey in 2018. Available from: http://www.gold-jac.jp/copd_facts_in_japan/copd_degree_of_recognition.html.
3. Hogg JC, Timens W. The pathology of chronic obstructive pulmonary disease. Annu Rev Pathol Mech Dis. 2009;4(1):435–459. doi:10.1146/annurev.pathol.4.110807.092145
4. The Japanese Respiratory Society. The JRS Guidelines for the Management of Chronic Obstructive Pulmonary Disease.
5. Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management and prevention of chronic obstructive pulmonary disease (2019report). Available from: https://goldcopd.org/wp-content/uploads/2018/11/GOLD-2019-v1.7-FINAL-14Nov2018-WMS.pdf.
6. American Thoracic Society. Statement on standards for the diagnosis and care of patients with Chronic Obstructive Pulmonary Disease (COPD) and asthma. Am Rev Respir Dis. 1987;136(1):225–244. doi:10.1164/ajrccm/136.1.225
7. Kanervisto M, Saarelainen S, Vasankari T, et al. COPD, chronic bronchitis and capacity for day-to-day activities: negative impact of illness on the health-related quality of life. Chron Respir Dis. 2010;7(4):207–215. doi:10.1177/1479972310368691
8. Martinez CH, Kim V, Chen Y, et al. The clinical impact of non-obstructive chronic bronchitis in current and former smokers. Respir Med. 2014;108(3):491–499. doi:10.1016/j.rmed.2013.11.003
9. Tan WC, Bourbeau J, Hernandez P, et al. Exacerbation-like respiratory symptoms in individuals without chronic obstructive pulmonary disease: results from a population-based study. Thorax. 2014;69(8):709–717. doi:10.1136/thoraxjnl-2013-205048
10. Regan EA, Lynch DA, Curran-Everett D, et al. Clinical and radiologic disease in smokers with normal spirometry. JAMA Intern Med. 2015;175(9):1539–1549. doi:10.1001/jamainternmed.2015.2735
11. Woodruff PG, Barr RG, Bleecker E, et al. Clinical significance of symptoms in smokers with preserved pulmonary function. N Engl J Med. 2016;374(19):1811–1821. doi:10.1056/NEJMoa1505971
12. Ferré A, Fuhrman C, Zureik M, et al. Chronic bronchitis in the general population: influence of age, gender and socio-economic conditions. Respir Med. 2012;106(3):467–471. doi:10.1016/j.rmed.2011.12.002
13. Omori H, Kaise T, Suzuki T, Hagan G. Prevalence of airflow limitation in subjects undergoing comprehensive health examination in Japan: survey of chronic obstructive pulmonary disease patients epidemiology in Japan. Int J Chron Obstruct Pulmon Dis. 2016;11:873–880. doi:10.2147/COPD.S99935
14. Jones PW, Harding G, Berry P, Wiklund I, Chen WH, Leidy NK. Development and first validation of the COPD Assessment Test. Eur Respir J. 2009;34(3):648–654. doi:10.1183/09031936.00102509
15. Stuart-Harris CH, Crofton J, Gilson JC, et al. Definition and classification of chronic bronchitis for clinical and epidemiological purposes. Lancet. 1965;285:775–779.
16. Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J. 2005;26(2):319–338. doi:10.1183/09031936.05.00034805
17. Sasaki H, Nakamura M, Kida K, et al. Reference value of spirogram and arterial blood gas partial pressure in Japanese. J Jpn Respir Soc. 2001;39:1–17.
18. Japan Society of Ningen Dock. Staging the severity. Available from: https://www.ningen-dock.jp/wp/common/data/other/release/hainteikubun_120405.pdf.
19. Wada T, Terashima S, Mimura A, et al. Effectiveness of encouragement to receive further consultation 3 months after Ningen Dock and future problems. Ningen Dock. 2012;27:748–754.
20. Martin MJ, Harrison TW. Causes of chronic productive cough: an approach to management. Respir Med. 2015;109(9):1105–1113. doi:10.1016/j.rmed.2015.05.020
21. Adachi M, Hozawa S, Nishikawa M, Yoshida A, Jinnai T, Tamura G. Asthma control and quality of life in a real-life setting: a cross-sectional study of adult asthma patients in Japan (ACQUIRE-2). J Asthma. 2019;56(9):1016–1025. doi:10.1080/02770903.2018.1514628
22. Chibana K, Ishii Y, Anraku Y, Fukuda T. Prevalence of airflow limitation in patients diagnosed and treated for symptoms of chronic bronchitis by general practitioners in Tochigi Prefecture, Japan. Intern Med. 2011;50(20):2277–2283. doi:10.2169/internalmedicine.50.5115
23. Allen-Ramey FC, Gupta S, DiBonaventura MD. Patient characteristics, treatment patterns, and health outcomes among COPD phenotypes. Int J Chron Obstruct Pulmon Dis. 2012;7:779–787. doi:10.2147/COPD.S35501
24. De Torres JP, Casanova C, Hernández C, Abreu J, Aguirre-Jaime A, Celli BR. Gender and COPD in patients attending a pulmonary clinic. Chest. 2005;128(4):2012–2016. doi:10.1378/chest.128.4.2012
25. Tatsumi K, Kasahara Y, Kurosu K, Tanabe N, Takiguchi Y, Kuriyama T. Clinical phenotypes of COPD: results of a Japanese epidemiological survey. Respirology. 2004;9(3):331–336. doi:10.1111/res.2004.9.issue-3
26. Braman SS. Chronic cough due to chronic bronchitis: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(1):104S–115S. doi:10.1378/chest.129.1_suppl.104S
27. Corhay JL, Vincken W, Schlesser M, Bossuyt P, Imschoot J. Chronic bronchitis in COPD patients is associated with increased risk of exacerbations: a cross-sectional multicentre study. Int J Clin Pract. 2013;67(12):1294–1301. doi:10.1111/ijcp.12248
28. Ramos FL, Krahnke JS, Kim V. Clinical issues of mucus accumulation in COPD. Int J Chron Obstruct Pulmon Dis. 2014;9:139–150. doi:10.2147/COPD.S38938
29. Lahousse L, Seys LJM, Joos GF, Franco OH, Stricker BH, Brusselle GG. Epidemiology and impact of chronic bronchitis in chronic obstructive pulmonary disease. Eur Respir J. 2017;50(2):1602470. doi:10.1183/13993003.02470-2016
30. Bowler RP, Kim V, Regan E, et al. Prediction of acute respiratory disease in current and former smokers with and without COPD. Chest. 2014;146(4):941–950. doi:10.1378/chest.13-2946
31. Dal Negro RW, Bonadiman L, Tognella S, Bricolo FP, Turco P. Extent and prevalence of cognitive dysfunction in chronic obstructive pulmonary disease, chronic non-obstructive bronchitis, and in asymptomatic smokers, compared to normal reference values. Int J Chron Obstruct Pulmon Dis. 2014;9:675–683. doi:10.2147/COPD.S63485
32. De Marco R, Accordini S, Cerveri I, et al. Incidence of chronic obstructive pulmonary disease in a cohort of young adults according to the presence of chronic cough and phlegm. Am J Respir Crit Care Med. 2007;175(1):32–39. doi:10.1164/rccm.200603-381OC
33. Martinez CH, Murray S, Barr RG, et al. Respiratory symptoms items from the COPD assessment test identify ever-smokers with preserved lung function at higher risk for poor respiratory outcomes: an analysis of the subpopulations and intermediate outcome measures in COPD study cohort. Ann Am Thorac Soc. 2017;14(5):636–642. doi:10.1513/AnnalsATS.201610-815OC
34. Yoo SH, Lee JH, Yoo KH, Jung KS, Rhee CK. Different pattern of chronic obstructive pulmonary disease assessment test score between chronic bronchitis and non-chronic bronchitis patients. Tuberc Respir Dis. 2018;81(3):228–232. doi:10.4046/trd.2017.0088
35. Hagimoto A, Nakamura N, Morita T, Masui S, Oshima A. Smoking cessation patterns and predictors of quitting smoking among the Japanese general population: a 1-year follow-up study. Addiction. 2010;105(1):164–173. doi:10.1111/add.2010.105.issue-1
36. Office for National Statistics. Smoking related behavior and attitudes, 2008/09. Available from: https://webarchive.nationalarchives.gov.uk/20151014031230/http://www.ons.gov.uk/ons/rel/lifestyles/smoking-related-behaviour-and-attitudes/2008-09/index.html.
37. Lavinghouze SR, Malarcher A, Jama A, Neff L, Debrot K, Whalen L. Trends in quit attempts among adult cigarette smokers — United States, 2001–2013. MMWR. 2015;64(40):1129–1135. doi:10.15585/mmwr.mm6440a1
38. World Health Organization. Tobacco taxes and prices: WHO report on the global tobacco epidemic 2017. Available from: http://www.who.int/tobacco/global_report/2017/appendix-ix/en/.
39. Igarashi A, Negishi S, Goto R, Suwa K. Web-based survey on smoking cessation behaviors of current and former smokers in Japan. Curr Med Res Opin. 2014;30(10):1911–1921. doi:10.1185/03007995.2014.938149
40. Hasegawa K, Sato S, Tanimura K, et al. Gastroesophageal reflux symptoms and nasal symptoms affect the severity of bronchitis symptoms in patients with chronic obstructive pulmonary disease. Respir Investig. 2018;56(3):230–237. doi:10.1016/j.resinv.2018.01.001
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.