Back to Journals » Pharmacogenomics and Personalized Medicine » Volume 13
CHRM3 rs2165870 Polymorphism Correlates with Postoperative Nausea and Vomiting Incidence and the Efficacy of Ondansetron in a Chinese Han Population
Authors Wang J, Li Y, Zheng C, Sun Y, Yang J
Received 18 March 2020
Accepted for publication 20 July 2020
Published 13 August 2020 Volume 2020:13 Pages 319—326
DOI https://doi.org/10.2147/PGPM.S254470
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Martin H Bluth
Jiayu Wang,1,2 Yang Li,3 Cuijuan Zheng,2 Yan Sun,1 Jianping Yang1
1Department of Anesthesiology, The First Affiliated Hospital of Soochow University, Suzhou 215006, Jiangsu, People’s Republic of China; 2Department of Anesthesiology, The Affiliated Huaian No.1 People’s Hospital of Nanjing Medical University, Huaian 223300, Jiangsu, People’s Republic of China; 3Jiangsu College of Nursing, Huaian 223300, Jiangsu, People’s Republic of China
Correspondence: Jianping Yang Email [email protected]
Background: Previous GWAS studies have shown that there is a relationship between M3 muscarinic acetylcholine receptor (CHRM3) rs2165870 polymorphism and postoperative nausea and vomiting (PONV) incidence. However, no Chinese studies have addressed this issue.
Methods: To explore the relationship between CHRM3 rs2165870 polymorphism and PONV incidence in a Chinese Han population, we enrolled 512 patients receiving elective surgery in this study. CHRM3 rs2165870 polymorphism was genotyped using PCR-RFLP method.
Results: We found that AA genotype or A allele of CHRM3 rs2165870 polymorphism elevated the risk of PONV (AA versus GG; OR, 2.88; 95% CI, 1.51– 5.47; P = 0.001; A versus G; OR, 1.39; 95% CI, 1.07– 1.81; P = 0.013). In addition, CHRM3 rs2165870 polymorphism was related to the risk of PONV among the males, smokers, and those individuals with Apfel Score 3– 4 or ASA classification 2– 3. Last, we assessed the effects of CHRM3 rs2165870 polymorphism on the treatment efficacy of ondansetron for PONV. Data uncovered that 103 of 209 patients (49.3%) showed response to ondansetron treatment for PONV. The PONV incidence was significantly higher in AA genotype carriers compared with GG genotype carriers during the first 2 h after surgery, but not from 2 to 24 h after surgery.
Conclusion: To sum up, this study reveals that CHRM3 rs2165870 polymorphism is related to the incidence of PONV and treatment effects of ondansetron for preventing PONV in this Chinese Han population.
Keywords: postoperative nausea and vomiting, CHRM3, single nucleotide polymorphism, ondansetron
Introduction
Postoperative nausea and vomiting (PONV) are reported to be the most common complication after anesthesia.1 The incidence of PONV is about 30% of overall surgical patients.2 Unresolved PONV will lead to electrolyte imbalance, dehydration, pulmonary aspiration, wound dehiscence, and delayed hospital discharge.3,4 It may result in elongated recovery time, increased nursing care, and health care costs. Female gender, PONV or motion sickness history, non-smoking status, and postoperative opioids use are the well-established risk factors for PONV.5 However, individuals without exposure to these abovementioned factors may have PONV, indicating that other factors, including genetic factors, may contribute to PONV.6 Thus, identifying genetic markers for PONV is urgently needed.
Recently, a lot of studies have focused on the relationship between different gene polymorphisms and PONV occurrence. A recently reported systematic review and some original studies indicate that polymorphisms in genes including hepatic cytochrome P450 (CYP2D6), Opioid receptor mu 1 (OPRM1), M3 muscarinic acetylcholine receptor (CHRM3), 5-hydroxytryptamine type 3 (5-HT), DRD2, TACR1, FAAH, HTR3B, and ABCB1 were associated with PONV risk.6–19 Ondansetron is a 5-HT receptor antagonist, which is usually administered to prevent PONV. Ondansetron is mainly metabolized by CYP2D6 enzyme.7 Most of opioids exerted effects on the opioid mu-1 receptor, which is encoded by the OPRM1 gene.7 OPRM1 A118G polymorphism was a primary variant for the study of pharmacogenetics of opioid response. Kong et al performed a meta-analysis to explore the relationship between OPRM1 gene A118G polymorphism and PONV, and found that this SNP reduced the risk of postoperative vomiting, but not pruritus, nausea, and dizziness.8 However, functional alleles of CYP2D6 gene were associated with a higher occurrence of PONV.6 Rs2165870 polymorphism is located on promoter region of CHRM3. Recently, three studies investigated the association between CHRM3 rs2165870 polymorphism and PONV risk, but with conflicting findings.10,11,20 A genome-wide association study (GWAS) explored the association between some loci of genes and PONV risk.20 They only observed GG+AA genotype of CHRM3 rs2165870 polymorphism was linked with PONV risk even after correcting for multiple testing.20 Subsequent two studies suggested that AA or GA genotype of CHRM3 rs2165870 polymorphism contributed to increased risk for PONV.10,11 To date, no studies from China have investigated the relationship between CHRM3 rs2165870 polymorphism and PONV risk. Thus, we performed this study to evaluate the effects of CHRM3 rs2165870 polymorphism on PONV occurrence among patients receiving elective surgery. In addition, we appraised the effects of CHRM3 rs2165870 polymorphism on the treatment efficacy of ondansetron for preventing PONV.
Methods
Patients and Ethics Statement
This study protocol was approved by the institutional review board of Huaian No.1 People’s Hospital. This study was conducted in accordance with the Declaration of Helsinki. We used the Quanto (http://hydra.usc.edu/gxe) to determine the sample size before this study with the following conditions: α = 0.05, β = 0.1, allele frequency = 0.3, power value = 0.9, and the estimated OR = 2.0; the sample sizes of case and control groups were 178 and 178, respectively. Eventually, a total of 512 patients (209 cases and 303 controls) receiving elective surgery (neurosurgery, throat and gynecological, or general surgery) with general anesthesia from the Huaian No.1 People’s Hospital (ASA-physical status of 1 or 2 or 3) were recruited in this study. All participants provided written informed consent. PONV cases were patients who had nausea and vomiting from 0 to 24 h after elective surgery. Controls were patients without nausea and vomiting after elective surgery. Patients with neurological and psychiatric disorders, or a history of drug abuse were excluded. Control subjects receiving elective surgery did not have PONV. Clinical features and demographic data of these patients were collected before surgery.
Fentanyl, vecuronium bromide, midazolam, and etomidate were combined to induce the general anesthesia. All patients received a combination of inhalation and intravenous medication for maintenance of anesthesia (intravenous: propofol, 4mg/kg/hour; and inhalation: sevoflurane, 1–2 mac). The dosage of fentanyl and operation time was recorded for all patients. 0.1mg/h fentanyl was injected intravenously at 30 minutes before the end of the surgery.
In stage one, we investigated whether CHRM3 rs2165870 polymorphism was associated the risk of PONV in a population of 512 patients. Of the 512 patients assessed to participate in this study, 209 were classified as PONV patients, 303 were classified as controls which have not incidence of PONV after elective surgery. In stage two, we explored whether the CHRM3 rs2165870 polymorphism affect the efficacy of ondansetron (0.1 mg.kg−1) to prevent PONV. Ondansetron (0.1 mg/kg) was intravenously administered at 30 minutes before the end of surgery. We noted any PONV from 0 h to 24 h after surgery. Any incidence of nausea that was recorded either in the 0–2 h or 2–24 h after the operation was presented as 'yes with' or 'no without' PONV as the responder outcome. If a patient experienced no episodes of nausea or vomiting after the administration of ondansetron, he or she was regarded as the responder to ondansetron. If a patient still experienced nausea or vomiting after the administration of ondansetron, he or she was the no-responders to ondansetron.
DNA Extraction and Genotyping
By utilizing the Puregenee DNA purification kit (Gentra, Minneapolis, MN, USA), Genomic DNA extracted from 2mL of peripheral blood was obtained. The corresponding concentration and purity of the extracted DNA were measured by absorbance and running electrophoresis, respectively. The gene distribution of CHRM3 rs2165870 polymorphism was evaluated by PCR-restriction fragment length polymorphism. The primers of the polymorphism in nucleotide extension reaction were 5ʹ-TGCATCTGTTTACAGCCTTA-3ʹ (forward) and 5ʹ- TGCATCTGTTTACAGCCTTG-3ʹ (reverse). Polymerase chain reaction (PCR) was carried out as follows: 5 min at 94 °C; 30 s at 94 °C, 35 cycles; extending for 10 min at 72 °C. The PCR products were first horizontally electrophorized on an ethidium bromide-dyed agarose gel (2% w/v) and then photographed. Ten percent of the samples were re-genotyped to ensure the genotyping accuracy, and the coincidence rate is 100%.
Statistical methods
All statistical analyses were addressed by SPSS 22.0 (SPSS Inc., Chicago, USA). All variables were calculated by Chi-square (χ2) tests or Student’s t-tests. HWE test among control group was assessed using a χ2 test. To estimate the statistical power of our study design, we implemented a comprehensive power analysis using Genetic Power Calculator 33. The crude or adjusted odds ratios (ORs) and 95% confidence intervals (CIs) were evaluated by use of logistic regression analysis. Stratified analyses by gender, age, alcohol, smoking, history of PONV, history of motion sickness, Apfel Score, and ASA classification were conducted. If a P value < 0.05, it was considered statistically significant.
Results
Study Population
Table 1 contains the demographic data and clinical features of the patients. No significant differences were observed about all characteristics of these patients among different genotype carriers, except for the history of PONV. GG genotype carriers showed higher incidence of history of PONV compared with other genotypes. Other characteristics of these patients are summarized in Table 1. In addition, data indicated that 209 of 512 patients (40.8%) had PONV (Supplemental Table 1). The percentage of PONV patients with each genotype were 39.2% (GG), 45.9% (GA), 14.9% (AA), respectively (see Table 2).
 |
Table 1 Demographics and Risk Factors for Postoperative Nausea and Vomiting Stratified for CHRM3 Rs2165870 Genotypes |
 |
Table 2 Postoperative Nausea and Vomiting (PONV) (2–6h) Occurrence to CHRM3 Rs2165870 Genotype of Study Patients |
PONV Risk and CHRM3 Rs2165870 Polymorphism
The distribution of alleles and genotypes of the CHRM3 rs2165870 polymorphism are shown in Table 2 (PHWE = 0.107). Obviously, 209 of 512 patients (40.8%) were classified as cases, 303 of 512 patients (59.2%) were classified as controls. Data showed that AA genotype was related to an elevated risk of PONV risk (AA versus GG; OR, 2.88; 95% CI, 1.51–5.47; P = 0.001). Even after adjusting the gender and age, this association was still significant (P < 0.05). In addition, A allele of CHRM3 rs2165870 polymorphism increased the risk of PONV in the allelic model (A versus G; OR, 1.39; 95% CI, 1.07–1.81; P = 0.013).
Next, we investigated the association of demographic and clinical characteristics with genotypes of rs2165870 polymorphism (Table 3). Data revealed that CHRM3 rs2165870 polymorphism correlated with the risk of PONV among the males, smokers, and those individuals with Apfel Score 3–4 or ASA classification 2–3. In addition, we explored the effects of the types of surgeries on PONV; overall, the types of surgeries had no significant effects on PONV (Supplemental Table 2).
 |
Table 3 Stratified Analyses Between CHRM3 Rs2165870 Polymorphism and the Risk of PONV |
Association of CHRM3 Rs2165870 Polymorphism with the Treatment Efficacy of Ondansetron for PONV
Last, we evaluated the association of CHRM3 rs2165870 polymorphism with the efficacy of ondansetron for PONV (Table 4). The incidence of PONV was recorded among different genotypes in CHRM3 rs2165870 polymorphism. One hundred three of 209 patients (49.3%) showed a response to ondansetron treatment. The PONV incidence was higher in AA genotype carriers compared with GG genotype carriers during the first 2 h after surgery. We did not obtain significant differences regarding the incidence of PONV for different genotypes of rs2165870 polymorphism from 2 to 24 h after surgery.
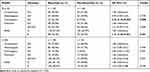 |
Table 4 Effects of CHRM3 Rs2165870 on the Efficacy of Ondansetron for Postoperative Nausea and Vomiting |
Discussion
The incidence of PONV depended on anesthetic, surgical, risk factors for patients, and genetic factors. The pharmacogenomics of PONV are poorly understood. Actually, studies on the effects of genetic factors were limited up to date. In addition, the sample size of enrolled patients in these studies was not large, which resulted in low statistical power. Among investigated genes, ABCB1,19,21 CYP2D6,22–24 and OPRM1 gene were most explored genes before.25–27
As for CHRM3 gene, only three studies addressed the relationship between CHRM3 rs2165870 polymorphism and PONV risk. Up to now, Janicki et al conducted the GWAS study, whose aims were to obtain genetic risk loci related with PONV risk.20 They revealed the GG+AA genotype of CHRM3 rs2165870 polymorphism was the only locus observed in a GWAS related with PONV risk in two independent studies.20 It is of note that this GWAS only enrolled 122 surgery patients with severe PONV and 129 matched controls, which may yield false positive results. Due to the GWAS findings, Klenke et al conducted a prospective, controlled study with 454 individuals undergoing elective surgery to validate previous findings.11 In addition, they found CHRM3 rs2165870 polymorphism could predict PONV susceptibility.11 They revealed that AA or GA genotype carriers showed increased risk for PONV compared with GG genotypes. Subsequently, Klenke et al also retrospectively performed a study with 472 patients receiving elective surgery, and showed CHRM3 rs2165870, and KCNB2 rs349358 polymorphism increased the risk of PONV,28 and they also found that AA or GA genotype of CHRM3 rs2165870 polymorphism contributed to PONV risk. In this study, we observed that AA genotype or A allele of CHRM3 rs2165870 polymorphism increased the risk of PONV in Chinese Han population. However, we did not observe an association between GA or GG+AA genotypes and PONV risk, which was inconsistent with abovementioned studies. Potential factors may be account for these conflicting findings of these studies: 1) genetic heterogeneity in different disorders was differential; 2) clinical heterogeneity of these disorders was diverse; 3) the sample sizes were significantly different. Limited sample sizes in GWAS and the study by Klenke et al may produce the over-estimation of effect size; and 4) differences in inclusion criteria of patients should be considered. Subgroup analysis obtained that CHRM3 rs2165870 polymorphism was related to increased risk of PONV in the groups of males, smokers, patients with higher Apfel Score and ASA classification.
Although some risk factors, surgical treatment, and perioperative drugs determine the patient’s risk for PONV, identifying the patient’s genetic genotypes was useful for selecting appropriate medications to prevent PONV during the perioperation. In this study, we found that AA genotype or A allele carriers showed high incidence of PONV in patients with elective surgery, which promoted clinicians to use some medications for these patients to restrain the occurrence of PONV. Therefore, we utilized ondansetron to prevent PONV. Our data observed that AA genotype or A allele carriers showed response to ondansetron treatment during the first 2 h after surgery. However, the incidence of PONV between different genotype carriers showed no significant differences regarding the treatment of ondansetron from 2 to 24 h after surgery. Thus, CHRM3 rs2165870 polymorphism may be an important marker for predicting the responsiveness for ondansetron treatment for PONV patients.
As for clinical practice, we found that AA genotype or A allele of CHRM3 rs2165870 polymorphism elevated the risk of PONV risk in this study, suggesting that surgery patients carrying AA genotype or A allele should be taken care of PONV issue for clinicians. Thus, gene detection for surgery patients before anesthesia may be necessary in the future. In addition, the PONV incidence was significantly higher in AA genotype carriers compared with GG genotype carriers during the first 2 h after surgery, but not from 2 to 24 h after surgery, indicating that AA genotype carriers in PONV was associated with lower response to ondansetron. Maybe clinicians should use other drugs to restrain the occurrence of PONV patients carrying AA genotype.
This study had several limitations. First, the sample size was not large enough in this study, which may yield false positive results. Further studies with larger sample size are urgently needed. Second, this study only investigated CHRM3 rs2165870 polymorphism whether other genetic variants of CHRM3 gene contributed to the genetic PONV risk. Whether CHRM3 rs2165870 polymorphism was in linkage disequilibrium with other SNPs should be also explored. Third, because a hospital-based case–control design, selection bias was unavoidable. Fourth, the potential mechanisms of CHRM3 rs2165870 polymorphism affecting the incidence of PONV should be investigated. Further cell and animal experiments should be performed to explore the underlying mechanisms. Fifth, Ondansetron is mainly metabolized by CYP2D6 enzyme; however, we did not assess the impact of CYP2D6 gene variations on ondansetron treatment for PONV patients in the Chinese population. Finally, further studies in other populations are needed to verify our findings.
In conclusion, this study indicates that CHRM3 rs2165870 polymorphism correlates with the incidence of PONV and the treatment effects of ondansetron for preventing the occurrence of PONV in this Chinese Han population.
Data Sharing Statement
The data are available on reasonable request to the correspondence author.
Disclosure
The authors report no funding and no conflicts of interest for this work.
References
1. Gan TJ. Postoperative nausea and vomiting–can it be eliminated? JAMA. 2002;287(10):1233–1236. doi:10.1001/jama.287.10.1233
2. Kovac AL. Updates in the management of postoperative nausea and vomiting. Adv Anesth. 2018;36(1):81–97. doi:10.1016/j.aan.2018.07.004
3. Glass PS, White PF. Practice guidelines for the management of postoperative nausea and vomiting: past, present, and future. Anesth Analg. 2007;105(6):1528–1529. doi:10.1213/01.ane.0000295854.53423.8A
4. Kovac AL. Update on the management of postoperative nausea and vomiting. Drugs. 2013;73(14):1525–1547. doi:10.1007/s40265-013-0110-7
5. Apfel CC, Laara E, Koivuranta M, Greim CA, Roewer N. A simplified risk score for predicting postoperative nausea and vomiting: conclusions from cross-validations between two centers. Anesthesiology. 1999;91(3):693–700. doi:10.1097/00000542-199909000-00022
6. Lopez-Morales P, Flores-Funes D, Sanchez-Migallon EG, Liron-Ruiz RJ, Aguayo-Albasini JL. Genetic factors associated with postoperative nausea and vomiting: a systematic review. J Gastrointest Surg. 2018;22(9):1645–1651. doi:10.1007/s11605-018-3788-8
7. Aroke EN, Hicks TL. Pharmacogenetics of postoperative nausea and vomiting. J Perianesth Nurs. 2019;34(6):1088–1105. doi:10.1016/j.jopan.2019.03.007
8. Kong Y, Yan T, Gong S, Deng H, Zhang G, Wang J. Opioid receptor mu 1 (OPRM1) A118G polymorphism (rs1799971) and postoperative nausea and vomiting. Am J Transl Res. 2018;10(9):2764–2780.
9. Niewinski PA, Wojciechowski R, Sliwinski M, et al. CYP2D6 basic genotyping as a potential tool to improve the antiemetic efficacy of ondansetron in prophylaxis of postoperative nausea and vomiting. Adv Clin Exp Med. 2018;27(11):1499–1503. doi:10.17219/acem/69451
10. Klenke S, de Vries GJ, Schiefer L, et al. Genetic contribution to PONV risk. Anaesth Crit Care Pain Med. 2020;39(1):45–51. doi:10.1016/j.accpm.2019.04.012
11. Klenke S, de Vries GJ, Schiefer L, et al. CHRM3 rs2165870 polymorphism is independently associated with postoperative nausea and vomiting, but combined prophylaxis is effective. Br J Anaesth. 2018;121(1):58–65. doi:10.1016/j.bja.2018.02.025
12. Wen QH, Zhang Z, Cai WK, Lin XQ, He GH. The associations between CYP2D6*10 C188T polymorphism and pharmacokinetics and clinical outcomes of tramadol: a systematic review and meta-analysis. Pain Med. 2020. doi:10.1093/pm/pnaa140
13. Zhang X, Liang Y, Zhang N, et al. The relevance of the OPRM1 118A>G genetic variant for opioid requirement in pain treatment: a meta-analysis. Pain Physician. 2019;22(4):331–340.
14. Kim MS, Lee JR, Choi EM, Kim EH, Choi SH. Association of 5-HT3B receptor gene polymorphisms with the efficacy of ondansetron for postoperative nausea and vomiting. Yonsei Med J. 2015;56(5):1415–1420. doi:10.3349/ymj.2015.56.5.1415
15. Frey UH, Schnee C, Achilles M, Silvanus MT, Esser J, Peters J. Postoperative nausea and vomiting: the role of the dopamine D2 receptor TaqIA polymorphism. Eur J Anaesthesiol. 2016;33(2):84–89. doi:10.1097/EJA.0000000000000320
16. Hayase T, Sugino S, Moriya H, Yamakage M. TACR1 gene polymorphism and sex differences in postoperative nausea and vomiting. Anaesthesia. 2015;70(10):1148–1159. doi:10.1111/anae.13082
17. Sadhasivam S, Zhang X, Chidambaran V, et al. Novel associations between FAAH genetic variants and postoperative central opioid-related adverse effects. Pharmacogenomics J. 2015;15(5):436–442. doi:10.1038/tpj.2014.79
18. Ma XX, Chen QX, Wu SJ, Hu Y, Fang XM. Polymorphisms of the HTR3B gene are associated with post-surgery emesis in a Chinese Han population. J Clin Pharm Ther. 2013;38(2):150–155. doi:10.1111/jcpt.12033
19. Choi EM, Lee MG, Lee SH, Choi KW, Choi SH. Association of ABCB1 polymorphisms with the efficacy of ondansetron for postoperative nausea and vomiting. Anaesthesia. 2010;65(10):996–1000. doi:10.1111/j.1365-2044.2010.06476.x
20. Janicki PK, Vealey R, Liu J, Escajeda J, Postula M, Welker K. Genome-wide Association study using pooled DNA to identify candidate markers mediating susceptibility to postoperative nausea and vomiting. Anesthesiology. 2011;115(1):54–64. doi:10.1097/ALN.0b013e31821810c7
21. Farhat K, Iqbal J, Waheed A, Mansoor Q, Ismail M, Pasha AK. Association of anti-emetic efficacy of ondansetron with G2677T polymorphism in a drug transporter gene ABCB1 in Pakistani population. J Coll Physicians Surg Pak. 2015;25(7):486–490. doi:07.2015/JCPSP.486490
22. Candiotti KA, Birnbach DJ, Lubarsky DA, et al. The impact of pharmacogenomics on postoperative nausea and vomiting: do CYP2D6 allele copy number and polymorphisms affect the success or failure of ondansetron prophylaxis? Anesthesiology. 2005;102(3):543–549. doi:10.1097/00000542-200503000-00011
23. Janicki PK, Schuler HG, Jarzembowski TM, Rossi M
24. Wesmiller SW, Henker RA, Sereika SM, et al. The association of CYP2D6 genotype and postoperative nausea and vomiting in orthopedic trauma patients. Biol Res Nurs. 2013;15(4):382–389. doi:10.1177/1099800412449181
25. Ren ZY, Xu XQ, Bao YP, et al. The impact of genetic variation on sensitivity to opioid analgesics in patients with postoperative pain: a systematic review and meta-analysis. Pain Physician. 2015;18(2):131–152.
26. Sugino S, Hayase T, Higuchi M, et al. Association of mu-opioid receptor gene (OPRM1) haplotypes with postoperative nausea and vomiting. Exp Brain Res. 2014;232(8):2627–2635. doi:10.1007/s00221-014-3987-9
27. Lee SH, Kim JD, Park SA, Oh CS, Kim SH. Effects of micro-opioid receptor gene polymorphism on postoperative nausea and vomiting in patients undergoing general anesthesia with remifentanil: double blinded randomized trial. J Korean Med Sci. 2015;30(5):651–657. doi:10.3346/jkms.2015.30.5.651
28. Klenke S, de Vries GJ, Schiefer L, et al. Genetic contribution to PONV risk. Anaesth Crit Care Pain Med. 2019. doi:10.1016/j.accpm.2019.04.012
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
