Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 11 » Issue 1
Childhood maltreatment as a risk factor for COPD: findings from a population-based survey of Canadian adults
Authors Shields ME, Hovdestad WE, Gilbert CP, Tonmyr LE
Received 1 March 2016
Accepted for publication 8 May 2016
Published 26 October 2016 Volume 2016:11(1) Pages 2641—2650
DOI https://doi.org/10.2147/COPD.S107549
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Richard Russell
Margot E Shields, Wendy E Hovdestad, Charles P Gilbert, Lil E Tonmyr
Public Health Agency of Canada, Ottawa, ON, Canada
Objective: The aim of this study was to examine the associations between childhood maltreatment (CM) and COPD in adulthood.
Methods: Data were from 15,902 respondents to the 2012 Canadian Community Health Survey – Mental Health. Multiple logistic regression models were used to examine associations between CM and COPD and the role of smoking and mental and substance use variables as mediators in associations.
Results: COPD in adulthood was related to CM, with associations differing by sex. Among females, COPD was related to childhood physical abuse (CPA), childhood sexual abuse, and childhood exposure to intimate partner violence, but in the fully adjusted models, the association with CPA did not persist. Among males, COPD was related to childhood exposure to intimate partner violence and severe and frequent CPA, but these associations did not persist in the fully adjusted models.
Conclusion: Results from this study establish CM as a risk factor for COPD in adulthood. A large part of the association is attributable to cigarette smoking, particularly for males. These findings underscore the importance of interventions to prevent CM as well as programs to assist victims of CM in dealing with tobacco addiction.
Keywords: child abuse, cigarette, smoking, physical abuse, sexual abuse, intimate partner violence, domestic violence, family violence
Introduction
COPD refers to a group of debilitating and degenerative diseases of the lungs including emphysema and chronic bronchitis.1,2 In Canada, COPD is a leading cause of hospital admissions among major chronic illnesses and has a high readmission rate, placing a significant strain on the health care system.3
Although cigarette smoking is the underlying cause of COPD in 80%–90% of cases, environmental factors such as occupational exposure to dusts and fumes, exposure to secondhand smoke, and air pollution may play a role in the development and prognosis of COPD.1,2,4 In addition, there is a growing body of evidence that disease suffered in adulthood may originate from adversities experienced in childhood, supporting a life course framework to better understand the determinants of chronic disease.5–7 Childhood adversities (including childhood maltreatment [CM]) are related to various physical chronic conditions in adulthood.8–12 Although associations between CM and COPD have rarely been studied, recent research provides evidence of a possible link.7,13,14
The life course approach posits that there are multiple pathways underlying the associations between CM and disease in adulthood.5–7 Since CM has been shown to predict smoking – the primary underlying cause of COPD – the association between CM and COPD may be mediated through smoking.15,16 A mediating relationship17 occurs if a third variable (smoking) plays a pivotal role in explaining the association between two other variables (CM and COPD). Furthermore, CM is associated with early smoking initiation, heavy smoking, and persistent smoking,15,16,18 factors that further elevate the risk and prognosis of COPD.19,20 In addition, CM is associated with increased risk of mental and substance use disorders21 and individuals with these disorders have higher smoking rates and are less successful at quitting.22,23 Therefore, associations between CM and COPD may be further mediated via mental and substance use disorders. However, other pathways beyond smoking may be involved since associations between CM and COPD have been observed among individuals who never smoked.14
Using data from a large sample of the Canadian adult population, this study examines the associations between three types of CM (childhood physical abuse [CPA], childhood sexual abuse [CSA], and childhood exposure to intimate partner violence [CEIPV]) and COPD. The role of smoking and mental and substance use disorders as mediators in associations between CM and COPD is investigated. Because sex differences have been observed in associations between CM and health conditions, we test for interactions between sex and CM in relation to COPD.24–27 We also examine the association between CM and COPD among individuals who never smoked.
Methods
Data and sample
The 2012 Canadian Community Health Survey – Mental Health (CCHS-MH) was conducted by Statistics Canada using a multistage stratified clustered sampling design.28 The target population for the 2012 CCHS-MH was household residents aged 15 years or older living in the ten Canadian provinces. Excluded from the survey’s coverage were: persons living on reserves and other Aboriginal settlements, full-time members of the Canadian Forces, and the institutionalized population. Overall, these exclusions represent ~3% of the target population. The response rate was 68.9%, yielding a sample of 25,113 individuals aged 15 years or older.28
CCHS-MH respondents were asked for permission to share the information they provided with Statistic Canada’s partners, which included the Public Health Agency of Canada. Most respondents (n=23,709; 94%) agreed to share. This article is based on data from only those respondents who agreed that their data could be shared (their consent was implicitly taken by responding “yes” to the following question “Do you agree to share the information provided?”). Because the study was based on an existing datafile, the joint Health Canada and Public Health Agency of Canada Research Ethics Board has decided that the requirement to obtain ethical approval was not necessary due to the nature of the study.
The question on COPD was asked only to respondents aged 35 years or older (n=16,508). This study is based on a total sample of 15,902; respondents were excluded due to missing values for CM (n=360), COPD (n=9), or any of the sociodemographic or smoking variables (n=237).
Measures
CM variables
CPA, CSA, and CEIPV were assessed by asking respondents about “things that may have happened to you before you were 16 in your school, in your neighborhood, or in your family” using the items shown in Figure 1.
  | Figure 1 CM items and definitions. |
The items for CPA and CEIPV are from the Childhood Experiences of Violence Questionnaire (CEVQ).29 The CSA items are very similar to ones used in the 2009 Canadian General Social Survey.30 For each type of abuse, binary variables (yes/no) were created following CEVQ guidelines. Variables were also derived to indicate the severity and frequency of abuse as indicated in Figure 1.
COPD
In the CCHS-MH, the presence of chronic conditions, including COPD, was based on self-reported diagnosed illness. Respondents were asked about any “long-term health conditions that have lasted or are expected to last six months or more and that have been diagnosed by a health professional”. A checklist of conditions was included, one of which was “chronic bronchitis, emphysema, or COPD”.
Smoking variables
Smoking status was based on responses to the following questions:
- At the present time, do you smoke cigarettes daily, occasionally or not at all?
- Have you ever smoked cigarettes daily?
“Current daily smokers” were those who answered “daily” to question 1, “former daily smokers” were those who answered “occasionally” or “not at all” to question 1 and “yes” to question 2. “Never daily smokers” were those who responded “occasionally” or “not at all” to question 1 and “no” to question 2.
Former daily smokers were asked “At what age did you stop smoking cigarettes daily”? This was used in conjunction with age at the time of the interview to calculate the number of years since quitting daily smoking. Using this information, former daily smokers were further categorized as: those who had quit within the past 4 years, 5-19 years, or ≥20 years.
Current and former daily smokers were asked about the number of cigarettes usually smoked per day. This was used as a measure of smoking intensity. Based on this information, respondents were classified into three intensity groups (<15, 15-24, or ≥25 cigarettes per day).
Respondents were classified into one of 13 categories based on smoking status; current daily smokers into three categories based on intensity, former daily smokers into nine categories based on smoking intensity and years since quitting, and those who never smoked daily.
Mental and substance use disorders
Lifetime history of mental and substance use disorders was assessed using the World Health Organization’s version of the Composite International Diagnostic Interview and based on the criteria of the Diagnostic and Statistical Manual of Mental Disorders, fourth edition.31 The specific disorders included depression, bipolar disorder, generalized anxiety disorder, and alcohol and drug abuse/dependence.
Sociodemographic characteristics
The sociodemographic characteristics used as covariates in the logistic regression models included age (continuous), marital status (married, widowed, divorced/separated, single, never married), highest level of education attained by the respondent (less than secondary graduation, secondary graduation, some postsecondary, postsecondary graduation), household income (quintiles based on household income adjusted by Statistics Canada’s low-income cutoffs specific to the number of individuals in the household, the size of the community, and the survey year), immigrant status (<20 years in Canada, 20 years or more in Canada, Canadian born), ethnicity (White, Black, Southeast/East Asian, off-reserve Aboriginal, other), employment status the week before the interview (employed, unemployed, not in the labor force), and place of residence (urban/rural).
Analysis
Logistic regression analysis was used to examine associations between the CM variables and COPD, controlling for age (model 1). Regressions used the binary variables for CPA, CSA, and CEIPV as well as the severity and frequency CM variables. The role of potential confounders (sociodemographic characteristics) and mediators (smoking status and mental and substance use disorders) in associations between CM and COPD was assessed by running four additional models (models 2–5).
In the second model, sociodemographic characteristics were added; in the third model, smoking variables; in the fourth model, both sociodemographic characteristics and smoking variables; and in the final model, (model 5) mental and substance use disorders in addition to sociodemographic characteristics and smoking variables.
To demonstrate mediation,17 we compared regression coefficients for the association between CM and COPD before and after each mediator was added to the model. Since raw regression coefficients are not directly comparable across logistic regression models,32 the logistic regression coefficients were first standardized based on a formula proposed by Menard.33
For each CM variable, the percentage change in the standardized regression coefficient is presented (ie, the percentage change resulting from the inclusion of each mediator/confounding variable). Attenuation in associations provides evidence of mediation.17,32,33 Using standardized regression coefficients is beneficial when making comparisons of the effects of predictors across models since all predictors are converted to a common scale of measurement.33 However, when demonstrating substantive findings for categorical variables, it is more relevant to present results based on unstandardized variables,33 and therefore odds ratios (ORs) are all based on unstandardized regression coefficients.
Analyses were conducted using SAS Enterprise Guide 5.1. All estimates are based on weighted data. Weights were created at Statistics Canada so that the data would be representative of the Canadian population living in the ten provinces in 2012 and were adjusted to compensate for nonresponse. Variance estimates and 95% confidence intervals (CIs) were calculated using the bootstrap technique (with the SAS “proc survey” procedures) to account for the complex survey design of the CCHS-MH.28
Results
First, we tested for sex differences in associations between reporting CM and COPD. Based on the binary CM variables, significant sex interactions were observed for CPA (OR =1.6, 95% CI: 1.0, 2.5) and CSA (OR =2.0, 95% CI: 1.1, 3.4) with associations being stronger for females (data not shown). The interaction with CEIPV was elevated (OR =1.5, 95% CI: 0.8, 2.8), suggesting a stronger association for females, but it did not attain statistical significance. In light of these findings, we stratified the analyses by sex.
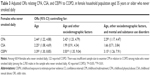
COPD was reported by 4.1% of females and 3.4% of males (Table 1). For both sexes, the most commonly reported form of CM was CPA (21.9% of females and 34.1% of males). CSA was reported by 16.1% of females and 7.1% of males, and CEIPV by 9.6% of females and 7.2% of males.
Based on reports of severe and frequent CM, the prevalence for CPA was 2.8% for females and 3.0% for males, and for CSA 4.0% for females and 1.7% for males. Frequent CEIPV was reported by 5.5% of females and 3.7% of males.
Associations between CM and COPD among females (controlling for age)
Among females (Table 2), the binary CPA variable was significantly associated with COPD when controlling for age (OR =1.8). A dose–response relationship emerged between CPA and COPD when severity and frequency were considered (OR =3.5 for severe and frequent CPA and OR =2.4 for severe CPA, ≤10 times). A similar pattern was observed for CSA; the odds for reporting COPD were 2.4 times higher among females reporting CSA based on the binary variable and 4.0 times higher when severe and frequent CSA was reported. Females who reported CEIPV had more than three times the odds of reporting COPD, but there was no dose–response relationship: ORs were ~3 whether the reported frequency was three to ten times or more than ten times.
Associations between CM and COPD among males (controlling for age)
Among males (Table 2), the binary CPA variable was not significantly associated with COPD. However, males who reported severe and frequent CPA had 2.6 times the odds of reporting COPD than males who reported no CPA. CSA was not significantly related to reporting COPD among males even when severity and frequency were taken into account. Males who reported CEIPV had 2.1 times the odds of reporting COPD with the odds being slightly higher (2.5) when frequent CEIPV was reported.
Effects of confounding and mediating variables
When sociodemographic characteristics, smoking status, and mental and substance use disorders were included in the models, among females, CSA (based on the binary variable), severe and frequent CSA, and CEIPV continued to be significantly associated with COPD. Among males, no associations retained statistical significance.
The inclusion of smoking status was influential in attenuating associations, particularly for males. The inclusion of control variables accounting for smoking intensity and years since quitting attenuated associations more than what was observed when more simplistic controls (current smoker/former smoker) were used (data not shown). However, the additions of sociodemographic characteristics and mental and substance use disorders resulted in further reductions in associations.
Associations between CM and COPD among those who never smoked
There was insufficient sample size to examine CM in relation to COPD among males who never smoked daily (among the 2,783 males in the sample who never smoked daily only 42 reported COPD). Among females, there was insufficient sample to consider associations using the CM variables that accounted for severity and frequency.
Based on the binary CM variables (Table 3), among females who never smoked daily all three types of maltreatment were associated with COPD (OR =2.4 for CPA, OR =2.2 for CSA, OR =3.4 for CEIPV). In the fully adjusted model, the association for CSA no longer attained statistical significance.
Discussion
We found that COPD in adulthood was related to CM with associations differing by sex. Based on binary CM variables, among females, COPD was related to CPA, CSA, and CEIPV. In the fully adjusted models controlling for smoking status and other covariates, the associations with CSA and CEIPV persisted but not with CPA. Among males, COPD was related to CEIPV, but this association did not persist in the fully adjusted model.
When severity and frequency of CM were taken into account, dose–response relationships between CPA, CSA, and COPD were observed among females with the strongest associations being observed for those who reported severe and frequent CPA or severe and frequent CSA. In the fully adjusted models, only the association with severe and frequent CSA persisted. Among males, a significant association was observed between severe and frequent CPA and COPD. However, this association did not persist in the fully adjusted model.
Our findings are for the most part consistent with three other studies that examined associations between CM and COPD based on samples from the American population.7,13,14 Using data from 3,000 respondents to the Wisconsin Longitudinal Study, Springer7 found a significant association between CPA and bronchitis/emphysema in adulthood; however, the association did not remain when controlling for mental health and smoking status. Similarly, Anda et al13 found a graded relationship between a cumulative measure of eight childhood adversities (including four measures of CM) and having been diagnosed with COPD in adulthood using a large sample of members of the Kaiser Foundation Health Plan in San Diego, California.
Many of our findings are similar to those of Cunningham et al14 who examined associations between several childhood adversities, including CPA, CSA, and CEIPV, and COPD using a large sample (n=46,000) of the general population in five American states. Consistent with our results, in the fully adjusted models controlling for sociodemographic variables and smoking status, they found that among females there was a higher likelihood of COPD in adulthood for those who reported CSA and CEIPV, and similar to our findings the association between CPA and COPD did not attain statistical significance. Likewise, they found that in the fully adjusted models all three types of CM were not significantly associated with COPD among males.
Similar to Cunningham et al, we examined associations between CM and COPD among the population who never smoked. In the unadjusted models, both studies found that among females who never smoked, CPA, CSA, and CEIPV were significantly associated with COPD. In our study, the associations with CPA and CEIPV persisted in the fully adjusted models but not for CSA, while in Cunningham et al’s study associations with CPA and CSA persisted but not for CEIPV. Among males who never smoked, Cunningham et al found no significant associations between CM and COPD, while in our study the sample size for males with COPD who never smoked was insufficient to examine associations with COPD.
As expected, we found that smoking and mental and substance use disorders were important mediators in associations between CM and COPD. It has been suggested that people use smoking to self-medicate to help cope with the trauma associated with early abusive experiences.9,15 The mental and substance use disorders associated with CM21 make persistent and heavy smoking more likely,22,23 further elevating the risk of COPD.
However, the associations that persisted in the fully adjusted models suggest that other pathways may account for associations between CM and COPD. There is evidence that the trauma associated with CM (particularly severe CM) may result in physiological responses including changes in the developing brain and enhanced sensitivity of the hypothalamic–pituitary–adrenal axis.34–36 These alterations can result in impairment of the body’s immune function35 increasing the risk of respiratory infection during childhood and adolescence. Research suggests that childhood respiratory infections may predispose individuals to develop COPD later in life4,37,38 and possibly these associations would be independent of smoking status.
The sex differences in associations between CM and COPD observed in this study may in part relate to sex differences in the susceptibility to the harmful effects of cigarette smoking and exposure to secondhand smoke. Studies have found that the respiratory damage and reduced lung function associated with cigarette smoking is stronger for females than males even when accounting for smoking intensity levels.39–41 This may explain the higher persistence of associations between CM and COPD for females compared with males in the models that included smokers, former smokers, and those who never smoked, even when controlling for smoking intensity. In addition, there is evidence that there are sex differences in the reporting of CSA; males with documented cases of CSA are less likely to report than their female counterparts.42 This may also have attributed to the sex differences observed in this study.
Strengths and limitations
Strengths of this study include the large representative sample of Canadian adults using multiple CM questions that made it possible for us to examine three types of CM in relation to COPD. In addition, unlike previous studies,7,13,14 we considered severity and frequency for the specific types of maltreatment. The CM items are behavior specific and thus are likely to have higher validity and reliability than broad and subjectively defined questions.43–46 The extensive array of variables collected in the 2012 CCHS-MH made it possible to control for the potentially confounding effects of sociodemographic factors and to examine the mediating effects of smoking status (including smoking intensity and years since quitting) as well as mental and substance use disorders when examining associations between CM and COPD. Previous studies have used more simplistic controls for smoking status (ie, current smoker/former smoker).7,13,14 This would tend to underestimate the importance of the mediation role of smoking in the association between CM and COPD since heavy smoking and persistent smoking15,16,18 elevate the risk of COPD.19,20
This study has some limitations that should be considered when interpreting results. All information collected was based on self-reports. Recall and other response biases may have affected associations between CM, smoking status, and COPD. A review of the literature on the validity of adult retrospective reports of adverse childhood experiences indicates that the rate of false negatives can be substantial and that false positive reports are rare.44 A study of the CEVQ concluded that it is a reliable and valid instrument with considerable agreement between self-reported CPA and CSA (including severe forms) and independent reports from clinicians.29 Although the behavior-specific CM items used in the CCHS-MH may have reduced the rate of false negatives in this study, the assessed types of CM may still have been underestimated. For CSA, a better indication of severity would have separated attempted and actual forced sexual activity.
In the CCHS-MH, COPD was assessed in a module that asked respondents to report on long-term health conditions lasting 6 months or more that had been diagnosed by a health professional.47 The validity of self-reported diagnosed COPD has been examined by making comparisons with spirometry measures of airflow obstruction.48,49 Although specificity is high (meaning that most people who report having been diagnosed with COPD have spirometry measures indicating airflow obstruction), sensitivity is low (meaning that many people who reported that they have not been diagnosed with COPD have spirometry results indicative of COPD).48,49 In Canada, it has been estimated that the prevalence of COPD is two to six times higher when based on spirometry-measured airflow obstruction compared with prevalence based on self-reported diagnosis.48
In contrast, a study comparing self-reported smoking status with a measure of urinary cotinine (a biomarker of exposure to tobacco smoke) concluded that accurate estimates of smoking status in the Canadian population can be derived from self-reported data.50 Among adults, sensitivity and specificity were >90%.
Finally, it is possible that the observed associations may be attributable to unmeasured factors such as childhood socioeconomic status, other childhood family adversities such as neglect and emotional abuse, and other risk factors for COPD such as occupational exposures and exposure to secondhand smoke and air pollution.
In spite of these limitations, our study suggests that there are significant associations between CM and COPD, which are largely mediated through smoking. It is unknown to what extent addressing these limitations would impact the observed findings.
Conclusion
The findings from this study establish CM as a risk factor for COPD in adulthood. Although a large part of the association is attributable to cigarette smoking, other factors such as the trauma associated with CM and environmental factors may also play a role. Among smokers, the single most important step that can be taken to slow the progression of COPD is to quit smoking.51 For victims of CM, this can be a difficult journey; smokers with a history of CM are less likely to quit smoking even after being diagnosed with a debilitating condition such as COPD.18 Mental illness is another important barrier to smoking cessation, and since mental and substance use disorders are common among individuals with a history of CM21 successful smoking cessation may be particularly challenging. These findings underscore the importance of interventions to prevent CM as well as programs specifically tailored to assist victims of CM to deal with their tobacco addictions. Further research is warranted to gain more insight into the association between CM and COPD among females who never smoked.
Acknowledgment
The assistance of Dr Deepa P Rao and Dr Heather Orpana (from the Public Health Agency of Canada) in providing analytical guidance is gratefully acknowledged.
Disclosure
The authors report no conflicts of interest in this work.
References
Public Health Agency of Canada. Life and Breath: Respiratory Disease in Canada. Ottawa: Public Health Agency of Canada; 2007. | ||
Silverman EK, Speizer FE. Risk factors for the development of chronic obstructive pulmonary disease. Med Clin North Am. 1996;80(3):501–522. | ||
Canadian Thoracic Society. The Human and Economic Burden of COPD: A Leading Cause of Hospital Admission in Canada. Ottawa, Ontario: Canadian Thoracic Society; 2010. | ||
Salvi SS, Barnes PJ. Chronic obstructive pulmonary disease in non-smokers. Lancet. 2009;374(9691):733–743. | ||
Kuh D, Ben-Shlomo Y, Lynch J, Hallqvist J, Power C. Life course epidemiology. J Epidemiol Community Health. 2003;57(10):778–783. | ||
Shonkoff JP, Boyce WT, McEwen BS. Neuroscience, molecular biology, and the childhood roots of health disparities: building a new framework for health promotion and disease prevention. JAMA. 2009;301(21):2252–2259. | ||
Springer KW. Childhood physical abuse and midlife physical health: testing a multi-pathway life course model. Soc Sci Med. 2009;69(1):138–146. | ||
Draper B, Pfaff JJ, Pirkis J, et al. Long-term effects of childhood abuse on the quality of life and health of older people: results from the depression and early prevention of suicide in general practice project. J Am Geriatr Soc. 2008;56(2):262–271. | ||
Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14(4):245–258. | ||
Gonzalez A, Boyle MH, Kyu HH, Georgiades K, Duncan L, MacMillan HL. Childhood and family influences on depression, chronic physical conditions, and their comorbidity: findings from the Ontario Child Health Study. J Psychiatr Res. 2012;46(11):1475–1482. | ||
Goodwin RD, Stein MB. Association between childhood trauma and physical disorders among adults in the United States. Psychol Med. 2004;34(3):509–520. | ||
Scott KM, Von Korff M, Angermeyer MC, et al. Association of childhood adversities and early-onset mental disorders with adult-onset chronic physical conditions. Arch Gen Psychiatry. 2011;68(8):838–844. | ||
Anda RF, Brown DW, Dube SR, Bremner JD, Felitti VJ, Giles WH. Adverse childhood experiences and chronic obstructive pulmonary disease in adults. Am J Prev Med. 2008;34(5):396–403. | ||
Cunningham TJ, Ford ES, Croft JB, Merrick MT, Rolle IV, Giles WH. Sex-specific relationships between adverse childhood experiences and chronic obstructive pulmonary disease in five states. Int J Chron Obstruct Pulmon Dis. 2014;9:1033–1042. | ||
Anda RF, Croft JB, Felitti VJ, et al. Adverse childhood experiences and smoking during adolescence and adulthood. JAMA. 1999;282(17):1652–1658. | ||
Tonmyr L, Thornton T, Draca J, Wekerle C. The childhood maltreatment and adolescent substance use relationship: a critical review. Curr Psychiatric Rev. 2010;6(3):223–234. | ||
Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173–1182. | ||
Edwards VJ, Anda RF, Gu D, Dube SR, Felitti VJ. Adverse childhood experiences and smoking persistence in adults with smoking-related symptoms and illness. Perm J. 2007;11(2):5–13. | ||
U.S. Department of Health and Human Services. The Health Consequences of Smoking: A report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centres for Disease Control and Prevention, National Centre for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2004. | ||
U.S. Department of Health and Human Services. Preventing Tobacco Use among Youth and Young Adults: A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centres for Disease Control and Prevention, National Centre for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2012. | ||
Afifi TO, MacMillan HL, Boyle M, Taillieu T, Cheung K, Sareen J. Child abuse and mental disorders in Canada. CMAJ. 2014;186(9):E324–E332. | ||
Lasser K, Boyd JW, Woolhandler S, Himmelstein DU, McCormick D, Bor DH. Smoking and mental illness: a population-based prevalence study. JAMA. 2000;284(20):2606–2610. | ||
Mackowick KM, Lynch MJ, Weinberger AH, George TP. Treatment of tobacco dependence in people with mental health and addictive disorders. Curr Psychiatry Rep. 2012;14(5):478–485. | ||
MacMillan HL, Fleming JE, Streiner DL, et al. Childhood abuse and lifetime psychopathology in a community sample. Am J Psychiatry. 2001;158(11):1878–1883. | ||
Molnar BE, Buka SL, Kessler RC. Child sexual abuse and subsequent psychopathology: results from the National Comorbidity Survey. Am J Public Health. 2001;91(5):753–760. | ||
Thompson MP, Kingree JB, Desai S. Gender differences in long-term health consequences of physical abuse of children: data from a nationally representative survey. Am J Public Health. 2004;94(4):599–604. | ||
Widom CS, White HR, Czaja SJ, Marmorstein NR. Long-term effects of child abuse and neglect on alcohol use and excessive drinking in middle adulthood. J Stud Alcohol Drugs. 2007;68(3):317–326. | ||
Statistics Canada. Canadian Community Health Survey (CCHS) – Mental Health User Guide. Statistics Canada: Ottawa; 2013. | ||
Walsh CA, MacMillan HL, Trocmé N, Jamieson E, Boyle MH. Measurement of victimization in adolescence: development and validation of the Childhood Experiences of Violence Questionnaire. Child Abuse Negl. 2008;32(11):1037–1057. | ||
Statistics Canada [webpage on the Internet]. General Social Survey – Victimization (GSS). 2014. Available from: http://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&SDDS=4504. Accessed November 1, 2015. | ||
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Third Edition. Washington, DC: American Psychiatric Association; 1980. | ||
MacKinnon DP, Dwyer JH. Estimating mediating effects in prevention studies. Evaluation Rev. 1993;17(2):144–158. | ||
Menard S. Applied Logistic Regression Analysis. 2nd ed. Thousand Oakes, CA: Sage; 2002. | ||
Bremner JD, Vythilingam M, Vermetten E, et al. Cortisol response to a cognitive stress challenge in posttraumatic stress disorder (PTSD) related to childhood abuse. Psychoneuroendocrinology. 2003;28(6):733–750. | ||
Heim C, Nemeroff CB. Neurobiology of early life stress: clinical studies. Semin Clin Neuropsychiatry. 2002;7(2):147–159. | ||
Liu D, Diorio J, Tannenbaum B, et al. Maternal care, hippocampal glucocorticoid receptors, and hypothalamic-pituitary-adrenal responses to stress. Science. 1997;277(5332):1659–1662. | ||
Britton J, Martinez FD. The relationship of childhood respiratory infection to growth and decline in lung function. Am J Respir Crit Care Med. 1996;154(6 pt 2):S240–S245. | ||
Martinez FD. Role of respiratory infection in onset of asthma and chronic obstructive pulmonary disease. Clin Exp Allergy. 1999;29(suppl 2):53–58. | ||
Chen Y, Horne SL, Dosman JA. Increased susceptibility to lung dysfunction in female smokers. Am Rev Respir Dis. 1991;143(6):1224–1230. | ||
Langhammer A, Johnsen R, Gulsvik A, Holmen TL, Bjermer L. Sex differences in lung vulnerability to tobacco smoking. Eur Respir J. 2003;21(6):1017–1023. | ||
Sørheim IC, Johannessen A, Gulsvik A, Bakke PS, Silverman EK, DeMeo DL. Gender differences in COPD: are women more susceptible to smoking effects than men? Thorax. 2010;65(6):480–485. | ||
Widom CS, Morris S. Accuracy of adult recollections of childhood victimization: part 2. Childhood sexual abuse. Psychol Assess. 1997;9(1):23–46. | ||
Fisher HL, Craig TK, Fearon P, et al. Reliability and comparability of psychosis patients’ retrospective reports of childhood abuse. Schizophr Bull. 2011;37(3):546–553. | ||
Hardt J, Rutter M. Validity of adult retrospective reports of adverse childhood experiences: review of the evidence. J Child Psychol Psychiatry. 2004;45(2):260–273. | ||
Monteiro IS, Maia A. Family childhood experiences reports in depressed patients: comparison between 2 time points. Procedia Soc Behav Sci. 2010;5:541–547. | ||
Thombs BD, Bernstein DP, Ziegelstein RC, et al. An evaluation of screening questions for childhood abuse in 2 community samples: implications for clinical practice. Arch Intern Med. 2006;166(18):2020–2026. | ||
Statistics Canada [webpage on the Internet]. Canadian Community Health Survey (CCHS) – Mental Health. 2015. Available from: www.statcan.gc.ca/imdb-bmdi/5015-eng.htm. Accessed January 1, 2015. | ||
Evans J, Chen Y, Camp PG, Bowie DM, McRae L. Estimating the prevalence of COPD in Canada: reported diagnosis versus measured airflow obstruction. Health Rep. 2014;25(3):3–11. | ||
Murgia N, Brisman J, Claesson A, Muzi G, Olin AC, Torén K. Validity of a questionnaire-based diagnosis of chronic obstructive pulmonary disease in a general population-based study. BMC Pulm Med. 2014;14:49. | ||
Wong SL, Shields M, Leatherdale S, Malaison E, Hammond D. Assessment of validity of self-reported smoking status. Health Rep. 2012;23(1):47–53. | ||
U.S. Department of Health and Human Services. The Health Benefits of Smoking Cessation. A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centres for Disease Control and Prevention, National Centre for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 1990. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.