Back to Journals » Clinical Interventions in Aging » Volume 18
Characteristics of Preoperative Acute Myocardial Infarction in Elderly Hip Fracture Patients and Construction of a Clinical Prediction Model: A Retrospective Cohort Study
Authors Zhang Y, Liu Y, Fu M, Wang Z, Hou Z
Received 29 June 2023
Accepted for publication 7 October 2023
Published 29 November 2023 Volume 2023:18 Pages 1985—1994
DOI https://doi.org/10.2147/CIA.S428092
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Maddalena Illario
Yaqian Zhang,1,* Yan Liu,2,* Mingming Fu,1 Zhiqian Wang,1 Zhiyong Hou2,3
1Department of Geriatric Orthopedics, The Third Hospital of Hebei Medical University, Shijiazhuang, Hebei, People’s Republic of China; 2Department of Orthopaedic Surgery, The Third Hospital of Hebei Medical University, Shijiazhuang, Hebei, People’s Republic of China; 3NHC Key Laboratory of Intelligent Orthopaedic Equipment (The Third Hospital of Hebei Medical University), Shijiazhuang, Hebei, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Zhiqian Wang, Third Hospital of Hebei Medical University Department of Geriatric Orthopedics, Shijiazhuang, Hebei, 050051, People’s Republic of China, Email [email protected] Zhiyong Hou, Third Hospital of Hebei Medical University Department of Orthopaedic Surgery, Shijiazhuang, Hebei, 050051, People’s Republic of China, Email [email protected]
Background: The prognosis of elderly patients with acute myocardial infarction (AMI) is poor, and this study aimed to investigate the characteristics and predictors of preoperative AMI in elderly hip fracture patients and to propose a valid clinical prediction model.
Methods: We collected clinical data of older hip fracture patients from January 2019 to December 2020. The data collected include demographic and clinical characteristics, underlying diseases and laboratory results. In AMI patients, we further collected type of myocardial infarctions, clinical symptoms, electrocardiogram (ECG), Killip class and diagnosis method. The prediction model was constructed by using Least absolute shrinkage and selection operator (LASSO) regression and multivariate logistic regression analyses. In addition, the constructed prediction model was transformed into a nomogram. The performance of the model was evaluated using the area under receiver operating characteristic curve (AUC), calibration curve, and decision curve analysis (DCA). Bootstrapping was used for validation.
Results: There are 40 (4.2%) cases developed AMI in all 958 patients. There were 685 (71.5%) female patients and 273 (28.5%) male patients. Among 40 AMI patients, 38 (95.0%) had Type 2 myocardial infarction (T2MI) and 2 (5.0%) had Type 1 myocardial infarction (T1MI). The majority of these ECG were ST segment depression (57.5%). Most elderly AMI patients (67.5%) presented asymptomatic. Predictors for preoperative AMI were higher age (OR 2.386, 95% CI 1.126– 5.057), diabetes (OR 5.863, 95% CI 2.851– 12.058), Hb≤ 100 g/L (OR 3.976, 95% CI 1.478– 10.695), CRP≥ 40 mg/L (OR 6.998, 95% CI 2.875– 17.033), and ALB≤ 35 g/L (OR 2.166, 95% CI 1.049– 4.471). Good discrimination and calibration effect of the model was showed. Interval validation could still achieve the C-index value of 0.771. DCA demonstrated this nomogram has good clinical utility.
Conclusion: This model has a good predictive effect on preoperative AMI in elderly patients with hip fracture, which can help to better plan clinical evaluation.
Keywords: hip fracture, myocardial infarction, characteristics, prediction model
Introduction
Osteoporosis-related hip fracture is common serious disease in older adults and associated with higher disability, mortality and economic costs.1 It has been estimated the number of hip fractures in women and men will increase 3.5 times by 2025, owing to fast population growth.2,3 A study found that the mortality in the first year after hip fracture of elderly patients was 22–30%.4
Researches have suggested that the complications after fracture may carry a high burden and mortality in older patients.5,6 Among all the complications, AMI is one of the most devastating complications in hip fracture population.7 Additional studies have shown that the incidence of perioperative AMI of non-cardiac surgery ranges from 6% to 36%8,9, and this has been associated with a higher mortality.10 A recent study found that hip fracture confers higher risk of subsequent AMI.11 Shea et al found that the rate of early postoperative MI within the first seven days of surgery was 10.4%.12 Several investigations demonstrated that postoperative MI significantly affects length of hospitalization, hospital mortality early and long-term mortality.8,13 The study mentioned that most perioperative AMI in elderly patients were asymptomatic or presented with atypical ischemic symptoms,14 which adds substantial difficulty to the diagnosing AMI. More attention should focus on these AMI patients. In addition, earlier studies on AMI related to hip fracture focus on patients with postoperative AMI after fracture surgery,15,16 while there are few studies on preoperative acute myocardial infarction.
In our study, we identified the characteristics of older hip fracture patients who developed AMI before fracture surgery. Furthermore, we constructed a LASSO regression and multivariate logistic regression analysis to predict individual risks and propose an effective clinical prediction model for preoperative AMI.
Materials and Methods
Patients and Groups
In this retrospective study, we collected data in the Third Hospital of Hebei Medical University from January 2019 to December 2020. The older adults (age ≥ 65) with hip fracture whose hospital admission less than 48 hours were included in our study. The study protocol was approved by the Institutional Review Board of the Third Hospital of Hebei Medical University with an informed waiver. The inclusion criteria were: (1) age ≥65; (2) Patients with hip fracture; (3) the injury time of hip fractures was ≤48 h before admission. The exclusion criteria were: (1) age <65; (2) the time of hip fracture injury was >48 h before admission incomplete medical information; (3) patients who had multiple fracture, periprosthetic fracture, or pathological fracture; (4) incomplete medical information. AMI was diagnosed as elevated troponin I > 99% of the upper reference limit (0.04 ng/mL) and must meet at least one of the following criteria: (1) new ischemic ECG changes (ST segment elevation or depression, evolutionary Q-wave, T waves symmetric inversion); (2) ischemic symptoms; (3) the abnormal imaging evidence of new myocardial loss or new regional wall motion.17 Patients with hip fracture were divided into two groups: AMI group and No-AMI group.
Data Collection
The information we collected contain gender, age, and fracture types, comorbidities, and laboratory data on admission. Laboratory data included white blood cell (WBC), Hb, ALb, CRP and blood glucose (Glu) levels. In AMI group, we further collected troponin I level, types of myocardial infarction, clinical symptoms, ECG, Killip class and diagnosis method. According to the pathological and clinical differences,18 AMI was classified into T1MI and T2MI. ECG could be shown as: ST segment elevation or depression, T wave inversion, and no new ST segment abnormalities. Killip class was categorized as Killip I, II, III, IV. The clinical symptoms include chest distress, chest pain, palpitations, nausea and vomiting, hypotension and no obvious symptoms.
Statistical Analysis
The statistical analyses were performed by IBM SPSS Statistics version 26.0 (IBM Corp, Armonk, NY) and R software version 4.2.1 and the “glmnet” package (R Foundation for Statistical Computing, Vienna, Austria). Continuous parametric variables were presented as mean ± standard deviation using Student’s t-test or analysis of variance while Categorical variables were shown as numbers and percentages and compared using the chi-square test or Fisher’s exact test. The prediction model was developed by LASSO and multivariable logistic regression and draw a nomogram. Area under the curve (AUC) of receiver operating characteristic curve (ROC) analysis was performed in order to assess how accurate the nomogram was at predicting risk. The calibration curve and decision curve analysis were used to assess calibration and clinical value of the nomogram separately. The level of significance was set at p < 0.05.
Results
The Characteristics of AMI
The characteristics of AMI are shown in Table 1. The types of AMI in older hip fracture patients were T1MI (5.0%) and T2MI (95.0%). The ECGs from these patients at first presentation showed ST segment depression (57.5%) and new T wave inversion (20.0%), and only a small proportion of them showed ST segment elevation (5%). In addition, 17.5% patients showed no new ST segment abnormalities. More than 2/3 of patients were asymptomatic (67.5%), other symptoms include chest tightness (10.0%), chest pain (7.5%), palpitations (7.5%), hypotension, nausea and vomiting (5.0%) and hypotension (2.5%). In these cases, there were 24(60.0%), 10(25.0%), 4(10.0%), and 2(5.0%) patients with killip I, killip II, killip III and killip IV, respectively. Twenty patients had a well-established coronary angiogram after AMI, 10 patients had a well-established coronary CTA, and 10 patients did not have both tests.
 |
Table 1 The Characteristics of AMI |
The Comparison of the AMI Group and No-AMI Group
As shown in Table 2, 40 (4.2%) occurred preoperative AMI. There were 958 patients were enrolled in our study, including 273 men and 685 women. The average age was 79.5 years old. Patients with AMI were older (age ≥ 80, p = 0.030) than no-AMI patients. AMI patients had more comorbidities than non-AMI patients (p = 0.001), which include hypertension (p = 0.041), CHD (p = 0.021) and diabetes (p = 0.000). There were no differences in sex and fracture type between the AMI and no-AMI groups (p = 0.198, p = 0.483). In addition, among AMI patients, CRP on admission was higher (p = 0.000) and albumin lower (p = 0.000) compared with the non AMI ones. Other laboratory results showed no differences were considered significant (p > 0.05).
 |
Table 2 The Comparison of the AMI Group and No-AMI Group |
Selection of Variables as Predictors and Derivation and Evaluation of the Prediction Model
LASSO regression initially included 15 variables, but eventually included 7 candidate variables that were significantly associated with AMI (age ≥ 80, CHD, diabetes, comorbidities ≥3, Hb≤100g/L, CRP≥40mg/L, ALb≤35g/L) were included (Figure 1a). When log (λ) = −4.4830 and λ = 0.0113, the five risk factor weights were analyzed with the logistic regression model (Figure 1b). Table 3 summarizes the findings of the analysis among higher age (OR 2.386, 95% CI 1.126–5.057), diabetes (OR 5.863, 95% CI 2.851–12.058), Hb ≤ 100 g/L (OR 3.976, 95% CI 1.478–10.695), CRP ≥ 40 mg/L (OR 6.998, 95% CI 2.875–17.033), and ALB ≤ 35 g/L (OR 2.166, 95% CI 1.049–4.471). By combining these independent predictors, a model was built and presented as a nomogram (shown in Figure 2). Calibration curves used for estimating preoperative AMI in hip fracture patients showed good agreement across the cohort. The AUC for the predictive nomogram model was 0.771 (95% CI 0697–0.846) (shown in Figure 3). With a p value of 0.783. The calibration curve indicated a good calibration effect of the nomogram. The internal validation C-index using bootstrapping (resampling = 1000) is 0.771. DCA demonstrated this nomogram has good clinical utility (shown in Figure 4).
 |
Table 3 Prediction Factors of Preoperative AMI in Elderly Patients After Hip Fracture |
 |
Figure 2 A model of risk prediction for AMI. |
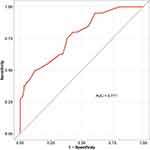 |
Figure 3 Analysis of ROC curve for the predictive values of preoperative AMI. |
 |
Figure 4 (a) Calibration curves of nomogram; (b) calibration curves of nomogram; (c) decision curve analysis of nomogram. |
Discussion
There were 40 (4.2%) older patients occurred AMI in 958 cases. The incidence of AMI after fracture was 4.2%. Among 40 AMI patients, T2MI was the most common type of myocardial infarction. The ECG of AMI in such patients mostly showed ST segment depression. 67.5% AMI patients were asymptomatic. The Killip class of the AMI was mostly Killip I. Five prediction factors constitute the prediction model, including Higher age, combined with diabetes, Hb ≤ 100 g/L, CRP ≥ 40 mg/L, and ALB ≤ 35 g/L, which are easily available in clinical practice. The nomogram could predict the preoperative AMI risk in hip fracture patients accurately.
AMI is a complication associated with adverse outcomes of hip fracture patients, particularly in older adults. There is also evidence that risk factors for fracture and CVD overlap considerably.19 A recent study found that hip fracture was associated with an increased risk of AMI.11 We suggest that the development of AMI after fracture in the elderly is associated with greater traumatic stress. The physical inactivity, blood loss, pain and fear after fracture increases the release of stress hormones such as thyroxine, glucagon, epinephrine, glucocorticoids and others,20 which can exacerbate pre-existing cardiovascular risk. We think this contributed to the development of AMI after hip fracture. Our study differs from previous studies, the AMI that occurred with hip fracture in our study was prior to hip surgery. The proportion of AMI after hip fracture was 4.2%. According to pathological and clinical differences, myocardial infarction is classified into different types. Patients with AMI were classified classified as T1MI and T2MI in our study, and the AMI patients mostly had T2MI. T1MI is an atherosclerotic thrombus due to plaque rupture or erosion, while T2MI results from an imbalance of myocardial oxygen supply–demand imbalance without atherothrombosis.18 On the basis of the original stenosis, stress reactions such as anemia and pain after fracture will aggravate ischemia, leading to the occurrence of T2MI. Patients with T2MI were older and had a higher proportion of women than men compared with patients with T1MI.18 This result overlapped with our results. In our study, some clinical symptoms of AMI patients were not obvious. This result is consistent with studies by others.21 Their ECGs were mostly in fact of ST segment depression, and about 1/3 of them was asymptomatic. A study has shown that silent AMI occurred more frequently in patients with diabetes.18 We think that this also may be related to cognitive decline in the elderly.22 The clinical symptoms of these patients were atypical and could be easily missed, which needs to draw our attention.
In our study, higher age, combined with diabetes were significant predictors of preoperative AMI. Numerous studies show that advancing age is one of the main causes for the increased incidence of fractures and perioperative complications.23,24 This may be due to the poorer health conditions and more underlying diseases in elderly people than younger individuals.25 We obtained the same result in old AMI patients with hip fracture. The elderly hip fracture patients with AMI have a variety of underlying diseases, including hypertension, diabetes, CHD, etc. Hypertension and diabetes are the main risk factors for AMI,26 which accelerate the progression of atherosclerosis. The formation and progression of atherosclerotic plaques is the major pathological basis of the cardio-cerebrovascular diseases.27 Moreover, additional studies determined that patients with diabetes or stress-induced hyperglycemia were at increased risk of cardiac complications after hip fracture surgery.20,28 Our results suggest that diabetes also has an important predictive role for preoperative AMI.
Hb≤100g/L, CRP≥40mg/L, and ALb≤35 g/L also were significant predictors of preoperative AMI. CRP is a general stress-response protein, which is produced in response to inflammation.29 CRP is considered to be a marker of atherosclerosis and CHD, and plays an important role in the formation of plaque in the arterial wall and the initiation of cardiovascular and cerebrovascular events.30 Acute trauma after fracture leads to a systemic inflammatory response, and inflammatory factors such as CRP and IL-6 subsequently increase.31 This may initiate and exacerbate myocardial injury that can lead to AMI. The studies documented that anemia or low hemoglobin levels on admission increased the risk of CVD and fracture in older adults.32,33 Anemia is more likely to cause T2MI,34 and we obtained the same results in patients with AMI after fracture. Hypoalbuminemia occurs in nearly 50% of elderly hip fracture patients and is associated with the development of perioperative complications and an increased risk of mortality.35,36 At present, the mechanism of perioperative acute myocardial infarction is not very clear. Some studies believe that it may be related to the strong stress suffered after fracture, sympathetic nerve excitation induces increased release of glucocorticoids, glucagon, epinephrine and other hormones, which can accelerate the production of oxygen-free radicals, damage cardiomyocytes, cause myocardial stunning and can also lead to microvascular contraction, endothelial function damage, affect cardiac function and promote microcirculation dysfunction and thrombosis, and ultimately leading to perioperative myocardial ischemia and injury.37 Immuno-inflammatory promoted production of inflammatory cytokines and superoxide, leading to perioperative myocardial injury. Changes in the metabolic function may lead to anemia, low albumin and others.38 Anemia and hypoproteinemia also increase the risk of perioperative AMI after hip fracture. For this reason, timely monitoring of Hb, Alb, and CRP levels on admission of fracture patients is beneficial for early assessment of the risk of AMI.
Limitations
Our study has some limitations worthy of discussion. First, this is a retrospective study and the inherent limitations of the design seem inevitable. Second, due to the small sample size, there is a possibility of selection bias. The conclusion cannot completely and reliably reflect the general clinical characteristics. Third, patients with AMI after hip fracture surgery were not included in this study. Further studies are needed to compare the different characteristics of AMI after hip fracture and AMI after surgery.
Conclusions
In summary, we observed that the overall incidence of perioperative AMI in older patients with hip fracture was 4.2%. Higher age, combined with diabetes, Hb≤100g/L, CRP≥40mg/L, and ALB≤35 g/L were the independent risk factors for perioperative AMI, and a readable nomogram is further formed to facilitate its use in practice, thus reducing the potential risk of AMI. Future prospective and multicenter design studies will help validate our findings.
Abbreviations
AMI, Acute Myocardial Infarction; ECG, Electrocardiogram; LASSO, Least absolute shrinkage and selection operator; AUC, Area under receiver operating characteristic curve; DCA, Decision curve analysis; CHD, Coronary heart disease; Hb, Hemoglobin; CRP, C-reactive protein; Alb, Albumin; T1MI, Type 1 myocardial infarction; T2MI, Type 2 myocardial infarction; WBC, White blood cell; Glu, Blood glucose; CVD, Cardiovascular disease; coronary CTA, Coronary computed tomographic angiography.
Data Sharing Statement
The data used to support the findings of this study are available from Zhiqian Wang upon request.
Ethical Approval and Informed Consent
This study was approved by the institutional review board of the third Hospital of Hebei Medical University in compliance with the Helsinki and an exemption from the informed consent was obtained. All data were anonymized before the analysis to safeguard patient privacy.
Funding
This study was supported by the 2021 clinical medical talent training program funded by the Hebei provincial government.
Disclosure
The authors declared no potential conflicts of interest in this work.
References
1. Bolton JM, Morin SN, Majumdar SR, et al. Association of mental disorders and related medication use with risk for major osteoporotic fractures. JAMA psychiatry. 2017;74(6):641–648. doi:10.1001/jamapsychiatry.2017.0449
2. Silva AM, Moura SR, Teixeira JH, et al. Long noncoding RNAs: a missing link in osteoporosis. Bone Res. 2019;7:10. doi:10.1038/s41413-019-0048-9
3. Pereira SR, Puts MT, Portela MC, et al. The impact of prefracture and hip fracture characteristics on mortality in older persons in Brazil. Clin Orthop Relat Res. 2010;468(7):1869–1883. doi:10.1007/s11999-009-1147-5
4. Zhang C, Feng J, Wang S, et al. Incidence of and trends in hip fracture among adults in urban China: a nationwide retrospective cohort study. PLoS Med. 2020;17(8):e1003180. doi:10.1371/journal.pmed.1003180
5. Tyagi AM, Yu M, Darby TM, et al. The microbial metabolite butyrate stimulates bone formation via T regulatory cell-mediated regulation of WNT10B expression. Immunity. 2018;49(6):1116–31.e7. doi:10.1016/j.immuni.2018.10.013
6. Nathan K, Lu LY, Lin T, et al. Precise immunomodulation of the M1 to M2 macrophage transition enhances mesenchymal stem cell osteogenesis and differs by sex. Bone Joint Res. 2019;8(10):481–488. doi:10.1302/2046-3758.810.BJR-2018-0231.R2
7. Rostagno C, Cartei A, Rubbieri G, et al. Perioperative myocardial infarction/myocardial injury is associated with high hospital mortality in elderly patients undergoing hip fracture surgery. J Clin Med. 2020;9(12):4043. doi:10.3390/jcm9124043
8. Puelacher C, Lurati Buse G, Seeberger D, et al. Perioperative myocardial injury after non-cardiac surgery: incidence, mortality, and Characterization. Circulation. 2018;137(12):1221–1232. doi:10.1161/CIRCULATIONAHA.117.030114
9. van Waes JA, Nathoe HM, de Graaff JC, et al. Myocardial injury after noncardiac surgery and its association with short-term mortality. Circulation. 2013;127(23):2264–2271. doi:10.1161/CIRCULATIONAHA.113.002128
10. Nagele P, Brown F, Gage BF, et al. High-sensitivity cardiac troponin T in prediction and diagnosis of myocardial infarction and long-term mortality after noncardiac surgery. Am Heart J. 2013;166(2):325–32.e1. doi:10.1016/j.ahj.2013.04.018
11. Chiang CH, Liu CJ, Chen PJ, et al. Hip fracture and risk of acute myocardial infarction: a nationwide study. J Bone Miner Res. 2013;28(2):404–411. doi:10.1002/jbmr.1714
12. Huddleston JM, Gullerud RE, Smither F, et al. Myocardial infarction after hip fracture repair: a population-based study. J Am Geriatr Soc. 2012;60(11):2020–2026. doi:10.1111/j.1532-5415.2012.04205.x
13. Izhaki A, Slesarenko Y, Boaz M, et al. Cardiac troponin T: an important predictor of late death and myocardial infarction following hip fracture: an eight year prospective observational cohort study. Eur J Orthop Surg Traumatol. 2011;21:243–249. doi:10.1007/s00590-010-0696-3
14. Hu W, Zhao K, Chen Y, et al. Characteristics and long-term mortality of patients with ST-elevation or non-ST-elevation myocardial infarction after orthopaedic surgery. J Int Med Res. 2021;49(3):300060521992995. doi:10.1177/0300060521992995
15. Gupta BP, Huddleston JM, Kirkland LL, et al. Clinical presentation and outcome of perioperative myocardial infarction in the very elderly following hip fracture surgery. J Hosp Med. 2012;7(9):713–716. doi:10.1002/jhm.1967
16. Rostagno C, Peris A, Polidori GL, et al. Perioperative myocardial infarction in elderly patients with Hip fracture. Is there a role for early coronary angiography? Int J Cardiol. 2019;284:1–5. doi:10.1016/j.ijcard.2018.10.095
17. Thygesen K, Alpert JS, Jaffe AS, et al. Fourth universal definition of myocardial infarction (2018). J Am Coll Cardiol. 2018;72(18):2231–2264. doi:10.1016/j.jacc.2018.08.1038
18. Chapman AR, Shah ASV, Lee KK, et al. Long-term outcomes in patients with type 2 myocardial infarction and myocardial injury. Circulation. 2018;137(12):1236–1245. doi:10.1161/CIRCULATIONAHA.117.031806
19. Paccou J, D’Angelo S, Rhodes A, et al. Prior fragility fracture and risk of incident ischaemic cardiovascular events: results from UK Biobank. Osteoporos Int. 2018;29(6):1321–1328. doi:10.1007/s00198-018-4426-8
20. Chen Y, Yang X, Meng K, et al. Stress-induced hyperglycemia after hip fracture and the increased risk of acute myocardial infarction in nondiabetic patients. Diabetes Care. 2013;36(10):3328–3332. doi:10.2337/dc13-0119
21. Hietala P, Strandberg M, Strandberg N, et al. Perioperative myocardial infarctions are common and often unrecognized in patients undergoing hip fracture surgery. J Trauma Acute Care Surg. 2013;74(4):1087–1091. doi:10.1097/TA.0b013e3182827322
22. Weng W, Liang J, Xue J, et al. The transfer effects of cognitive training on working memory among Chinese older adults with mild cognitive impairment: a randomized controlled trial. Front Aging Neurosci. 2019;11:212. doi:10.3389/fnagi.2019.00212
23. Ensrud KE, Kats AM, Boyd CM, et al. Association of disease definition, comorbidity burden, and prognosis with hip fracture probability among late-life women. JAMA Intern Med. 2019;179(8):1095–1103. doi:10.1001/jamainternmed.2019.0682
24. Aloisi A, Tseng JH, Sandadi S, et al. Is robotic-assisted surgery safe in the elderly population? An analysis of gynecologic procedures in patients ≥ 65 years old. Ann Surg Oncol. 2019;26(1):244–251. doi:10.1245/s10434-018-6997-1
25. Jiang YQ, Wang ZX, Deng YN, et al. Efficacy of hepatic resection vs. radiofrequency ablation for patients with very-early-stage or early-stage hepatocellular carcinoma: a population-based study with stratification by age and tumor size. Front Oncol. 2019;9:113. doi:10.3389/fonc.2019.00113
26. Kim H, Choi HY, Kim YH, et al. Pharmacokinetic interactions and tolerability of rosuvastatin and ezetimibe: an open-label, randomized, multiple-dose, crossover study in healthy male volunteers. Drug Des Devel Ther. 2018;12:815–821. doi:10.2147/DDDT.S158408
27. Hu Z, Hui B, Hou X, et al. APE1 inhibits foam cell formation from macrophages via LOX1 suppression. Am J Transl Res. 2020;12(10):6559–6568.
28. Norris R, Parker M. Diabetes mellitus and Hip fracture: a study of 5966 cases. Injury. 2011;42:1313–1316. doi:10.1016/j.injury.2011.03.021
29. Vogel CF, Sciullo E, Wong P, et al. Induction of proinflammatory cytokines and C-reactive protein in human macrophage cell line U937 exposed to air pollution particulates. Environ Health Perspect. 2005;113(11):1536–1541. doi:10.1289/ehp.8094
30. Berger E, Castagné R, Chadeau-Hyam M, et al. Multi-cohort study identifies social determinants of systemic inflammation over the life course. Nat Commun. 2019;10(1):773. doi:10.1038/s41467-019-08732-x
31. Peña JM, Aspberg S, MacFadyen J, et al. Statin therapy and risk of fracture: results from the Jupiter randomized clinical trial. JAMA Intern Med. 2015;175(2):171–177. doi:10.1001/jamainternmed.2014.6388
32. Meng Y, Fu M, Guo J, et al. Characteristics and complications of fracture in older adults with chronic kidney disease: a cross-sectional study. J Orthop Surg Res. 2022;17(1):377. doi:10.1186/s13018-022-03253-8
33. Teng Y, Teng Z, Xu S, et al. The analysis for anemia increasing fracture risk. Med Sci Monit. 2020;26:e925707. doi:10.12659/MSM.925707
34. Miller-Hodges E, Anand A, Shah ASV, et al. High-sensitivity cardiac troponin and the risk stratification of patients with renal impairment presenting with suspected acute coronary syndrome. Circulation. 2018;137(5):425–435. doi:10.1161/CIRCULATIONAHA.117.030320
35. He Y, Xiao J, Shi Z, et al. Supplementation of enteral nutritional powder decreases surgical site infection, prosthetic joint infection, and readmission after hip arthroplasty in geriatric femoral neck fracture with hypoalbuminemia. J Orthop Surg Res. 2019;14(1):292. doi:10.1186/s13018-019-1343-2
36. Sim SD, Sim YE, Tay K, et al. Preoperative hypoalbuminemia: poor functional outcomes and quality of life after Hip fracture surgery. Bone. 2021;143:115567. doi:10.1016/j.bone.2020.115567
37. Zhang Y, Fu M, Guo J, et al. Characteristics and perioperative complications of hip fracture in the elderly with acute ischemic stroke: a cross-sectional study. BMC Musculoskelet Disord. 2022;23(1):642. doi:10.1186/s12891-022-05585-2
38. Carpintero P, Caeiro JR, Carpintero R, et al. Complications of hip fractures: a review. World J Orthop. 2014;5(4):402–411. doi:10.5312/wjo.v5.i4.402
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

