Back to Journals » Clinical Optometry » Volume 10
Changes in the morphology of corneal endothelial cells in young myopic adults after 6 months of wearing soft contact lenses: a Malaysian perspective
Authors Ahmad A , Mohd-Ali B , Ishak B
Received 25 April 2018
Accepted for publication 12 June 2018
Published 7 September 2018 Volume 2018:10 Pages 109—113
DOI https://doi.org/10.2147/OPTO.S172272
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Mr Simon Berry
Asmah Ahmad, Bariah Mohd-Ali, Bashirah Ishak
Optometry and Vision Science Program and Centre for Community Health, Faculty of Health Science, Universiti Kebangsaan Malaysia, Kuala Lumpur, Malaysia
Purpose: Soft contact lens wear is most frequently associated with morphologic changes in corneal endothelial cells, but the data are scarce in Asians. This study aimed to evaluate changes in corneal endothelial cell morphology after 6 months of wearing soft hydrogel contact lenses (SH) in young myopic adults living in Kuala Lumpur.
Patients and methods: Forty-eight subjects were included in the study, 24 were fitted with SH contact lenses (A) and the rest were prescribed with glasses (B). Refraction was conducted subjectively and standard contact lens fitting protocol was followed. Corneal endothelial cell morphology (endothelial cell density, ECD; coefficient of variation, COV; cells’ hexagonality, HEX; and central corneal thickness, CCT) was evaluated using specular microscope. Data were collected at baseline and after 6 months of lens wear.
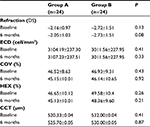
Results: Mean age of all subjects was 21.23±1.30 years. All results are shown at baseline and 6 months, respectively. Mean refraction for A was –2.16±0.97 diopter sphere (DS) and –2.05±1.03 DS (P=0.49); for B was –2.72±1.51 DS and –2.73±1.51 DS (P=0.58). Mean ECD (cell/mm2) for A: 3104.19±237.30 and 3107.23±237.51 (P=0.07); for B: 3011.56±227.95 and 2983.83±244.55 (P=0.33). COV (%) for A: 46.52±8.63 and 48.53±10.65 (P=0.06); for B: 46.93±9.31 and 46.14±10.65 (P=0.88). HEX (%) for A: 46.21±10.12 and 45.15±10.01 (P=0.08); for B: 46.21±10.12 and 45.15±10.01 (P=0.12). CCT (µm) for A: 520.33±0.04 and 525.70±0.05 (P=0.41); for B: 532.00±0.04 µm and 530.00±0.05 µm (P=0.40).
Conclusion: This study found no significant change in corneal endothelial cell morphology after 6 months of wearing SH contact lenses. This is probably due to better oxygen permeability of the contact lens material, good compliance, and short wearing period.
Keywords: corneal endothelial cells, soft contact lens, myope, young adults
Introduction
Endothelium is the extremely thin, innermost layer of the cornea. It is made of a single layer of densely packed flattened cells facing the anterior chamber. Many factors can affect the morphology of corneal endothelial cells including age, contact lens wear, diabetes mellitus, ocular surgery, and race.1,2 Nevertheless, contact lens wear is often associated with the incidence of corneal morphologic changes in young adults.2 Thus, it is important to monitor the changes as these may affect the functions of corneal endothelial cells and cause vision reduction. Previous studies using conventional hydrogel soft contact lenses have shown significant alterations in the corneal endothelial layer.2,3 Hydrogel soft contact lenses with low oxygen permeability can lead to chronic corneal hypoxia, which subsequently leads to changes in the corneal endothelial cell morphology.4 A minimum amount of oxygen must pass through the contact lenses to the cornea to prevent these alterations. Following a mathematical model of oxygen diffusion across the cornea, it is estimated that a minimum level of 125×10−9 (cm2/sec)mL O2/mL × mmHg oxygen transmissibility for extended wear contact lens is needed.5
Lee et al6 analyzed the effect of the morphologic characteristics of the corneal endothelium toward the duration of daily wear soft contact lens wearing periods. They found significant correlation between duration of soft contact lens use and morphologic changes of corneal endothelium. Soft contact lens wearers have significantly greater coefficient of variation in cell size compared to non-contact-lens users. The proportion of hexagonal cells and the mean corneal endothelial cell density (ECD) in those using soft contact lenses for more than 6 years were significantly lower compared to the control group. In an earlier study,4 the authors also showed that increased rate of corneal endothelial polymegathism is associated with the duration of wearing conventional soft hydrogel contact lenses, but the trend was not observed in high oxygen permeability (Dk) silicone hydrogel contact lens wearers.7
Mohidin et al8 investigated the morphologic status of corneal endothelial cells among silicone hydrogel contact lens wearers in Kuala Lumpur who have worn their lenses up to 24 months on daily basis. Their results demonstrated insignificant difference in the morphology of the corneal endothelial cells between the contact lens wearers and non-contact-lens users and concluded that it was probably due to high oxygen permeability of the contact lens materials and short duration of lens wear. Majority of the contact lens wearers in their study wore their lenses approximately 11 hours every day.
The purpose of this study was to describe the effects of wearing soft hydrogel contact lenses for 6 months on corneal endothelial cell morphology in young myopic subjects living in Kuala Lumpur. Soft hydrogel contact lenses are popular in Asia but there are not many reports available on Asian eyes. According to Hamano et al,9 there is a significant difference between Asian and non-Asian eyes in corneal response to oxidative stress. Their results showed that Asian eyes had significantly higher degree of endothelial bleb formation during closed eye conditions than non-Asian population. Doughty10 examined the morphology of the Asian corneal endothelium and concluded that polymegethism is uncommon in healthy young Asian adults. It is possible that ethnicity is a factor in determining corneal response toward contact lens wear but there are limited reports available. In this study, hydrogel contact lenses were fitted on young neophyte myopic subjects and the results were compared to those who were prescribed with glasses. To our knowledge this is the first case–control study that investigated morphologic changes in corneal endothelium following hydrogel contact lens wear in Malaysia. The research protocol was approved by UKM research ethics committee (1.5.3.5/244/NN-133-2014) and followed the tenets of Declaration of Helsinki on the use of human subjects in research.
Materials and methods
The sample size required in this study was calculated using statistical package G*Power version 3.1.9.3 for comparison between two groups with two-tailed test. The test power was set at 0.8 with significant level at 0.05 and the ratio between groups was set at 0.5 with medium effect size. The number of sample size calculated was 16 per group. All subjects were screened using self-administered McMonnies Dry Eye Questionnaires (MDEQ) to exclude dry eye subjects. The questionnaire was invented by Charles McMonnies in 1986 and consists of 12 questions that focus on clinical risk factors of dry eye.11 The questions employ answer options that vary in number and type and provide score from 0 to 45. Each question has a weighted scoring scale and participants must answer all questions and the score of each question was calculated. Scores above 14.5 are consistent with dry eye. The reliability and validity studies of MDEQ have been verified by earlier researchers12,13 and the results are consistent for clinical use.
The inclusion criteria for this study are as follows: neophytes; free from ocular diseases and systemic illnesses; not pregnant or smoking; myopic of ≤–5.50 DS with astigmatism ≤–1.00 DC; and MDEQ score <14.5. Refraction was conducted subjectively using cross cylinder method and visual acuity was evaluated using Log Mar chart. Standard ocular examination and contact lens fitting procedure were conducted for all subjects. Endothelial cell morphology was evaluated in all subjects using noncontact specular microscopy (SP2000, Topcon Corporation, Tokyo, Japan) with a single examiner performing all measurements. The computer automatically evaluated, calculated, and displayed endothelial cell density (ECD) (cell/mm2), coefficient of variation (COV) (%) in cell size, cells’ hexagonality (HEX) (%), and cornea thickness (μm). The room illumination was measured using the illuminance meter (Topcon, Japan). This was to ensure that the room illumination was within the recommended level for photopic vision that is between 480 and 600 lux.14
Selected subjects were divided into two groups: groups A and B. Daily wear soft hydrogel contact lenses (Ocufilcon D 45%, water content 55%) were fitted on subjects in Group A and spectacles were prescribed to subjects in Group B. All measurements were measured at baseline and after 6 months of wearing contact lenses. Maximum wearing hours recommended to subjects were between 8 and 10 hours/day and subjects were required to wear their prescription every day. Contact lens wearers were also prescribed with multipurpose solutions, saline, and rewetting eye drops for contact lens maintenance. Results were analyzed using paired t-test with P <0.05 considered as significant.
Results
A total of 48 subjects were included in this study with ten males and 38 females. All subjects gave written informed consent and no payment was offered to subjects to volunteer to take part in the study. Mean age of subjects was 21.23±1.30 years and mean refraction was 2.17±1.10 DS. The demographic data for all subjects are shown in Table 1. The experimental subjects were age matched with the controls. Standard contact lens follow-up examination was performed and no adverse events due to contact lens wear were observed or reported during the period of this study. Mean room illumination during examination was 546.40±13.72 lux. Mean duration of contact lens wear was 10.5±1.5 hours per day. Mean refraction at baseline and 6 months for Group A was –2.16±0.97 DS and –2.05±1.03 DS and for Group B was –2.72±1.51 DS and –2.73±1.51 DS, respectively. Statistical analysis showed no significant difference in measurements at baseline (P=0.13) and at 6 months (P=0.08) between both groups.
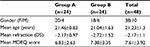  | Table 1 Demography of subjects Note: Group A, subjects wearing soft contact lenses; Group B, subjects wearing spectacles. Abbreviations: MDEQ, Mc Monnies Dry Eye Questionnaire; DS, Diopter sphere. |
The results of corneal morphology measurements are as follows.
Mean ECD (cell/mm2) at baseline and 6 months for Group A was 3104.19±237.30 and 3107.23±237.51 and for Group B was 3011.56±227.95 and 2983.83±244.55, respectively. Mean COV of cells (%) for Group A at baseline was 46.52±8.63 and at 6 months was 45.15±10.01. COV (%) for Group B at baseline and 6 months was 46.93±9.31 and 46.14±10.65, respectively.
Regarding hexagonality, mean HEX of cells (%) at baseline and 6 months for Group A was 46.65±10.12 and 45.13±10.01 and for Group B was 49.58±10.4 and 48.36±9.6, respectively. Mean central corneal thickness (CCT; µm) for Group A at baseline was 520.33±0.04 and at 6 months was 525.7±0.05, respectively. Mean CCT for Group B at baseline was 532±0.04 and at 6 months was 530±0.05, respectively.
Statistical analysis revealed no significant difference (P>0.05) in all parameters measured between both groups. Summary of measurements for both groups is presented in Table 2.
Discussion
This study examined the impact of wearing soft hydrogel contact lenses for 6 months on the morphology of corneal endothelial cells in young myopic adults living in Kuala Lumpur. The results of this study showed no significant difference in the corneal endothelial cell morphology between subjects wearing soft hydrogel contact lenses and spectacles. Generally, the subjects were comfortable wearing their soft contact lenses even though they did not have any prior experience of wearing them. The contact lens wearers were prescribed with multipurpose solutions and rewetting eye drops for maintenance and they complied with the instructions prescribed by the optometrists. There was no complaint or reported adverse events during the follow-up visits and their refractive error remained consistent through the study period.
There are many factors that can affect the morphology of corneal endothelial cells, and contact lens wear is the most frequently cited. Changes in the morphology of corneal endothelial cells in contact lens wearers have been attributed to chronic hypoxia due to extended wearing time.4 In this study, the short duration of wear (approximately 11 hours/day), good compliance, and high oxygen permeability contact lens material possibly prevented such changes from happening. The results are in agreement with earlier works8,15 that showed no significant difference in endothelial cell morphology between soft contact lens wearers and the controls. Conventional hydrogel contact lenses have been shown to induce changes in the morphology of corneal endothelium. Setälä et al16 investigated whether contact lens type and lens wearing time affect the morphology of corneal endothelial cells and found that longer wearing time of the contact lenses caused pleomorphism, polymegathism, and decrease in ECD. The authors concluded that extended wearing time of contact lenses is a factor that affected the morphology of corneal endothelial cells rather than lens types. Similar results were obtained by Lee et al6 who investigated the morphology of corneal endothelial cells in soft contact lens wearers with wearing time more than 5 years. The authors found that the ECD and HEX decreased while COV increased with duration of contact lens wear. However, it is now well known that extended-wear hydrogel soft contact lenses with low oxygen transmissibility are the main cause for corneal hypoxia, which subsequently leads to changes in corneal endothelial morphology. Development of newer generation of hydrogel lenses with higher water content that increases oxygen permeability but not to the level preventing significant overnight corneal swelling was proven to be clinically successful.17,18 Results by previous researchers have shown that hydrogel lenses with higher water content minimize hypoxic clinical signs in the majority of subjects who wore their lenses on a daily wear basis.17,18
In corneal endothelial morphology studies, ECD, COV, and HEX are the parameters measured to evaluate the changes in the cells. ECD is the parameter used to measure density of endothelial cells over specific area and the COV is a measurement of cell size variation that estimates the degree of polymegathism. The results of this study showed insignificant change in both ECD and COV at baseline and after 6 months of wearing hydrogel contact lenses. The ECD values are within the range of normal ECD found in normal population19 but lower than the reported values in local population within the same age group.20 It is possible that the discrepancy is probably due to the ethnicity of the subjects. The sample subjects used in this study were from mixed ethnicity, while in the previous study,20 the subjects were only from Malay ethnicity. With regard to COV, reported study on normal population showed higher COV (63.5% ± 23.2%) in the normal Malays in the same age group and ethnicity seemed to contribute to the COV, with the normal Malays having higher COV than the Chinese.20,21
With regard to percentage of HEX and CCT, the results of this study showed no significant difference before and after 6 months of contact lens wear. The results support earlier findings that showed no significant difference in HEX of silicone hydrogel contact lens wearers and non-contact-lens wearers.8 It is possible that due to high oxygen permeability of the hydrogel contact lens material (Dk = 19.6 × 10−11 (cm2/sec)mL O2/mL × mmHg), short duration of contact lens wear (approximately 11 hours daily) and good compliance no morphologic changes were observed after 6 months of wearing the contact lenses.
Conclusion
This study concludes that there is no significant change in the morphology of corneal endothelial cells after 6 months of wearing hydrogel contact lenses. This is probably due to high oxygen transmissibility of the contact lens material, short wearing duration, and good contact lens compliance.
Acknowledgment
This study was funded by UKM industrial research grant (2013–018).
Disclosure
The authors report no conflicts of interest in this work.
References
Sheng H, Bullimore MA. Factors affecting corneal endothelial morphology. Cornea. 2007;26(5):520–525. | ||
Bourne WM. The effect of long-term contact lens wear on the cells of the cornea. Clao J. 2001;27(4):225–230. | ||
Carlson KH, Bourne WM, Brubaker RF. Effect of long-term contact lens wear on corneal endothelial cell morphology and function. Invest Ophthalmol Vis Sci. 1999;76(10):712–719. | ||
Schoessler JP, Woloschack MJ. Corneal endothelium in veteran PMMA contact lens wearers. ICLC. 1981;8:19–25. | ||
Harvitt DM, Bonanno JA. Re-evaluation of the oxygen diffusion model for predicting minimum contact lens Dk/t values needed to avoid corneal anoxia. Optom Vis Sci. 1999;76(10):712–719. | ||
Lee JS, Park WS, Lee SH, Oum BS, Cho BM. A comparative study of corneal endothelial changes induced by different durations of soft contact lens wear. Graefes Arch Clin Exp Ophthalmol. 2001;239(1):1–4. | ||
Covey M, Sweeney DF, Terry R, Sankaridurg PR, Holden BA. Hypoxic effects on the anterior eye of high-Dk soft contact lens wearers are negligible. Optom Vis Sci. 2001;78(2):95–99. | ||
Mohidin N, Hoon NL, Ishak B, Mohd Ali B. Cornea endothelial cell morphology in short term silicone hydrogel soft contact lens wearers - Asian context. IJCRIMPH. 2014;6:296–302. | ||
Hamano H, Jacob JT, Senft CJ, et al. Differences in contact lens-induced responses in the corneas of Asian and non-Asian subjects. Clao J. 2002;28(2):101–104. | ||
Doughty MJ. A prospective analysis of corneal endothelial polymegethism and cell density in young adult Asians. Clin Exp Optom. 2014;97(3):256–263. | ||
McMonnies CW, Ho A. Responses to a dry eye questionnaire from a normal population. J Am Optom Assoc. 1987;58(7):588–591. | ||
Gothwal VK, Pesudovs K, Wright TA, McMonnies CW. McMonnies questionnaire: enhancing screening for dry eye syndromes with Rasch analysis. Invest Ophthalmol Vis Sci. 2010;51(3):1401–1407. | ||
Nichols JJ, Mitchell GL, Nichols KK, Chalmers R, Begley C, Lynn MAS. The performance of the contact lens dry eye questionnaire as a screening survey for contact lens-related dry eye. Cornea. 2002;21(5):469–475. | ||
Sheedy JE, Bailey IA, Raasch TW. Visual acuity and chart luminance. Optom Vis Sci. 1984;61(9):595–600. | ||
Yildiz Y, Gurdal C, Sarac O, Nacaroğlu SA, Takmaz T, Can I. The long term effects of silicone hydrogel contact lens wear on corneal morphology. Turk Oftal Dergisi. 2012;42:91–96. | ||
Setälä K, Vasara K, Vesti E, Ruusuvaara P. Effects of long-term contact lens wear on the corneal endothelium. Acta Ophthalmol Scand. 1998;76(3):299–303. | ||
Jones L. The use of high water content lenses on a daily wear basis. J Brit Contact Lens Assoc (Scientific Meeting). 1988:26–31. | ||
La Hood D. Daytime edema levels with plus powered low and high water content hydrogel contact lenses. Optom Vis Sci. 1991;68(11):877–880. | ||
Gutiérrez J, Ayala G, Dı́az ME. Set descriptors for visual evaluation of human corneal endothelia. Comput Vis Image Underst. 2001;84(2):249–263. | ||
Mohammad-Salih PA. Corneal endothelial cell density and morphology in normal Malay eyes. Med J Malaysia. 2011;66(4):300–303. | ||
Delshad S. Corneal Endothelial Cell Density in Young Malays and Chinese Adults [MHSc thesis]. Universiti Kebangsaan Malaysia; 2011. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.