Back to Journals » Risk Management and Healthcare Policy » Volume 13
Changes in Physical Activity and Sedentary Behavior Amid Confinement: The BKSQ-COVID-19 Project
Authors Alomari MA , Khabour OF , Alzoubi KH
Received 18 June 2020
Accepted for publication 14 August 2020
Published 25 September 2020 Volume 2020:13 Pages 1757—1764
DOI https://doi.org/10.2147/RMHP.S268320
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Marco Carotenuto
Mahmoud A Alomari,1 Omar F Khabour,2 Karem H Alzoubi3
1Department of Physical Education, Qatar University, Doha, Qatar; 2Department of Medical Laboratory Sciences, Jordan University of Science and Technology, Irbid, Jordan; 3Department of Clinical Pharmacy, Jordan University of Science and Technology, Irbid, Jordan
Correspondence: Mahmoud A Alomari Department of Physical Education
Qatar University, Doha, Qatar
Email [email protected]
Background: Coronavirus disease 19 (COVID-19) has compelled implementing confinement measure across the globe. These measures can potentially lead to many changes in lifestyle. However, no studies examined the effect of COVID-19-induced confinement on physical activity (PA) and sedentary behavior (SB).
Methods: During April and May of 2020, the current study surveyed changes in PA and SB induced by COVID-19 confinement.
Results: The participants of the study were 1844. Among the participants who were regularly involved in PA, the majority (41.8– 42.2%) of the participants reported a “decrease” (p< 0.05) in walking, jogging, and sports while the majority (46.3– 53.1%) reported a “no change” (p< 0.05) in swimming, cycling, and weight lifting. With regard to the SB, most of the participants reported an “increase” in watching TV (72.3%), using electronics (82.7%), and logging to social media (81.9%). Additionally, gender, job type, obesity, and being worried to contract the disease were associated (p< 0.05) with changes in PA. On the other hand, age, gender, obesity, job type and income were related (p< 0.05) to changes in SB.
Conclusion: Results of the current study might enhance knowledge about the impact of COVID-19 on lifestyle, particularly PA and SB. Subsequently, it can also be used to establish strategies to enhance engagement in activities during the current and future pandemics.
Keywords: physical activity, sedentary behavior, confinement, COVID-19, pandemic
Introduction
Coronavirus disease 19 (COVID-19) started in China, Wuhan in November of 2019 and was declared as a fatal pandemic by the WHO in March, 2020.1,2 According to WHO data, millions of COVID-19 cases leading to hundreds of thousands fatalities have been documented worldwide, as of June of 2020.
The COVID-19 is a highly pathogenic single-stranded RNA virus that belongs to the genus Beta coronavirus.3–6 Human-to-human transmission of the COVID-19 is usually via direct contact and is higher among individuals in one household.7,8 Commonly reported symptoms included cough, fever, breathing difficulty, sore throat, headache, vomiting and diarrhea.9 Though is experienced less frequently, the most potent effect of the virus is attacking the respiratory track cells via its envelope proteins.10,11 Subsequently, some patients develop acute respiratory failure and sepsis, which are considered the major complications of the disease.12,13
As a response to the spread and devastating effect of the virus, several actions have been taken. These actions include suspension of schools, banning public gatherings, closure of the borders, airports, businesses, and worship places, and restriction of local travel. Such actions have been implemented across the globe with slight differences between countries. Subsequently, people spend most of their time at home, which is expected to impact most aspects of their routine lifestyle such as physical activity (PA) and sedentary behavior (SB). A recent study among adults in the UK showed limited physical activity experienced during the application of COVID-19 related social distancing measures.14 Another study from Brazil showed reduced moderate to vigorous physical activity and increased SB during the application of COVID-19 related social distancing measures.15
Such changes in lifestyle during the COVID-19 crisis might have long-term effects on health, subsequently the body response to infections. In a review, exercise has been shown to ameliorate the response of the body to respiratory tract viral infections. The review concluded that moderate-intensity PA enhances immune function and reduces the risk and severity of respiratory viral infections. Exercise seems to elevate stress hormones, subsequently enhance the Th2 immune response pathway.16 Another review reported that engaging in moderate PA may enhance the immune function, especially in less fit subjects/sedentary population. On the other hand, intense exercise may cause immunosuppression and increases the risk of respiratory viral infection.17 Thus, changes in lifestyles during COVID-19 crisis, especially PA and SB might have health consequences on the response of the body to respiratory tract infections. Therefore, in the current investigation, changes in PA and SB during COVID-19 crisis were investigated. The results of this study might enhance current knowledge about the impact of COVID-19 on lifestyle, particularly PA and SB. Subsequently, highlights the needs for interventions to prepare for the negative effects of the current and possible future calamities.
Methods
Design and Participants
The current data is derived from a larger project, the “Behavior, Knowledge, Stress and Quality of Life during COVID19-induced Confinement (BKSQ-COVID19) project”. The study is a cross-sectional survey distributed during April and May of 2020 to examine changes in PA and SB. Jordanian adults (age >18 years) of both genders from most parts of Jordan were invited to participate in the study. The questionnaire was distributed anonymously and electronically via social media platforms. Participants were informed about the objectives of the study and consented electronically prior to filling the questionnaire. Institutional Review Board (IRB) of Jordan University of Science and Technology approved the study procedures.
Questionnaire
Given the novelty of the disease, no previous questionnaires were appropriate enough to fit the objectives of the study. Thus, the research team developed the questionnaire based on similar studies.18 The questionnaire covers domains including demographics, perceptions about COVID-19 disease, and changes in PA and SB during the pandemics. Demographic parameters included age, gender, weight, height, job type (ie educational, medical, versus managerial), education, and income. Additionally, COVID-19 perception and confinement information, such as the likelihood of getting infected, knowing somebody infected with COVID-19, and the implemented governmental confinement procedures, were surveyed.
The examined PA measures were walking, jogging, swimming, sporting, weight lifting, while watching TV, using electronics, and logging to social media were considered SB. The participants were asked “What changes have you experienced in the following lifestyle behaviors due to the spread of coronavirus?”. Four choices were available, “increase”, “decrease”, “no change”, and “never practiced this behavior”.
Statistics
The SPSS (version 21) was used to statistically analyze the data. For statistical significance, α was set a priori at 0.05. The data are presented in mean±SD, frequency and percentages. The Chi2 goodness of fit test was used to determine the differences in the distribution of the participant responses, “increase”, “decrease”, versus “no-change” in PAs and SBs. Cross-tabulation was used to determine the relationship of potential factors with the participant responses to the questions about the changes in PAs and SBs, “increase”, “decrease”, or “no-change”. The factors found, using cross-tabulation, related to the responses to each question were incorporated into a multinomial model to determine the ability of each factor to predict the responses. The potential factors were age, gender, obesity (BMI classifications), income, education, job type, worried to be infected COVID-19, and knowing a person infected with COVID-19.
Results
Participants
The participants’ characteristics are presented in Table 1. A total of 1844 individuals responded to the questionnaire. Age, weight, and height ranges were 18–72 years, 38–144 kg, and 120–198 cm. Most of the participants were women, with a bachelor's degree, receiving middle income, who are unemployed while more than 50% were either overweight, obese or severely obese. As in Table 2, very few participants were worried about getting infected or knew a person who was infected. Additionally, the majority of the participants reported a range of confinement practices and advisories, including self-quarantine, social distancing, lockdown, school closure, and event banning.
 |
Table 1 The Participant Demographic (n=1844) |
 |
Table 2 Perception and Confinement Information Related to COVID-19 (n=1844) |
Prevalence of Physical Activities and Sedentary Behaviors
As in Table 3, the majority of the participants reported no involvement in PA including cycling (71.4%), swimming (65.2%), sports (56.4%), and weight lifting (68.2%). Additionally, most of the subjects were involved in all the surveyed SB including watching TV (94.6%), using electronics (97.6%), and logging to social media (99.2%).
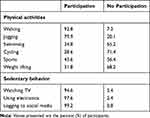 |
Table 3 Prevalence of Physical Activities and Sedentary Behavior |
Changes in Physical and Sedentary Activities
The chi-square goodness-of-fit test demonstrates differences (p<0.05) between the participants’ responses to the questions about participating in PAs and SBs, “increase”, “decrease”, versus “no-change”. Table 4 shows that among the participants who were regularly involved in PA, the majority of the participants reported a decrease in walking, jogging, and sports while the majority reported a no change in swimming, cycling, and weight lifting. With regard to the SB, most of the participants reported an increase in watching TV (72.3%), using electronics (82.7%), and logging to social media (81.9%).
 |
Table 4 Changes in Physical Activities and Sedentary Behavior |
Factors Contributing to the Changes in Physical Activities
Cross-tabulation tests were used to examine the relationship of PA measures with potential contributing factors. Values are expressed as percentage. Walking was related to gender (χ2=7.3; p=0.026) and job type (χ2=38.7; p=0.001) while jogging was related to age (χ2=19.0; p=0.001) and job type (χ2=30.7; p=0.015). The cross-tabulation also revealed that cycling was related to age (χ2=19.9; p=0.001) while swimming was related to age (χ2=11.8; p=0.02) and obesity (χ2=15.9; p=0.04). Additionally, the analysis showed a relationship of sports with age (χ2=14.0; p=0.007) and gender (χ2=25.9; p=0.0001) as well as an association of weight lifting with age (χ2=20.8; p=0.0001) and obesity (χ2=17.9; p=0.02).
Factors Contributing to the Changes in Sedentary Behaviors
The cross-tabulation revealed a relationship between TV watching time and age (χ2=13.8; p=0.008), gender (χ2=9.1; p=0.01), obesity (χ2=19.9; p=0.01), and income (χ2=15.7; p=0.003). The cross-tabulation showed that electronic use was related to education (χ2=15.6; p=0.016), income (χ2=16.5; p=0.014), and job type (χ2=46.9; p=0.0001).
Predictors of the Changes in Physical Activities
The factors that were found related to each perspective PA parameter using cross-tabulation, were added to the regression model. Additionally, the “no change” choice was used as the reference for all PA variables in the regression model. The regression showed that the combination of gender and job type can predict participating in walking (χ2= 40.8; p<0.002; NagR2=0.03). However, further analysis showed that only job type contributes meaningfully to the model (χ2= 36.0; p=0.003). The participants holding a job in the military (β=−1.0; OR=0.35; p=0.035), agriculture (β=−1.4; OR=0.25; p=0.024), health (β=−1.1; OR=0.31; p=0.006), and engineering (β=−1.1; OR=0.34; p=0.02), versus a job in crafting, were less likely to select an “increase” in walking versus “no change”.
The regression showed that the combination of age and job type can predict participating in jogging (χ2=29.0; p<0.0001; NagR2=0.04). Additional analysis revealed that age (χ2= 16.7; p=0.002) and job type (χ2= 30.0; p=0.02) can each contribute uniquely to the model. The younger individuals, versus the elderly, were more likely to select a “decrease” (β=0.6; OR=1.8; p=0.007) and an “increase” (β=0.5; OR=2.4; p=0.02) in jogging versus a “no-change”. The regression showed that age can predict participating in cycling (χ2=19.5; p<0.001; NagR2=0.45). Further analysis, however, showed that age can contribute uniquely to the model with middle age, comparing to elderly, more likely to select a “decrease” (β=0.6; OR=2.0; p=0.05) in cycling versus a “no-change”.
The regression showed that the combination of age and obesity can predict participating in swimming (χ2=22.6; p<0.03; NagR2=0.05). Further analysis, however, showed that neither age (χ2=6.5; p>0.16) nor obesity (χ2=10.0; p>0.26) can uniquely contribute to the model. The regression showed that the combination of age and gender can predict participating in sports (χ2=42.4; p<0.0001; NagR2=0.06). Further analysis showed that age (χ2=13.9; p=0.007) and gender (χ2=28.9; p=0.0001) can each contribute uniquely to the model. Being younger (β=0.7; OR=2.0; p=0.007), versus elderly, while men (β=0.4; OR=1.5; p=0.017) versus women, is more likely to select a “decrease” while being a man (β=−0.7; OR=0.5; p=0.001), versus being a woman, is less likely to select an “increase” in sport participation.
The regression showed that the combination of age and obesity can predict (χ2= 26.6; p<0.0001; NagR2=0.07) participating in weight lifting. Further analysis, however, showed that only age (χ2= 15.5; p=0.004) can contribute uniquely to the model. Being younger (β=0.7; OR=2.0; p=0.05), versus elderly is more likely, while being obese (β=−1.1; OR=0.3; p=0.04), versus overly obese, is less likely to select a “decrease” in weightlifting.
Predictors of the Changes in Sedentary Behavior
The factors were found related to each perspective SB parameter using cross-tabulation, were added to the regression model. Additionally, the “no change” choice was used as the reference for all SB variables in the regression model. The regression showed that the combination of age, gender, obesity, and income can predict participating in TV watching time (χ2= 55.8; p<0.0001; NagR2=0.044). Additional analysis showed that age (χ2= 13.0; p=0.01), obesity (χ2= 21.0; p=0.007), and income (χ2= 15.7; p=0.003) can each contribute uniquely to the model. Being younger (β=0.6; OR=0.2; p=0.02), versus older, is more likely, while being normal (β=−1.3; OR=0.3; p=0.007) and over (β=−1.5; OR=0.2; p=0.003) weight, versus overly obese, was less likely to select a “decrease” in TV watching time. Additionally, being a man (β=0.3; OR=1.3; p=0.04), versus a woman, was more likely to select an “increase” in TV watching time. The regression showed that the combination of education, income, and job type can predict participating in electronic use (χ2= 62.9; p<0.0001; NagR2=0.06). Additional analysis showed that only job type (χ2= 41.8; p=0.0001) can contribute uniquely to the model.
Discussion
The study examined the changes in PAs and SBs during the COVID-19-induced confinement. The results showed that the majority (41.8–42.2%) of the participants reported a decrease in walking, jogging, and sports while the majority (46.3–53.1%) reported a no change in swimming, cycling, and weight lifting. Conversely, the majority (72.1–82.7%) of the participants reported an “increase” in all of SBs. Subsequent analysis indicates that walking was related to gender and job type and jogging was related to age and job type while cycling was related to age and swimming was related to age and obesity. Sport was related to age and gender while weightlifting was related to age, obesity, and being worried to conduct the disease. Watching TV was related to age, gender, obesity and income while using electronics was related to the job type. Given the lack of studies, the present study provides unique information to understand the changes in PAs and SBs during COVID-19. The results can be used to establish strategies to enhance engagement in activities during the current and future pandemics.
Confinement is often experienced under few settings, prison, Antarctic camps, and space trips. The data from these settings have suggested a range of psychological and physiological symptoms. Among these symptoms are cognitive, neural, and hormonal alterations, lethargy, skewed circadian rhythm, sleeping difficulties, and diminished immune regulations.19–21 In fact, some studies have found a relationship between confinement and death after release from prison.22 Mental health was also shown to be negatively impacted by COVID-19-related confinement leading to increased stress anxiety and depression symptoms.23–26 Studies have shown that lockdown is a great stress for citizens; thus, the characteristics of exercise selection may be affected by such a stress. A previous review has concluded a differential impact for stress on exercise adoption, maintenance, and relapse, where habitually active individuals exercise more in the face of stress, and those in beginning stages exercise less.27 In a study from Italy, the lockdown was also shown to adversely impact dietary habits leading to increased consumption of “comfort food” such as chocolate, ice-cream, and desserts, and salty snacks.28
Since the COVID-19 breakout, several reports have cautioned of the possible decrease in PA,29–33 increase in SB,34 and subsequent adverse health effects during COVID-19-induced confinement.34 As far as the author's knowledge, one study reported 36.9%, 34.7%, 42.7%, and 38% decrease in vigorous, moderate, walking, and total PA METs, respectively, while SB increased by 5–8 hours/daily.35 A recent study from Brazil showed reduced moderate to vigorous physical activity and increased SB during the application of COVID-19 related social distancing measures.15 Similarly, a large portion of the current sample reported a decrease in PA and an increase in SB. These results are alarming and might be associated with adverse health effects. These studies have suggested the possibilities of increased risk of cardiovascular,33,34 metabolic,34,36 neural,34 and muscular34 disease symptoms. Additionally, results from inactivity models including bed rest, limb suspension, and step-reduction have demonstrated rapid muscle wasting, fiber denervation, neuromuscular junction damage, suppressed protein synthesis, and augmented protein degradation.34,37 Reduced PA and increased SB may also impact the metabolic system, including glucose homeostasis and diminished insulin sensitivity. Impaired cardiovascular endurance, subsequent to diminished cardiac and vascular functions and muscular oxidative capacity, has also been reported. Physical inactivity has also been implicated in the positive energy balance and subsequent fat deposition and weight gains.34 Fortunately, these negative adverse effects can be ameliorated by regular participation in PA.38
The benefits of regular PA are undeniable and unlimited. It decreases the risk, hospitalization, morbidity, and mortality of many noncommunicable diseases. These include diseases of the cardiovascular, metabolic, immune, neural, and hormonal systems. Additionally, it is an essential component of strategies to enhance weight loss and maintenance, mental health, quality of life, and well-being.38 More recently, some research is arguing the environmental benefits of PA including generating extra returns of investments, lowering fossil fuel dependence, and less congested and safer roads, and cleaner air, which are shared goals of the ambitious global 2030 Sustainable Development Agenda.39
The measured parameter of PA, including walking, jogging, cycling, swimming, sports, and weight lifting, decreased. Additionally, parameters of SB, including time spent watching TV, using social media and electronics, increased among the majority of the participants. According to the results, age, gender, income, occupation, obesity, and being worried about conducting COVID-19 seem to predict the changes in PA and SB participation. Given the novelty of the disease and the sparsity of information, it is difficult to explain the current results. Previous studies have suggested cultural,40 psychological,41 behavioral,42 biological,43 environmental,44 economic,45 and policy46 detriments of participating in PA. The importance of these factors seems to vary across social segments, age, gender, location and education.40–46 Therefore, more studies are needed to verify the current findings under confinement situations, especially due to infectious diseases. Subsequently, design studies and strategies to improve exercise adherence among adults during disease-induced confinement.
Implications
As previously has been anticipated,29–34 PA decreased, whereas SB increased among the participants in the current study during confinement due to COVID-19. The ramifications of these changes remained to be unraveled. However, the adverse health effects of decreased PA and increased SB are well documented.29–34 Therefore, strategies are needed to help people staying active and to mitigate the possible adverse health effect during the current and future pandemics.
Limitations
The design of the current study is cross-sectional, which makes concluding a cause-effect relationships difficult. The measures of PAs and SBs are crude without details of the intensity, duration, frequency, progression, and METs. Additionally, the inherited misinformation in self-reported survey research is a disadvantage of the current study. Furthermore, the study participants are from Jordan, which confines the generalizability of the results in other communities, countries, and ethnicities. Therefore, future interventions and longitudinal studies in different regions of the world using objective measures of PAs and SBs are warranted to better understand the effect of confinement during the current and future pandemics.
Conclusions
The current study revealed a 35.9–44.5% decrease in the different modes of PAs and a 72.1–82.7% increase in the various SB measures. Additionally, age, gender, income, occupation, obesity, and being worried about conducting COVID-19 are associated with the changes in PA and SB. However, studies are needed to verify the current findings and strategies are warranted to encourage people staying active and to mitigate the adverse health effects of inactivity due to confinement during the current and future pandemics.
Acknowledgment
Open Access funding provided by the Qatar National Library. The project was supported by the Deanship of Research at Jordan University of Science and Technology, Irbid, Jordan (Grant number: 245/2020).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Peeri NC, Shrestha N, Rahman MS, et al. The SARS, MERS and novel coronavirus (COVID-19) epidemics, the newest and biggest global health threats: what lessons have we learned? Int J Epidemiol. 2020;49(3):717–726. doi:10.1093/ije/dyaa033
2. Rothan HA, Byrareddy SN. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J Autoimmun. 2020;109:102433. doi:10.1016/j.jaut.2020.102433
3. Bai Y, Yao L, Wei T, et al. Presumed asymptomatic carrier transmission of COVID-19. JAMA. 2020;323(14):1406. doi:10.1001/jama.2020.2565
4. Zhou M, Zhang X, Qu J. Coronavirus disease 2019 (COVID-19): a clinical update. Front Med. 2020;14(2):126–135. doi:10.1007/s11684-020-0767-8
5. Elfiky AA. Ribavirin, remdesivir, sofosbuvir, galidesivir, and tenofovir against SARS-CoV-2 RNA dependent RNA polymerase (RdRp): a molecular docking study. Life Sci. 2020;253:117592. doi:10.1016/j.lfs.2020.117592
6. Joynt GM, Wu WK. Understanding COVID-19: what does viral RNA load really mean? Lancet Infect Dis. 2020;20(6):635–636. doi:10.1016/S1473-3099(20)30237-1
7. Bai Z, Gong Y, Tian X, Cao Y, Liu W, Li J. The rapid assessment and early warning models for COVID-19. Virol Sin. 2020;35(3):272–279. doi:10.1007/s12250-020-00219-0
8. Calton B, Abedini N, Fratkin M. Telemedicine in the time of coronavirus. J Pain Symptom Manage. 2020;60(1):e12–e14. doi:10.1016/j.jpainsymman.2020.03.019
9. Liu N, Zhang F, Wei C, et al. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: gender differences matter. Psychiatry Res. 2020;287:112921. doi:10.1016/j.psychres.2020.112921
10. Luan J, Jin X, Lu Y, Zhang L. SARS-CoV-2 spike protein favors ACE2 from Bovidae and Cricetidae. J Med Virol. 2020;92(9):1649–1656. doi:10.1002/jmv.25817
11. Zhang C, Wu Z, Li JW, Zhao H, Wang GQ. The cytokine release syndrome (CRS) of severe COVID-19 and Interleukin-6 receptor (IL-6R) antagonist Tocilizumab may be the key to reduce the mortality. Int J Antimicrob Agents. 2020;55(5):105954. doi:10.1016/j.ijantimicag.2020.105954
12. Gane SB, Kelly C, Hopkins C. Isolated sudden onset anosmia in COVID-19 infection. A novel syndrome? Rhinology. 2020;58(3):299–301. doi:10.4193/Rhin20.114
13. Verity R, Okell LC, Dorigatti I, et al. Estimates of the severity of coronavirus disease 2019: a model-based analysis. Lancet Infect Dis. 2020;20(6):669–677. doi:10.1016/S1473-3099(20)30243-7
14. Smith L, Jacob L, Butler L, et al. Prevalence and correlates of physical activity in a sample of UK adults observing social distancing during the COVID-19 pandemic. BMJ Open Sport Exerc Med. 2020;6(1):e000850. doi:10.1136/bmjsem-2020-000850
15. Schuch F, Bulzing R, Meyer J, et al. Moderate to vigorous physical activity and sedentary behavior change in self-isolating adults during the COVID-19 pandemic in Brazil: A cross-sectional survey exploring correlates. 2020.
16. Martin SA, Pence BD, Woods JA. Exercise and respiratory tract viral infections. Exerc Sport Sci Rev. 2009;37(4):157. doi:10.1097/JES.0b013e3181b7b57b
17. Romeo J, Warnberg J, Pozo T, Marcos A. Role of physical activity on immune function. Proc Nutri Soc. 2010;69(3):390–399. doi:10.1017/S0029665110001795
18. Alomari MA, Shqair DM, Khabour OF, Alawneh K, Nazzal MI, Keewan EF. The clinical and nonclinical values of nonexercise estimation of cardiovascular endurance in young asymptomatic individuals. ScientificWorldJournal. 2012;2012:958752. doi:10.1100/2012/958752
19. Hagan BO, Wang EA, Aminawung JA, et al. History of solitary confinement is associated with post-traumatic stress disorder symptoms among individuals recently released from prison. J Urban Health. 2018;95(2):141–148. doi:10.1007/s11524-017-0138-1
20. Hodkinson PD, Anderton RA, Posselt BN, Fong KJ. An overview of space medicine. Br J Anaesth. 2017;119(suppl_1):i143–i153. doi:10.1093/bja/aex336
21. Pagel JI, Chouker A. Effects of isolation and confinement on humans-implications for manned space explorations. J Appl Physiol (1985). 2016;120(12):1449–1457. doi:10.1152/japplphysiol.00928.2015
22. Brinkley-Rubinstein L, Johnson T. Solitary Confinement and Health. N C Med J. 2019;80(6):359–360. doi:10.18043/ncm.80.6.359
23. Rossi R, Socci V, Talevi D, et al. COVID-19 Pandemic and Lockdown Measures Impact on Mental Health Among the General Population in Italy. An N=18147 Web-Based Survey. 2020.
24. Meyer J, McDowell C, Lansing J, et al. Changes in Physical Activity and Sedentary Behaviour Due to the COVID-19 Outbreak and Associations with Mental Health in 3,052 US Adults. 2020.
25. Schuch FB, Bulzing RA, Meyer J, et al. Associations of moderate to vigorous physical activity and sedentary behavior with depressive and anxiety symptoms in self-isolating people during the COVID-19 pandemic: a cross-sectional survey in Brazil. Psychiatry Res. 2020;292:113339. doi:10.1016/j.psychres.2020.113339
26. Stanton R, To Q, Khalesi S, et al. Depression, anxiety and stress during COVID-19: associations with changes in physical activity, sleep, tobacco and alcohol use in australian adults. Int J Environ Res Public Health. 2020;17:4065. doi:10.3390/ijerph17114065
27. Stults-Kolehmainen MA, Sinha R. The effects of stress on physical activity and exercise. Sports Med (Auckland, NZ). 2014;44(1):81–121.
28. Scarmozzino F, Visioli F. Covid-19 and the subsequent lockdown modified dietary habits of almost half the population in an italian sample. Foods. 2020;9:5. doi:10.3390/foods9050675
29. Chen P, Mao L, Nassis GP, Harmer P, Ainsworth BE, Li F. Coronavirus disease (COVID-19): the need to maintain regular physical activity while taking precautions. J Sport Health Sci. 2020;9(2):103–104. doi:10.1016/j.jshs.2020.02.001
30. Rahmati-Ahmadabad S, Hosseini F. Exercise against SARS-CoV-2 (COVID-19): does workout intensity matter? (A mini review of some indirect evidence related to obesity). Obesity Med. 2020;19:100245. doi:10.1016/j.obmed.2020.100245
31. Jurak G, Morrison SA, Leskosek B, et al. Physical activity recommendations during the coronavirus disease-2019 virus outbreak. J Sport Health Sci. 2020;9(4):325–327. doi:10.1016/j.jshs.2020.05.003
32. Carter SJ, Baranauskas MN, Fly AD. Considerations for obesity, Vitamin D, and physical activity amid the COVID-19 Pandemic. Obesity (Silver Spring). 2020;28(7):1176–1177. doi:10.1002/oby.22838
33. Pecanha T, Goessler KF, Roschel H, Gualano B. Social isolation during the COVID-19 pandemic can increase physical inactivity and the global burden of cardiovascular disease. Am J Physiol Heart Circ Physiol. 2020;318(6):H1441–H1446. doi:10.1152/ajpheart.00268.2020
34. Narici M, De Vito G, Franchi M. et al. Impact of sedentarism due to the COVID-19 home confinement on neuromuscular, cardiovascular and metabolic health: physiological and pathophysiological implications and recommendations for physical and nutritional countermeasures. Eur J Sport Sci;2020. 1–22. doi:10.1080/17461391.2020.1761076
35. Ammar A, Brach M, Trabelsi K, et al. Effects of COVID-19 home confinement on eating behaviour and physical activity: results of the ECLB-COVID19 International Online Survey. Nutrients. 2020;12(6):6. doi:10.3390/nu12061583
36. Bhutani S, Cooper JA. COVID-19 related home confinement in adults: weight gain risks and opportunities. Obesity (Silver Spring). 2020. doi:10.1002/oby.22904
37. Sarto F, Impellizzeri FM, Sporri J, et al. Impact of potential physiological changes due to COVID-19 Home Confinement on Athlete Health Protection in Elite Sports: a call for awareness in sports programming. Sports Med. 2020;50(8):1417–1419. doi:10.1007/s40279-020-01297-6
38. Garber CE, Blissmer B, Deschenes MR, et al. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43(7):1334–1359. doi:10.1249/MSS.0b013e318213fefb
39. Terama E, Milligan B, Jimenez-Aybar R, Mace GM, Ekins P. Accounting for the environment as an economic asset: global progress and realizing the 2030 Agenda for Sustainable Development. Sustainability Sci. 2016;11(6):945–950. doi:10.1007/s11625-015-0350-4
40. Jaeschke L, Steinbrecher A, Luzak A, et al. Socio-cultural determinants of physical activity across the life course: a ‘Determinants of Diet and Physical Activity’ (DEDIPAC) umbrella systematic literature review. Int J Behav Nutr Phys Act. 2017;14(1):173. doi:10.1186/s12966-017-0627-3
41. Cortis C, Puggina A, Pesce C, et al. Psychological determinants of physical activity across the life course: a “DEterminants of DIet and Physical ACtivity” (DEDIPAC) umbrella systematic literature review. PLoS One. 2017;12(8):e0182709. doi:10.1371/journal.pone.0182709
42. Condello G, Puggina A, Aleksovska K, et al. Behavioral determinants of physical activity across the life course: a “Determinants of diet and physical activity” (DEDIPAC) umbrella systematic literature review. Int J Behav Nutr Phys Act. 2017;14(1):58. doi:10.1186/s12966-017-0510-2
43. Aleksovska K, Puggina A, Giraldi L, et al. Biological determinants of physical activity across the life course: a “Determinants of Diet and Physical Activity” (DEDIPAC) umbrella systematic literature review. Sports Med. 2019;5(1):2. doi:10.1186/s40798-018-0173-9
44. Carlin A, Perchoux C, Puggina A, et al. A life course examination of the physical environmental determinants of physical activity behaviour: a “Determinants of Diet and Physical Activity” (DEDIPAC) umbrella systematic literature review. PLoS One. 2017;12(8):e0182083. doi:10.1371/journal.pone.0182083
45. O’Donoghue G, Kennedy A, Puggina A, et al. Socio-economic determinants of physical activity across the life course: a “DEterminants of DIet and Physical ACtivity” (DEDIPAC) umbrella literature review. PLoS One. 2018;13(1):e0190737. doi:10.1371/journal.pone.0190737
46. Puggina A, Aleksovska K, Buck C, et al. Policy determinants of physical activity across the life course: a ‘DEDIPAC’ umbrella systematic literature review. Eur J Public Health. 2018;28(1):105–118. doi:10.1093/eurpub/ckx174
 © 2020 The Author(s). This work is published by Dove Medical Press Limited, and licensed under a Creative Commons Attribution License.
The full terms of the License are available at http://creativecommons.org/licenses/by/4.0/.
The license permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
© 2020 The Author(s). This work is published by Dove Medical Press Limited, and licensed under a Creative Commons Attribution License.
The full terms of the License are available at http://creativecommons.org/licenses/by/4.0/.
The license permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
