Back to Journals » Clinical Ophthalmology » Volume 17
Causes of Moderate to Severe Visual Impairment and Blindness Among Children in Integrated Schools for the Blind and Visiting a Tertiary Eye Hospital in Nepal: The Nepal Pediatric Visual Impairment (NPVI) Study
Authors Adhikari S , van Nispen RMA, Elsman EBM, van Rens F, van Rens G
Received 3 November 2022
Accepted for publication 12 January 2023
Published 3 April 2023 Volume 2023:17 Pages 1025—1034
DOI https://doi.org/10.2147/OPTH.S394890
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Srijana Adhikari,1 Ruth Marie Antoinette van Nispen,2 Ellen Bernadette Maria Elsman,2 Fleur van Rens,3 Ger van Rens2
1Department of Pediatric Ophthalmology and Strabismus, Tilganga Institute of Ophthalmology, Kathmandu, Nepal; 2Department of Ophthalmology, VU University Medical Centre and the Amsterdam Public Health Research Institute, Amsterdam, the Netherlands; 3Discipline of Exercise Science, Murdoch University, Murdoch, WA, Australia
Correspondence: Srijana Adhikari, Tilganga Institute of Ophthalmology, Gaushala, PO Box 561, Kathmandu, Nepal, Tel +977-9849287387, Email [email protected]
Purpose: To study the causes of moderate and severe visual impairment (VI) and blindness and its changing trends in Nepalese children.
Patients and Methods: A cross-sectional descriptive study was conducted. Participants, aged 7 to 17 years were recruited from integrated schools for the blind and the outpatient department of a tertiary eye hospital in Kathmandu. VI and blindness were categorized according to World Health Organization (WHO) categories and its protocol for eye examination of children with blindness and VI was followed. Findings were compared to former studies from Nepal.
Results: A total of 200 children were included, of whom 45% had moderate VI, 5% had severe VI, and 50% were blind. Mean age of children with VI and blindness was 11.1 (SD = 3.3) and 12.9 (SD = 3) years, respectively. Forty percent of children with VI and 38% of blind children were female. In our study, retina (39%) and whole globe (32%) were the most common anatomical site of involvement in children with VI and blindness, respectively, while cornea was the most common anatomical site of involvement in former studies. Heredity (43%) was the most common etiological factor although in 24.5% of all children, etiology was unknown. In 43.5% of children, blindness and VI was due to avoidable causes.
Conclusion: In relatively many children, the etiology of VI and blindness could be either prevented or treated. Compared to former studies from Nepal, there is a changing trend in the etiology of severe VI and blindness.
Keywords: childhood blindness, Nepal, visual impairment, pediatric
A Letter to the Editor has been published for this article.
A Response to Letter by Mr Singh has been published for this article.
Introduction
Blindness and visual impairment (VI) are among the leading causes of disabilities in children.1 For this reason, childhood blindness is considered a priority disease by the World Health Organization (WHO).2 The number of years a person lives with a visual disability poses a socioeconomic burden not only for the individual person but also for the family, society and the country as a whole. Most causes of childhood visual disabilities in low-income countries are either preventable or treatable.3 Moreover, childhood blindness is closely linked with child survival as many of the causes of blindness in children also cause mortality such as measles, vitamin A deficiency, retinopathy of prematurity, etc.4 The prevalence of blindness in children around the globe ranges from 0.3/1000 children in high-income countries to 1.5/1000 children in the least developed countries.5 Similarly, the etiology also varies from region to region with cerebral visual impairment, retinopathy of prematurity and retinal dystrophy being the leading causes of blindness in the developed world, while vitamin A deficiency, measles and uncorrected refractive errors being the leading causes in the developing world.6,7 Given these geographical differences, it is important to investigate the national prevalence and etiology of childhood VI and blindness so that local policies and programs for prevention and treatment can be developed and implemented. Also, it is useful to repeat the studies every five to ten years to see the changing trends in etiology and prevalence and to adapt healthcare policy if needed.8
There are several ways in which the prevalence and etiology of childhood VI and blindness can be studied. In high-income countries, the availability of registries as well as large-scale vision screening programs provides an important source of data.9,10 In low- and middle-income countries, community-based rehabilitation programs are important to study childhood VI. If these are not available proxy data from under-five mortality rate and key informant method with people who know what is going on in certain communities are potentially important tools to study the prevalence of childhood VI and blindness.11,12 Conducting population-based studies can be challenging because of the substantial costs and manpower required, as well as geographical challenges that may be present. Collecting data from schools for the blind or using hospital-based data on VI is one of the alternative methods to investigate the prevalence and etiology of childhood VI and blindness despite the fact that the information from this source may under represent the whole population. However, there are studies conducted in hospitals and in special schools which give information on etiology and changing trends of VI and blindness in several countries.13–18
Between 2008 and 2017, childhood VI and blindness have been investigated in several studies in Nepal.19–24 Kansakar et al and Shrestha et al conducted studies in integrated schools for the blind.19,20 They found that corneal diseases were the leading cause of childhood VI and blindness in Nepal. Similarly, large population-based studies identified childhood ocular morbidity and blindness in several parts of the country. These studies found the prevalence of childhood blindness ranged between 0.03% and 0.06% with amblyopia being the leading cause of blindness.22,23 Similarly, these studies have found the prevalence of low vision ranging from 0.1% to 0.5% with refractive error and retinal diseases being the leading causes. However, these studies were conducted some ten years back. In the last decade, an effective nutritional program has been introduced by the Nepali government. Further, eyecare is increasingly accessible and awareness of eye diseases in the country is growing. Therefore, the aim of the current study is to explore both the etiology and its changing trends compared to previous studies19–21,24 in childhood VI and blindness in Nepalese school-aged children attending integrated schools for the blind as well as visiting a tertiary referral hospital in Kathmandu.
Materials and Methods
Design and Ethics
This cross-sectional descriptive study is a part of the Nepal Pediatric Visual Impairment Study (NPVI). In this study, we aim to investigate causes of childhood VI and blindness, the children’s level of participation, physical activity and quality of life. A literature review was conducted to compare our data to findings from previous Nepali studies. The literature search was carried out in PubMed with the topic” Childhood blindness and VI in Nepal”. All previous studies from Nepal within the same age group hospital and blind school settings were selected for comparison. Population-based studies were excluded.
The study was approved by the Ethical review board of the Tilganga Institute of Ophthalmology (TIO) and the Nepal Health Research Council (NHRC). The proposal id is 239–2020. The study adhered to the tenants of declaration of Helsinki. Prior to the study commencement, informed consent was obtained from the parents or care-givers of the children, and ascent was provided by the children themselves.
Participants
Schoolchildren aged 7 to 17 years were included in the study. We used this age group according to the UN conventions on the right of the child25 Data collection was done from April 2021 to March 2022. The first recruitment approach included blind children who were studying in integrated schools for the blind. These children were examined in their respective schools located in the Kathmandu, Bhaktapur and Lalitpur districts in the Kathmandu valley. The second recruitment approach included children with VI who were examined as outpatients in TIO who met the criteria for participation in this study. This included children aged 7 to 17 years with VI according to WHO criteria of VI and blindness.26 Participant recruitment was stopped once 100 participants were included from each recruitment approach. Children who refused to give consent and those with cognitive disorders were excluded from the study. We used convenience sampling for selecting the schools and purposive sampling for collecting data.
Procedure
Detailed medical history and demographic information were collected via parents, guardians or school teachers. Medical history included antenatal and perinatal history, systemic illness, family history of illness, and treatment history. The examination team consisted of a pediatric ophthalmologist who performed a detailed ocular examination and an ophthalmic assistant who performed the visual acuity (VA) examination and refraction in these children. VA was measured by Snellen’s visual acuity chart which was positioned at a distance of three meters.
If the VA was <3/60, the child was progressively taken closer to the chart until he/she was able to read the top letter. If the top letter could not be read at 1 m, counting fingers and hand movement was tried and perception of light and projection of rays in four quadrants were tested. VA was tested separately for each eye.
Anterior segment examination was conducted by using a portable handheld slit lamp in the schools and a mounted slit lamp in the outpatient department. Fundus evaluation under mydriasis was conducted by a portable indirect ophthalmoscope.
All information was recorded in the examination Records for Children with Blindness and Low Vision which had been developed by the WHO’s Program for the Prevention of Blindness.27 The form includes sections for recording demographic data and causes of visual loss using a descriptive anatomical and etiological classification. The diseases or conditions included in different etiological categories are as follows:
Hereditary Disease: Chromosomal Mitochondrial Autosomal Dominant Autosomal Recessive X-linked Intrauterine factor: Rubella Toxoplasmosis Drugs/alcohol Other.
Perinatal/Neonatal factor: Cerebral hypoxia/injury R.O.P Ophthalmia neonatorum Other.
Postnatal/ Infancy/Childhood factor: Vitamin A deficiency Measles Neoplasm Trauma Harmful Trad. Practices.
Cannot determine (unknown etiology): Cataract, Glaucoma/Buphthalmos, Retinoblastoma, Abnormality since birth.
Criteria for Visual Impairment and Blindness
Visual loss was classified by the WHO categories of VI.27 where blindness was defined as best- corrected VA (BCVA) <3/60 in the better eye, severe VI as VA <6/60 to 3/60 in the better eye, and moderate VI as BCVA <6/18 to 6/60 in the better eye. Blindness was categorized into two groups; BCVA<3/60 to light perception (LP) and no light perception (NLP). The visual field was not assessed.
Data Analysis
All the data were entered in Microsoft Excel and analyzed in the statistical package for social sciences (SPSS) software version 18, SPSS Inc, Chicago, Illinois. The frequency distribution was calculated for VI categories in different age groups. Similarly, frequency distribution was calculated for the etiology and anatomical site of involvement of VI and blindness in two different age groups: 7 to 12 years and 13 to 17 years. The chi-square test was applied to see any difference in the causes of avoidable blindness in the two age groups and gender.
Results
A total of 200 children aged 7 to 17 years participated in the study. Of these, 100 children in the moderate to severe visual impairment category were recruited from the outpatient department of TIO while 100 children in the blindness category were recruited from schools for the blind. Table 1 shows the distribution of children with VI and blindness in the age group of 7 to 12 years and 13 to 17 years. The mean age of children with moderate to severe VI and blindness was 11 (SD = 3) and 12 (SD 3), respectively. There were 111 (55.5%) children in the age group 7 to 12 years. Sixty percent of children with moderate to severe VI and 62% of children with blindness were male. Out of 200 children 45% had moderate VI, 5% had severe VI, 44.5% had blindness including LP and 5.5% had NLP.
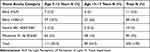 |
Table 1 Distribution of Children According to Visual Impairment Category and Age Group |
The etiology of VI and blindness according to the anatomical site of involvement has been described in Table 2. The “retina” was the most common anatomical site of involvement in the moderate to severe VI category while “whole globe” was the most common anatomical site of involvement in the blindness category. When looking at both groups combined, retinal diseases were the leading cause of blindness and VI Similarly, we analyzed children according to disease etiology in two different VI categories. [Table 3] In both groups, the etiology of eye diseases was often hereditary in nature followed by factors that developed after birth, infancy and childhood. In 25% of children the etiology was unknown. In total 43.5% of children had avoidable (treatable/preventable) causes of VI and blindness. There was no significant difference of avoidable and unavoidable blindness and VI in both age groups (p = 0.5) and gender (p = 0.4). Table 4 shows the causes of avoidable and unavoidable VI and blindness.
 |
Table 2 Distribution of Children According to Anatomical Site of Involvement |
 |
Table 3 Distribution of Children According to Disease Etiology |
 |
Table 4 Distribution of Blind and Visually Impaired Children According to Avoidable and Unavoidable Causes |
We compared our findings to studies found in the literature to explore changing trends in the etiology of VI and blindness in Nepalese children over the last few years. The cornea was the most common anatomical site of involvement (22.8%, 35.7%) in studies conducted by Jyoti et al and Kansakar et al, respectively. Retinal diseases and globe anomalies were common among children with VI after the refraction correction in studies conducted by Upreti et al and Thakur et al. Similarly, childhood factor was the most common etiology in the study conducted by Irina et al while hereditary was the most common factor in the study conducted by Jyoti et al Table 5 summarizes the leading etiological factors and the anatomical sites involved in the current study and the Nepali studies that have been published between 2008 and 2017.
 |
Table 5 Overview of the Leading Etiological Factors of Visual Impairment and Blindness in Nepal and the Anatomical Site Involved |
Discussion
In our study, we examined children with moderate to severe VI and blindness in two different age groups recruited via schools for the blind and outpatients of a tertiary eye hospital in Nepal. We found that the majority of children in the VI categories were in the younger age group (7–12 years), while the majority of children in the blindness categories were in the older age group (13–17 years). This may be due to lack of awareness of schools for the blind and stigma in the community about special education. However, another explanation may be the progression of eye diseases as children grow older. Consequently, these children may be enrolled in schools for the blind at a later age.
There are no registries for children with blindness and VI in Nepal. However, studies on blind schools and low vision clinics in hospitals can also give information on the causes of childhood VI and blindness. Repeating such studies every ten to fifteen years can provide insight into changing trends of causes of vision loss. Our study did show such a changing trend in the etiology of childhood VI and blindness compared to the studies conducted approximately a decade ago by Jyoti et al (conducted from 2008 to 2011) and Irina et al (conducted in 2006). Specifically, our study shows that retinal diseases are currently the most common cause of blindness among Nepalese children, followed by diseases involving the lens and the whole globe, whereas Irina et al and Jyoti et al found corneal opacity to be the leading cause of severe VI and blindness.19,20 Similar to our findings, studies conducted by Uprety et al in 2012–2013 in the eastern part of Nepal found retinal diseases to be the leading causes of moderate to severe VI. However, they also found a high number of (uncorrected) refractive errors.21 This finding is similar to findings from other developing countries.28–30 However, studies from developed countries have shown optic atrophy, cortical visual impairment and hereditary diseases to be the leading causes of blindness.31–33 In the study conducted by Kansakar et al, the age range of participants was 5 to 29 years so this also included young adults. However, around 60% of the participants were 15 years and below. Similarly, the age range in the study conducted by Jyoti et al was 6 to 32 years, with around 70% of participants 16 years or below. In both studies, the age range of participants was larger than in our study, however more than half of the participants were below 16 years of age, hence comparable to our study. There are population-based studies conducted by Adhikari et al and Byanju et al, which found amblyopia due to uncorrected refractive errors to be the leading cause of blindness.22,23 However, these studies included children from birth to 15 years. These studies depict the prevalence of childhood blindness in the population but the number is very small to study the etiology of childhood blindness and VI in the population. The decrease in corneal blindness as a cause found in our study probably is the result of good immunization coverage and effective vitamin A program implemented by the Nepali government.34–36
In the present study, we found around two-third of those who underwent pediatric cataract surgery had decreased vision because of stimulus deprivation amblyopia leading to poor vision and nystagmus. Most of these children had moderate to severe VI. This indicates a late detection and treatment. Consequently, timely detection and intervention with effective age-specific vision screening are very important in children. While analyzing the etiology of severe VI and blindness, we found that heredity was the most common etiology followed by eye diseases leading to blindness that had been developed post-natal, in infancy or at childhood. Importantly, we found that corneal diseases were less common in our study compared to previous studies. This could be a sign that the nationwide strategy to prevent vitamin-A deficiency is successful. Pseudophakia, aphakia and stimulus deprivation amblyopia were common causes of eye diseases leading to VI that had been developed post-natal, infancy or at childhood. Previous research suggests that around two-third of children in low-income countries have an avoidable blindness.5 We found that 43.5% of the causes of childhood VI and blindness were avoidable (either preventable or treatable). Our study showed retinal dystrophy as the leading cause of VI in children and “whole globe” disorders as a major cause of blindness. But also, that there is a big challenge in tackling blindness completely due to unavoidable causes such as for example microphthalmus, congenital anophthalmos and retinal dystrophies. More research is required to identify the causes of these diseases. Genetic counseling and genetic testing could play an important role in preventing these etiologies.
There are few limitations in conducting studies in schools for the blind. These schools underrepresent the population since children with multiple disabilities including VI, might not be attending the schools (and preschools). A lack of awareness about special education schools still exists in Nepal. Additionally, poverty, poor access to eye care eg when living in remote areas, and social stigma play a role in countries like Nepal, preventing blind children from attending regular schools.
Conclusion
In Nepal, retinal diseases are the most common causes of blindness and VI in children attending schools for the blind and visiting a hospital eye clinic. There is a changing trend in the etiology of blindness and VI partly explained by prevention programs and better treatment for corneal diseases in Nepal. However, approximately 44% of all children with VI and blindness live with potentially preventable conditions. To decrease the levels of VI and blindness in Nepal, periodic vision screening programs, genetic counselling and testing, and increased accessibility of eye care should be one of the priorities of government policymakers.
Acknowledgment
We would like to express our appreciation to Professor Dr. Suman S Thapa, Ms. Radhika Uprety, Mr. Manish Poudel, Mr. Pradeep Banjara, Ms. Rina Budathoki and all the principals, teachers and students of integrated schools for the blind.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Rahi JS, Gilbert CE, Foster A, Minassian D. Measuring the burden of childhood blindness. Br J Ophthalmol. 1999;83(4):387–388. doi:10.1136/bjo.83.4.387
2. WHO.int. Available from: https://www.who.int/news-room/fact-sheets/detail/blindness-and-visual-impairment.
3. Gilbert C, Muhit M. Twenty years of childhood blindness: what have we learnt? Community Eye Health. 2008;21(67):46–47.
4. Muhit M, Gilbert C. A review of the epidemiology and control of childhood blindness. Trop Doct. 2003;33(4):197–201. doi:10.1177/004947550303300403
5. World Health Organization. Report of WHO/IAPB Scientific Meeting. World Health Organization; 2000.
6. Solebo AL, Teoh L, Rahi J. Epidemiology of blindness in children. Arch Dis Child. 2017;102(9):853–857. doi:10.1136/archdischild-2016-310532
7. Gilbert C, Bowman R, Malik AN. The epidemiology of blindness in children: changing priorities. Community Eye Health. 2017;30(100):74–77.
8. Gilbert CE, Anderton L, Dandona L, Foster A. Prevalence of visual impairment in children: a review of available data. Ophthalmic Epidemiol. 1999;6(1):73–82. doi:10.1076/opep.6.1.73.1571
9. Rahi JS, Cumberland PM, Peckham CS. British Childhood Visual Impairment Interest Group. Improving detection of blindness in childhood: the British Childhood Vision Impairment study. Pediatrics. 2010;126(4):e895–903. doi:10.1542/peds.2010-0498
10. Boonstra N, Limburg H, Tijmes N, van Genderen M, Schuil J, van Nispen R. Changes in causes of low vision between 1988 and 2009 in a Dutch population of children: acta Ophthalmologica 2011. Acta Ophthalmol. 2012;90(3):277–286. doi:10.1111/j.1755-3768.2011.02205.x
11. Muhit MA, Shah SP, Gilbert CE, Hartley SD, Foster A. The key informant method: a novel means of ascertaining blind children in Bangladesh. Br J Ophthalmol. 2007;91(8):995–999. doi:10.1136/bjo.2006.108027
12. Gilbert C. Changing challenges in the control of blindness in children. EYE. 2007;21(10):1338–1343. doi:10.1038/sj.eye.6702841
13. Ezinne NE, Nnadi CJ, Mashigo KP, Onoikhua EE. Causes of Childhood Blindness among Children Seen at the National Eye Centre, Kaduna. Nigeria J Ophthalmic Clin Res. 2018;5:39.
14. Gogate P, Deshpande M, Sudrik S, Taras S, Kishore H, Gilbert CE. Changing pattern of childhood blindness in Maharashtra, India. Br J Ophthalmol. 2007;91:8–12. doi:10.1136/bjo.2006.094433
15. Muecke J, Hammerton M, Aung YY, et al. A survey of visual impairment and blindness in children attending seven schools for the blind in Myanmar. Ophthalmic Epidemiol. 2009;16:370–377. doi:10.3109/09286580903312269
16. Akinsola FB, Aribaba OT, Onakoya AO, Adefule-Ositelu AO, Majekodunmi AA. Causes of childhood blindness in a tertiary hospital in Lagos. J Clin Sci. 2005;5:23–26.
17. Bamashmus MA, Al-Akily SA. Profile of childhood blindness and low vision in Yemen: a hospital-based study. East Mediterr Health J. 2010;16(4):425–428. doi:10.26719/2010.16.4.425
18. Gao Z, Muecke J, Edussuriaya K, et al. A survey of severe visual impairment and blindness in children attending thirteen schools for the blind in Sri Lanka. Ophthalmic Epidemiol. 2011;18:36–43. doi:10.3109/09286586.2010.545504
19. Kansakar I, Thapa HB, Salma KC, Ganguly S, Kandel RP, Rajasekaran S. Causes of vision impairment and assessment of need for low vision services for students of blind schools in Nepal. Kathmandu Univ Med J. 1970;7(1):44–49. doi:10.3126/kumj.v7i1.1764
20. Shrestha JB, Gnyawali S, Upadhyay MP. Causes of blindness and visual impairment among students in integrated schools for the blind in Nepal. Ophthalmic Epidemiol. 2012;19(6):401–406. doi:10.3109/09286586.2012.722245
21. Uprety S, Khanal S, Morjaria P, Puri LR. Profile of paediatric low vision population: a retrospective study from Nepal. Clin Exp Optom. 2016;99(1):61–65. doi:10.1111/cxo.12314
22. Byanju RN, Kandel RP, Sharma P, Thapa HB, Shrestha M, Bassett K. Childhood blindness and visual impairment in the Narayani Zone of Nepal: a population-based survey. Ophthalmic Epidemiol. 2019;26(4):257–263. doi:10.1080/09286586.2019.1604976
23. Adhikari S, Shrestha MK, Adhikari K, Maharjan N, Shrestha UD, Causes of visual impairment and blindness in children in three ecological regions of Nepal, Nepal Pediatric Ocular Diseases Study. Clinical Ophthalmology. 2015;9:1543–1547. doi:10.2147/OPTH.S89431
24. Kumar A, Joshi P, Kandel H, Bhatta S. Profile of low vision clinics in eastern region of Nepal: a retrospective study. Br J Visual Impairment. 2011;29(3):215–226. doi:10.1177/0264619611414990
25. Mower AG. The Convention on the Rights of the Child: International Law Support for Children. Praeger; 1997.
26. World Health Organization. ICD-10: International Statistical Classification of Diseases and Related Health Problems, 10th Revision. Geneva:: World Health Organization; 1994.
27. Gilbert C, Foster A, Négrel AD, Thylefors B. Childhood blindness: a new form for recording causes of visual loss in children. Bull World Health Organ. 1993;71(5):485–489.
28. Raihan A, Rahmatullah S, Arefin MH, Banu T. Prevalence of significant refractive error, low vision and blindness among children in Bangladesh. Int Congr Ser. 2005;1282:433–437. doi:10.1016/j.ics.2005.05.111
29. Courtright P, Hutchinson AK, Lewallen S. Visual impairment in children in middle- and lower-income countries. Arch Dis Child. 2011;96(12):1129–1134. doi:10.1136/archdischild-2011-300093
30. Kaphle D, Marasini S, Kalua K, Reading A, Naidoo KS. Visual profile of students in integrated schools in Malawi. Clin Exp Optom. 2015;98(4):370–374. doi:10.1111/cxo.12269
31. Ingelse J, Steele G. Characteristics of the pediatric/adolescent low-vision population at the Illinois School for the Visually Impaired. Optometry. 2001;72(12):761–766.
32. de Carvalho KM, Minguini N, Filho DCM, Kara-José N. Characteristics of a pediatric low-vision population. J Pediatr Ophthalmol Strabismus. 1998;35(3):162–165. doi:10.3928/0191-3913-19980501-09
33. Rahi JS, Cable N; British Childhood Visual Impairment Study Group. Severe visual impairment and blindness in children in the UK. Lancet. 2003;362(9393):1359–1365. doi:10.1016/S0140-6736(03)14631-4
34. Public Health Update. Vitamin A supplementation, deworming tablet & Baal vita distribution campaign. Public Health Update; 2020. Available from: https://www.publichealthupdate.com/vitamin-a-supplementation-deworming-tablet-baal-vita-distribution-campaign/.
35. Gorstein J, Shreshtra RK, Pandey S, Adhikari RK, Pradhan A. Current status of vitamin A deficiency and the National Vitamin A Control Program in Nepal: results of the 1998 National Micronutrient Status Survey. Asia Pac J Clin Nutr. 2003;12(1):96–103.
36. Thorne-Lyman AL, Parajuli K, Paudyal N, et al. To see, hear, and live: 25 years of the vitamin A programme in Nepal. Matern Child Nutr. 2022;18(S1):e12954. doi:10.1111/mcn.12954
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
