Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 16
Causes of Drug-Induced Severe Cutaneous Adverse Reaction Epidermal Necrolysis (EN): An Analysis Using FDA Adverse Event Reporting System (FAERS) Database
Received 20 June 2023
Accepted for publication 11 August 2023
Published 16 August 2023 Volume 2023:16 Pages 2249—2257
DOI https://doi.org/10.2147/CCID.S422928
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jeffrey Weinberg
Weiqiang Fei,1 Jun Shen,2 Hui Cai3
1College of Nursing, Hangzhou Vocational & Technical College, Hangzhou, Zhejiang Province, People’s Republic of China; 2Nursing Department, Sir Run Run Shaw Hospital Affiliated to Zhejiang University School of Medicine, Hangzhou, Zhejiang Province, People’s Republic of China; 3Nursing Department, Jiangsu Province Hospital Chinese Medicine, Affiliated Hospital of Nanjing University of Chinese Medicine, Nanjing, People’s Republic of China
Correspondence: Weiqiang Fei, College of Nursing, Hangzhou Vocational & Technical College, 68 Xueyuan Street, Xiasha Higher Education Park, Qiantang District, Hangzhou, Zhejiang Province, 310018, People’s Republic of China, Tel/Fax +86-571-56700120, Email [email protected]
Purpose: The purpose of the study is to analyze FAERS data to identify drugs associated with Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN), determine demographics, drug classes involved, most likely resulted in death, and highlight emerging trends in SJS/TEN reactions.
Patients and Methods: We reviewed the publicly available FAERS database from 2004– 2021. Using search terms “Stevens-Johnson syndrome” or “Toxic epidermal necrolysis”, we identified the reports of SJS/TEN or SJS/TEN followed by death that might associated with specific drugs. Then the amounts and trends were counted analyzed.
Results: During the study period of 2004– 2021, the Food and Drug Administration (FDA) received a total of 14,363,139 reports of adverse reactions, among which 24,976 were linked to SJS or TEN. After excluding the cases with incomplete or insufficient information on age, gender, or country of origin, the median median age of patients was 53.82 (IQR = 57.52), the females accounted for 56.59% (12,827 cases) and 8,507 (38.34%) originated in the United States. The top 50 drugs were associated with 15,149 cases (60.65%). The subsequent fatal outcome occurring in 4878 out of 24,976 cases (19.53%). Top 3 drug classes associated with SJS/TEN in FAERS were antiepileptics, non-steroidal anti-inflammatory drugs (NSAIDs) and others. Top drug classes associated with SJS/TEN deaths were antineoplastic agents and cephalosporins. Linear regression showed that the annual percentage of monoclonal antibody-related SJS/TEN reactions increased at an average rate of 0.25% (95% confidence interval: 0.18, 0.32) from 0.00% in 2004 to 4.79% in 2021, faster than any other drug class except antigout drug (allopurinol).
Conclusion: By using the publicly available FAERS data, we have identified some important themes and trends in drug-related SJS/TEN reactions. Monoclonal antibodies and proton pump inhibitors are drugs with emerging trends causing SJS/TEN. Additionally, cephalosporin antibiotics have a higher mortality rate following SJS/TEN.
Keywords: Stevens-Johnson syndrome, SJS, toxic epidermal necrolysis, TEN, adverse drug reactions, fatal outcome, trends
Introduction
Epidermal necrolysis (EN), a severe cutaneous adverse reaction, comprises two subtypes, namely toxic epidermal necrolysis (TEN) and Stevens-Johnson syndrome (SJS). The condition is characterized by the loss of the epidermis, resulting from extensive apoptosis and/or necroptosis of keratinocytes.1 SJS and TEN are part of a spectrum of diseases, with SJS representing a milder form of epidermolysis involving an area of less than 10% of the body surface area. Conversely, TEN is a more severe form, involving an area of epidermolysis exceeding 30% of the body surface area. Cases with skin involvement between 10% and 30% are categorized as SJS/TEN overlap.
Hsu et al2 conducted a study in the United States and reported that between 2009 and 2012, the annual incidence rates for SJS, TEN, and SJS/TEN overlap syndrome were 9.2, 1.9, and 1.6 cases per million adults, respectively. Meanwhile, a UK-based observational study by Frey et al3 estimated the overall incidence rate for SJS/TEN to be 5.76 cases per million between 1995 and 2013. In Korea, Yang et al4 reported an estimated incidence rate ranging from 3.96 to 5.03 cases per million persons per year for SJS and 0.94 to 1.45 cases per million persons per year for TEN between 2009 and 2013. According to Doaa et al,5 the incidence rates for SJS/TEN in Egypt ranged from 1.7% in 2012 to 7.7% in 2017. Notably, mortality rates for SJS, TENSJS/TEN, and SJS/TEN overlap syndrome were reported to be 4.8–9%, 14.8–48%, and 19.4–29%, respectively.2,6 Furthermore, complications arising from SJS/TEN are frequent and constitute critical factors that significantly impact patients’ health and economic well-being.
The pathogenesis of SJS/TEN is primarily linked to the genetic background of the body, and it is frequently triggered by specific medications. Immune-mediated responses are responsible for the development of most cases of SJS and TEN, and these responses involve the activation of different inflammatory mechanisms. Type IV delayed-type hypersensitivity reactions, which involve multiple cytokines, are the main cause of both TEN and SJS. Additionally, the genetic background of the body is mainly associated with polymorphisms in human leukocyte antigen (HLA).7,8 A variety of drugs, including anticonvulsants9,10 like carbamazepine, lamotrigine, and phenytoin; allopurinol11 used for treating gout; nonsteroidal anti-inflammatory drugs (NSAIDs)12 such as ibuprofen and naproxen; sulfonamide antibiotics13 like sulfamethoxazole; and antiretroviral drugs14,15 such as nevirapine can cause SJS/TEN.
Prompt diagnosis, discontinuation of the suspect drug, and specialized medical intervention are critical factors for improving patients’ chances of survival following SJS/TEN. Nonetheless, there are limited summarized data available on the exogenous drugs that can lead to the development of SJS/TEN. Furthermore, the dearth of comprehensive analysis based on real-world big data compounds this issue.
Due to certain limitations inherent in the FDA Adverse Event Reporting System (FAERS) data,16 which record adverse drug events data from spontaneous reporting in diverse populations, it is challenging to draw definitive conclusions regarding the prevalence, incidence, and causality of adverse drug reactions. Nevertheless, the dataset available through FAERS consists of a substantial number of drug-related adverse events. In light of this, we collected FAERS data to evaluate the prevalence of specific drugs linked to SJS/TEN. Our objective was to identify the top 50 drugs implicated in the development of SJS/TEN, as well as 20 drugs that most likely resulted in death following their administration. Additionally, we sought to examine the evolution of these reports over time and compare our findings to those reported in the existing literature.
Materials and Methods
Data Source and Collection
The quarterly data extraction document (2004Q1-2021Q4) was obtained by downloading from the FAERS. The dataset includes demographic and administrative details, initial report case identification numbers, drug and reaction information, patient outcomes, and information about the reporting source. FAERS data files are available for free download by selecting a year and choosing ASCII for the desired quarter, which can be accessed at https://fis.fda.gov/extensions/FPD-QDE-FAERS/FPD-QDE-FAERS.html. According to Chinese measures for ethical review of life science and medical research, if the research is conducted using legally obtained public data or anonymized data, ethical review can be exempted. Our research was based on the FAERS data, which are freely accessible on the FDA website and all data were anonymized by FDA and in compliance with the ethical standard. Therefore, no further ethical measure was required.
Signal Detection Method
A query was conducted using the medical terms “Stevens-Johnson syndrome” or “Toxic epidermal necrolysis” in the FDA Data field. The search results were filtered to retain data within the time frame of 2004–2021. To focus our results on the drugs that were most likely to cause adverse events, we limited our analysis to the reports with the role code “PS”, which meant the drug was considered as the primary suspect by the reporter. Drug names were standardized to their Generic Name using Drugbank and drug classification was conducted using WHOATC data from https://www.whocc.no/atc_ddd_index/, supplemented or adjusted manually.
The number of adverse events associated with specific drugs or drug categories, occurring within different years, were counted to identify the top 50 drugs. The top 6 countries/regions with the highest number of reported adverse events were identified based on the country of occurrence, and the top 10 drugs in these countries/regions were calculated. The annual trends of the top 50 drugs were determined by analyzing time series data and generating linear regression plots.
Results
Top 50 Drugs Associated with SJS/TEN
During the selected study period of 2004–2021, the FDA reported a total of 14,363,139 adverse reactions, out of which 24,976 were associated with SJS/TEN. Excluding the patients without age information, the median age of SJS/TEN patients was 53.82 (n=15,149, IQR = 57.52). Excluding patients without or unknown gender information, females accounted for 56.59% (12,827 cases), while males accounted for 42.44% (9620 cases). The remaining cases were Not Specified (142 cases, 0.63%) or Unknown (76 cases, 0.34%). Excluding patients without country information, 8507 out of 22,191 cases (38.34%) originated in the USA. The top 50 drugs in amount were associated with 15,149 cases (60.65%), the main categories include Antiepileptics, NSAIDs, Antigout Drug, etc (See Supplementary Figure 1). The subsequent outcome of SJS/TEN was fatal in 4878 out of 24,976 cases (19.53%).
Lamotrigine was the most commonly associated with SJS/TEN in the FDA adverse event data, accounting for 9.63% (2404/24976) of all SJS/TEN adverse event reports during the study period. The details for the top 50 drugs see Supplementary Table 1.
The Highest Ranked Drug Class Associated with SJS/TEN
We categorized the top 50 drugs (Table 1, Supplementary Table 2). The ranking of the main drug classes associated with SJS/TEN in cases reported to the FDA were antiepileptics, NSAIDs, others (antigout drug, immunosuppressants, diuretic drug, selective calcium channel blockers, chemotherapy for cancer, antimalarial drugs), other antibiotics, quinolones, lactam antibiotics, macrolides, proton pump inhibitor, antivirals, monoclonal antibodies, sulfa-derived medications and antidepressants.
 |
Table 1 The Top 50 Drug Classes Associated with Reports of SJS or TEN in FAERS from 2004–2021 |
In terms of drug categories, antiepileptic drugs were found to be the most commonly associated drug class with SJS/TEN, comprising 19.37% (4839/24976) of all reported adverse events during the study period. The proportion of antiepileptic drug-related SJS/TEN cases peaked in 2011, representing 34.20% of the total cases in that year. Phenytoin was the main drug involved in these cases, with a surge to 217 cases in 2011, accounting for 15.76% of the total cases. The second highest class of drugs identified in this study was NSAIDs, which accounted for 13.97% (3489/24976) of all reports. The representative drug are valdecoxib and Ibuprofen. Antibiotics, including quinolones, lactam antibiotics, and other antibiotics, were responsible for 16.23% (2459/24976) of all reports.
Linear regression analysis was carried out for each major drug class associated with SJS/TEN. The analysis of other antibiotics, monoclonal antibodies, and proton pump inhibitors, as well as others, such as antigout drugs, immunosuppressants, diuretic drugs, selective calcium channel blockers, chemotherapy for cancer, and antimalarial drugs (as detailed in Tables 1–3 and Figures 1–2) demonstrated an increasing trend over time. The annual percentage of monoclonal antibody-related SJS/TEN reactions increased at an average rate of 0.25% (95% confidence interval: 0.18, 0.32) from 0.00% in 2004 to 4.79% in 2021. This was faster than any other drug class except “others”. The fastest growing single drug was allopurinol (antigout drug class), with an annual increase rate of 0.32% (95% confidence interval: 0.22, 0.42), from 0.43% in 2004 to 4.25% in 2021. No significant differences were observed in other drug classes from year to year.
 |
Table 2 Linear Regressions on the Percent of SJS/TEN Cases Reported in Association with Drug Classes |
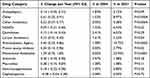 |
Table 3 Linear Regressions on the Percent of SJS/TEN Death Cases Reported in Association with Drug Classes |
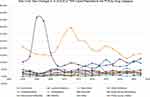 |
Figure 1 Year Over Year Changes in % of SJS or TEN Cases Reported to the FDA by Drug Category. |
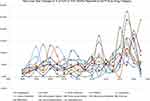 |
Figure 2 Year Over Year Changes in % of SJS or TEN Deaths Reported to the FDA by Drug Category. |
National Reporting Data
Subsequently, we calculated the proportion of SJS/TEN cases reported in the United States (US) for each drug. SJS/TEN reactions reported in the US accounted for 8507 out of 24,976 (34.06%) cases in the corresponding countries. Lactam antibiotics (14.13%) and proton pump inhibitors (11.09%) were reported in less than 15% of SJS/TEN cases in the US. All other drug classes were within the range of 20–53% (as shown in Table 2 and Supplementary Table 1).
Among the top 50 drugs, valdecoxib (92.84%), phenytoin (80.11%), sulfamethoxazole\trimethoprim (60.51%), and celecoxib (71.81%) were reported to be associated with more than 60% of SJS/TEN reactions in the United States, while diclofenac (7.18%), acetylsalicylic acid (4.71%), piperacillin/tazobactam (8.65%), and lansoprazole (1.08%) were reported with less than 10% of SJS/TEN reactions in the United States. The top ten drugs associated with SJS/TEN reactions reported by the FDA ranged from 17.87% to 92.84% in the United States.
In order to gain a more comprehensive understanding of the regional distribution of SJS/TEN cases reported to the FDA during the study period, we identified six countries that reported the highest number of cases and determined the top 10 drugs associated with SJS/TEN in each of these countries (refer to Supplementary Table 3 for details).
Death Following SJS/TEN Reaction
Over the period from 2004 to 2021, FDA received 4878 cases of SJS/TEN deaths reports, representing 19.53% of all SJS/TEN cases reported. These fatalities comprised 0.03% of all adverse events reported during the same period. Our analysis revealed that the annual number of SJS/TEN deaths reports to the FDA increased over time (linear regression β=16.12, 95% CI: 9.21–23.02, P<0.001), from 85 reports in 2004 to 326 reports in 2021. The proportion of SJS/TEN deaths reported increased a little as a percentage of total SJS/TEN reports (linear regression β=0.40, 95% CI: 0.14–0.66, P=0.0051), increasing from 18.20% in 2004 to 19.78% in 2021. Detailed information on these findings is presented in Supplementary Table 4.
The median age of patients reporting death as a result of SJS/TEN was 58 years [IQR: 72], and 53.56% of them were female. We have identified 55 drugs with 20 or more SJS/TEN death reports, as listed in Supplementary Table 5.
Eight drugs had the death rate exceeded 50% following SJS/TEN between 2004 and 2021 compared to the number of drug-specific SJS/TEN reports that occurred during this time period. These drugs were ceftazidime (20 deaths, 60.61%), alendronic acid (25 deaths, 58.14%), lansoprazole (53 deaths, 56.99%), amphotericin B (21 deaths, 55.26%), methotrexate (80 deaths, 54.42%), bortezomib (20 deaths, 54.05%), piperacillin/tazobactam (56 deaths, 52.34%), and meropenem (40 deaths, 50.63%).
There were 16 drugs among these 55 drugs, including cephalosporins (cefuroxime, ceftazidime), meropenem, docetaxel, capecitabine, metformin, alendronic acid, linezolid, rifampicin, rituximab, bendamustine, ampicillin, enoxaparin, americin B, cyclosporine, and bortezomib, were not included in the list of the top 50 drugs associated with SJS/TEN cases. Among the top 30 reported drugs in association with SJS/TEN, rank 24 zonisamide (11 total deaths) and rank 26 amlodipine (19 total deaths) did not have 20 or more reports of SJS/TEN death.
Categorized by drug class (Supplementary Table 6), SJS/TEN-related deaths were highest for antiepileptic drugs, followed by other antibiotics, as well as antigout drugs (specifically allopurinol), NSAIDs, quinolones, lactam antibiotics, and others. The ratio of SJS/TEN-related deaths to the total number of SJS/TEN cases was determined. The lowest ratios were observed for NSAIDs and antiepileptics, whereas the highest ratios were associated with antineoplastic agents, cephalosporins, and other drugs. See Supplementary Table 7 for more details.
Calculating the proportion of deaths relative to the number of SJS/TEN cases, NSAIDs and antiepileptics had the lowest proportion, while antineoplastic agents, cephalosporins, and others were the top three in rank.
Discussion
Our analysis of the publicly available FAERS data has revealed significant patterns and developments in the documentation of SJS/TEN drug reactions. Among these, antibiotics emerged as a prominent class of drugs that were frequently reported to cause both general SJS/TEN reactions and SJS/TEN reactions leading to fatality. Additionally, we detected a growing incidence of SJS/TEN reactions associated with monoclonal antibodies and proton pump inhibitors over the course of the study period. A yearly rise in reports of SJS/TEN reactions has been observed between 2004 and 2019, followed by a declining trend from 2019 to 2021.
Within our study period, females comprised the majority of reported SJS/TEN reactions submitted to the FDA, with a female-to-male ratio of 12,827:9620. This outcome aligns with prior literature reports indicating a higher incidence of SJS/TEN among females.17,18
It is noteworthy that monoclonal antibodies were the fastest growing category of SJS/TEN events among all categories, and also the fastest growing category of deaths following SJS/TEN. This may be consistent with the relevance of this class of drugs in treatment and their increasing use. This is also in line with the results of a PubMed literature search.19–25 Most of the case reports related to monoclonal antibodies were concentrated after 2016, and there is a trend of increase. We noted that the most important antibodies leading to this phenomenon were humanized monoclonal antibodies pembrolizumab and nivolumab. The available data did not currently permit the identification of risk factors associated with the emergence of SJS/TEN-like reactions to monoclonal antibodies. One possible explanation for this phenomenon may be genetic variability in the genes regulating immune function. Further studies encompassing clinical, pathological, and basic science investigations will ultimately be required to comprehensively elucidate the mechanisms, attributes, and optimal management strategies for SJS/TEN-like reactions arising in response to monoclonal antibodies.
In the EuroSCAR study,26 a case-control surveillance of severe cutaneous adverse reactions conducted in Europe and published in 2008, it was observed that pantoprazole exhibited a high univariate relative risk of causing SJS/TEN. However, due to the low number of cases, a precise estimation of risk could not be made. Lin27 conducted a retrospective analysis of patients with drug hypersensitivity reactions (DHR) related to proton pump inhibitors (PPI) from multiple medical centers in Taiwan. The study period spanned from January 2003 to April 2016, and a total of 27 cases of PPI-related SJS/TEN were identified. Later, Frey et al28 observed an increased risk of SJS/TEN among new users of omeprazole, lansoprazole, and to a lesser extent rabeprazole. Incorporating our analysis findings with previous research, we posit that PPIs should be included among the potential suspects in instances of drug-induced subacute lupus erythematosus. Additionally, there is a significant body of evidence regarding PPI-related occupational contact dermatitis.
Regarding deaths after SJS/TEN, ceftazidime, a cephalosporin drug, accounted for 60.61% of all cases resulting in death after SJS/TEN between 2004 and 2021, despite being ranked outside the top 50 drugs causing SJS/TEN during this time period. In addition, two other cephalosporin drugs, cefuroxime and ceftazidime, had over 20 reported deaths, but their overall cases of SJS/TEN were ranked outside the top 50 as well. Cephalosporins were shown to be the most commonly suspected drug category in SCAR study29 where SJS/TEN were induced in 170 patients by β-lactam antibiotics and the mortality rate for SJS/TEN caused by β-lactam antibiotics was 7.4%. In another study, the mortality rate was 34% (87/259) for TEN and only 1% (2/315) for SJS. Although our data on the proportion of deaths did not exclude the impact of comorbidities, this result is much higher than previous studies and warrants further attention in clinical use, as it ranks highly when calculated using the same method, second only to antitumor drugs.
One major limitation of self-reported data in FAERS is the lack of denominator data and the high risk of selection and reporting bias, so the data should not be used to estimate the true incidence rates of SJS/TEN reactions or SJS/TEN deaths for drugs. Drugs that are closely monitored during administration (eg, in surgical settings, infusion centers) may have lower rates of SJS/TEN reactions that result in death due to early identification. Specifically, relying on patient, physician, pharmaceutical company, or literature reports submitted to the FDA is not an accurate estimate of the true amount of drug SJS/TEN reactions, as the data itself is limited by under reporting of cases, uncertain causality, and potential duplicate reports, despite our efforts to de-duplicate the data. Additionally, FAERS lacks racial data, which is an important narrative component in considering all drug adverse reactions and ecological and genetic factors.
In the end, we believe that our analysis of FAERS data confirms previous population studies on SJS/TEN, and thus, FAERS data can be used to identify themes and trends of SJS/TEN reactions and guide our clinical practitioners to be alert to the clinical risks associated with related drugs, and to monitor closely at an early stage, thereby effectively reducing clinical drug risks.
Conclusion
Through our examination of publicly available FAERS data, we have identified important themes and trends in drug-related SJS/TEN reactions. Monoclonal antibodies and proton pump inhibitors are emerging trends. Additionally, cephalosporin antibiotics may have a higher mortality rate following SJS/TEN. Although our reports are limited due to the voluntary nature of FDA FAERS reporting, they raise awareness of important issues and can be used to guide SJS/TEN researchers in generating hypotheses related to potentially important drugs.
Ethics Statement
According to item 1 and 2 of Article 32 of “the Measures for Ethical Review of Life Science and Medical Research Involving Human Subjects”, which was reviewed by the National Science and Technology Ethics Committee, approved by the State Council of China, and jointly promulgated by the National Health Commission, the Ministry of Education, the Ministry of Science and Technology and the State Administration of Traditional Chinese Medicine on Feb. 18, 2023, on the following circumstances:
- The research is conducted using legally obtained public data or data generated through observation and does not interfere with public behavior
- Use of anonymized data for research
Ethical review can be exempted to reduce unnecessary burden on researchers and promote life science and medical research involving human beings. Our research was based on the FAERS database on the FDA website, which are freely accessible to all the medical researchers, all the participants data were anonymized by FDA and in compliance with the ethical standard. Therefore, no further ethical measure was required. For more information on China’s guideline on research ethics and governance, please see the governmental web-page: https://www.gov.cn/zhengce/zhengceku/2023-02/28/content_5743658.htm.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Heng YK, Lee HY, Roujeau J-C. Epidermal necrolysis: 60 years of errors and advances. Br J Dermatol. 2015;173(5):1250–1254. doi:10.1111/bjd.13989
2. Hsu DY, Brieva J, Silverberg NB, et al. Morbidity and mortality of Stevens-Johnson syndrome and toxic epidermal necrolysis in United States adults. J Invest Dermatol. 2016;136(7):1387–1397. doi:10.1016/j.jid.2016.03.023
3. Frey N, Jossi J, Bodmer M, et al. The epidemiology of Stevens-Johnson syndrome and toxic epidermal necrolysis in the UK. J Invest Dermatol. 2017;137(6):1240–1247. doi:10.1016/j.jid.2017.01.031
4. Yang M-S, Lee JY, Kim J, et al. Incidence of Stevens-Johnson syndrome and toxic epidermal necrolysis: a nationwide population-based study using national health insurance database in Korea. PLoS One. 2016;11(11):e0165933. doi:10.1371/journal.pone.0165933
5. Abou-Taleb DAE, El-Sayed AM, Ghabesha AA, et al. Severe cutaneous adverse drug reactions: incidence, clinical patterns, causative drugs and modalities of treatment in Assiut University Hospital, Upper Egypt. Dermatol Ther. 2020;33(6):e14176. doi:10.1111/dth.14176
6. Paulmann M, Mockenhaupt M. Severe skin reactions: clinical picture, epidemiology, etiology, pathogenesis, and treatment. Allergo J Int. 2019;28(8):311–326. doi:10.1007/s40629-019-00111-8
7. Gupta LK, Martin AM, Agarwal N, et al. Guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis: an Indian perspective. Indian J Dermatol Venereol Leprol. 2016;82(6):603–625. doi:10.4103/0378-6323.191134
8. Zhang J, Lei Z, Xu C, et al. Current perspectives on severe drug eruption. Clin Rev Allergy Immunol. 2021;61(3):282–298. doi:10.1007/s12016-021-08859-0
9. Lucia L, Silvia C, Paolo B, et al. Clinical features, outcomes and treatment in children with drug induced Stevens-Johnson Syndrome and toxic epidermal necrolysis. Acta Biomed. 2019;90:52–60.
10. Edinoff AN, Nguyen LH, Fitz-Gerald MJ, et al. Lamotrigine and Stevens-Johnson syndrome prevention. Psychopharmacol Bull. 2021;51(2):96–114.
11. Lavu A, Thiriveedi S, Thomas L, et al. Clinical Utility of HLA-B*58:01 Genotyping to Prevent Allopurinol-Induced SJS/TEN. Hosp Pharm. 2021;56(6):660–663. doi:10.1177/0018578720934972
12. Kowalski ML, Asero R, Bavbek S, et al. Classification and practical approach to the diagnosis and management of hypersensitivity to nonsteroidal anti-inflammatory drugs. Allergy. 2013;68(10):1219–1232. doi:10.1111/all.12260
13. Asyraf PA, Kusnadi IF, Stefanus J, et al. Clinical manifestations and genetic influences in sulfonamide-induced hypersensitivity. Drug Healthc Patient Saf. 2022;14:113–124. doi:10.2147/DHPS.S347522
14. Peter J, Choshi P, Lehloenya RJ. Drug Hypersensitivity in HIV Infection. Curr Opin Allergy Clin Immunol. 2019;19(4):272. doi:10.1097/ACI.0000000000000545
15. Budamakuntla L, Challa N, Basappa P, et al. A retrospective study of spectrum of nevirapine induced cutaneous drug reactions in HIV positive patients. UCMS. 2015;12:85–89.
16. Sakaeda T, Tamon A, Kadoyama K, et al. Data mining of the public version of the FDA adverse event reporting system. Int J Med Sci. 2013;10(7):796–803. doi:10.7150/ijms.6048
17. Schöpf E, Stühmer A, Rzany B, et al. Toxic epidermal necrolysis and Stevens-Johnson syndrome. an epidemiologic study from West Germany. Arch Dermatol. 1991;127(6):839–842. doi:10.1001/archderm.1991.01680050083008
18. Lim VM, Do A, Berger TG, et al. A decade of burn unit experience with Stevens-Johnson Syndrome/Toxic epidermal necrolysis: clinical pathological diagnosis and risk factor awareness. Burns. 2016;42(4):836–843. doi:10.1016/j.burns.2016.01.014
19. Maloney NJ, Ravi V, Cheng K, et al. Stevens‐Johnson Syndrome and toxic epidermal necrolysis‐like reactions to checkpoint inhibitors: a systematic review. Int J Dermatol. 2020;59(6):e183–e188. doi:10.1111/ijd.14811
20. Dasanu CA. Late-Onset Stevens-Johnson syndrome due to nivolumab use for hepatocellular carcinoma. J Oncol Pharm Pract. 2019;25(8):2052–2055. doi:10.1177/1078155219830166
21. Hong D, Sloane DE. Hypersensitivity to monoclonal antibodies used for cancer and inflammatory or connective tissue diseases. Ann Allergy Asthma Immunol. 2019;123(1):35–41. doi:10.1016/j.anai.2019.04.015
22. Robinson S, Saleh J, Curry J, et al. Pembrolizumab-induced Stevens-Johnson syndrome/toxic epidermal necrolysis in a patient with metastatic cervical squamous cell carcinoma: a case report. Am J Dermatopathol. 2020;42(4):292–296. doi:10.1097/DAD.0000000000001527
23. Cao J, Li Q, Zhi X, et al. Pembrolizumab-induced autoimmune Stevens-Johnson syndrome/toxic epidermal necrolysis with myositis and myocarditis in a patient with esophagogastric junction carcinoma: a case report. Transl Cancer Res. 2021;10(8):3870–3876. doi:10.21037/tcr-21-470
24. Gallo Marin B, Oliva R, Kahn B, et al. Pembrolizumab-induced toxic epidermal necrolysis in a patient with metastatic esophageal adenocarcinoma. R I Med J. 2022;105:34–36.
25. Lee O, Masood M, Nutan F. Case series of Stevens-Johnson syndrome and toxic epidermal necrolysis with nivolumab and nivolumab/ipilimumab combination therapy in metastatic melanoma. J Drugs Dermatol. 2022;21(5):529–530. doi:10.36849/JDD.6559
26. Mockenhaupt, 11 human leukocyte antigen-associated severe cutaneous adverse drug reactions: from bedside to bench and beyond – PMC. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6676067/.
27. Lin C-Y, Wang C-W, Hui C-YR. Delayed‐type hypersensitivity reactions induced by proton pump inhibitors: a clinical and in vitro T‐cell reactivity study. Allergy. 2018;73(1):221–229. doi:10.1111/all.13235
28. Frey N, Bodmer M, Bircher A, et al. Stevens–Johnson syndrome and toxic epidermal necrolysis in association with commonly prescribed drugs in outpatient care other than anti-epileptic drugs and antibiotics: a population-based case–control study. Drug Saf. 2019;42(1):55–66. doi:10.1007/s40264-018-0711-x
29. Kim M-H, Kang DY, Nam Y-H, et al. Clinical aspects of severe cutaneous adverse reactions caused by beta-lactam antibiotics: a study from the Korea SCAR Registry. World Allergy Organ J. 2023;16(1):100738. doi:10.1016/j.waojou.2022.100738
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
